The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in the functioning of the human body. It is responsible for regulating various bodily functions, including heart rate, digestion, and breathing. But what happens when the vagus nerve is cut? This article explores the consequences of cutting the vagus nerve, the medical procedures involving it, recovery and rehabilitation after nerve damage, and future research and developments in this field.
Understanding the Role of the Vagus Nerve
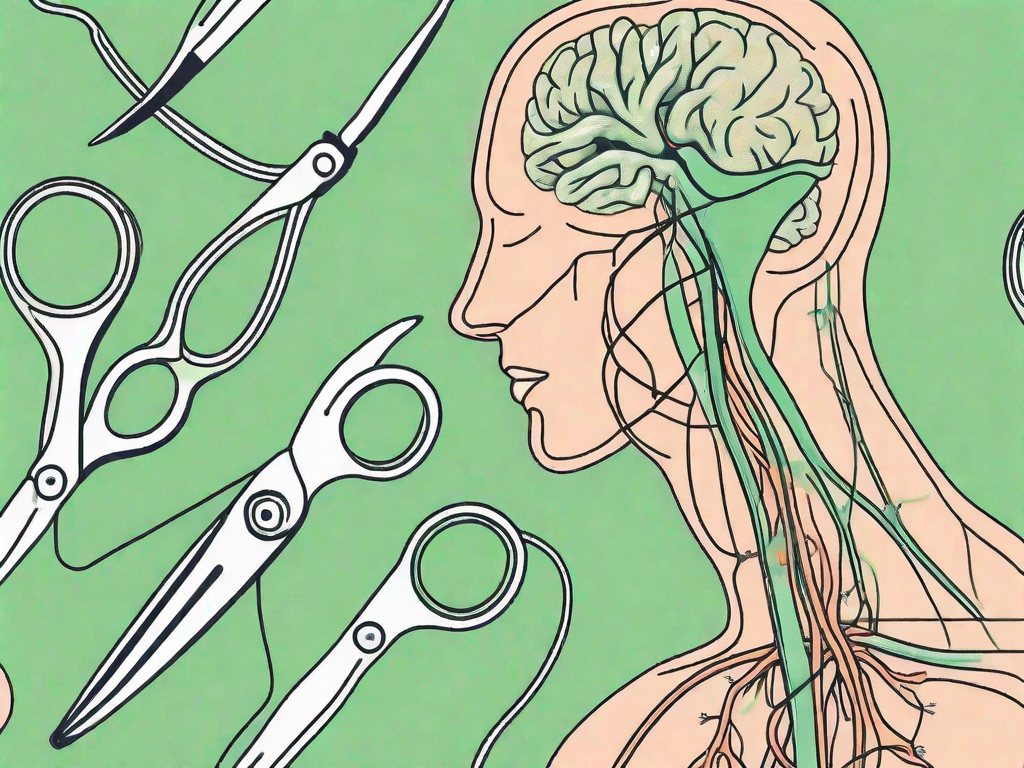
The vagus nerve is a vital component of the autonomic nervous system, which controls involuntary bodily functions. It is the longest cranial nerve, extending from the brainstem to multiple organs in the body. The name “vagus” is derived from the Latin word for “wandering,” highlighting the nerve’s extensive reach.
The vagus nerve is responsible for maintaining the balance between the sympathetic and parasympathetic branches of the autonomic nervous system. While the sympathetic system prepares the body for fight or flight responses, the parasympathetic system promotes rest, relaxation, and digestion. The vagus nerve plays a significant role in activating the parasympathetic response.
The Vagus Nerve and the Autonomic Nervous System
The vagus nerve, along with other components of the autonomic nervous system, helps regulate essential bodily functions without conscious effort. It connects the brain to organs such as the heart, lungs, stomach, and intestines, allowing for seamless communication and coordination.
Through its extensive network of fibers, the vagus nerve carries signals between the brain and various organs, ensuring proper functioning and maintaining homeostasis. It influences heart rate, digestion, sweating, and even the release of certain hormones.
For example, when you eat a delicious meal, the vagus nerve is responsible for stimulating the production of stomach acid and digestive enzymes, ensuring efficient digestion and nutrient absorption. It also plays a crucial role in the regulation of insulin, a hormone that helps control blood sugar levels.
Moreover, the vagus nerve affects the muscles in the throat and voice box, allowing us to speak and swallow effortlessly. It contributes to smooth muscle control in the respiratory system, facilitating the rhythmic expansion and contraction of the lungs during breathing. Additionally, it helps initiate the production of saliva, which aids in the digestion process.
Key Functions of the Vagus Nerve
One of the primary functions of the vagus nerve is controlling heart rate and blood pressure. It sends signals to the heart to slow down or speed up, depending on the body’s needs. This intricate communication between the vagus nerve and the heart ensures that blood is pumped efficiently throughout the body, supplying oxygen and nutrients to all organs and tissues.
Furthermore, the vagus nerve influences our emotional state and mental well-being. It communicates with the brain’s limbic system, which is responsible for regulating emotions, memory, and stress responses. By activating the parasympathetic response, the vagus nerve helps calm the body and mind, promoting relaxation.
Research has shown that stimulating the vagus nerve can have therapeutic effects on various mental health conditions, including anxiety and depression. Techniques such as deep breathing exercises and meditation can activate the vagus nerve, leading to a sense of calm and improved emotional well-being.
In conclusion, the vagus nerve is a remarkable component of the autonomic nervous system, with its extensive reach and crucial role in maintaining bodily functions. From regulating heart rate and digestion to influencing emotions and mental well-being, the vagus nerve plays a vital part in keeping our bodies and minds in balance.
The Impact of Cutting the Vagus Nerve
While the vagus nerve is essential for maintaining bodily functions, there are certain medical conditions that may require cutting or severing the nerve. One such condition is severe epilepsy, where seizures are not adequately controlled by traditional treatments.
However, cutting the vagus nerve can lead to significant consequences, both immediate and long-term. Understanding these effects is crucial for individuals considering vagus nerve procedures and for healthcare professionals managing postoperative care.
Immediate Physical Effects
After the vagus nerve is cut, immediate physical effects can be observed. The heart rate may increase, and blood pressure may elevate as the parasympathetic stimulation is reduced. Digestive processes may become altered since the vagus nerve no longer provides the same level of control.
Furthermore, cutting the vagus nerve can affect swallowing and speech, causing difficulties in these areas. Short-term postoperative pain, swelling, and discomfort are also expected.
On a more detailed note, the increased heart rate and elevated blood pressure after cutting the vagus nerve can be attributed to the sympathetic nervous system taking over. This system is responsible for the body’s “fight or flight” response, which can lead to heightened physiological arousal. However, it is important to note that these effects may vary from person to person.
In terms of digestive processes, the vagus nerve plays a crucial role in regulating the movement of food through the gastrointestinal tract. Cutting the nerve can disrupt this regulation, leading to issues such as delayed stomach emptying, known as gastroparesis. This condition can result in symptoms like nausea, bloating, and abdominal pain.
Moreover, the impact on swallowing and speech can be attributed to the vagus nerve’s involvement in controlling the muscles responsible for these functions. Without its influence, individuals may experience difficulties in these areas, requiring additional therapy and support to regain normal function.
Long-Term Health Implications
The long-term health implications of cutting the vagus nerve can be diverse and depend on various individual factors. Digestive issues, such as gastroparesis (delayed stomach emptying), may arise due to reduced vagus nerve stimulation. This can lead to symptoms like nausea, bloating, and abdominal pain.
Weight gain or loss may also occur as the body’s metabolism and appetite regulation are affected. Since the vagus nerve plays a role in emotional regulation, psychiatric conditions, including anxiety and depression, may become more challenging to manage.
Expanding on the topic of weight regulation, the vagus nerve is responsible for transmitting signals between the stomach and the brain, informing the body about satiety and hunger levels. When the nerve is cut, these signals may be disrupted, leading to imbalances in appetite regulation. Some individuals may experience an increase in appetite, leading to weight gain, while others may experience a decrease in appetite, resulting in weight loss.
Furthermore, the vagus nerve is involved in the regulation of emotional responses and mood. By cutting the nerve, the intricate balance of neurotransmitters and hormones involved in emotional regulation may be disrupted. This disruption can contribute to the development or exacerbation of psychiatric conditions such as anxiety and depression. It is crucial for individuals undergoing vagus nerve procedures to receive comprehensive mental health support to manage these potential challenges.
In conclusion, cutting the vagus nerve can have significant immediate and long-term effects on various bodily functions. From alterations in heart rate and blood pressure to disruptions in digestion, swallowing, and speech, the consequences of this procedure should be carefully considered. Additionally, the long-term implications on weight regulation and emotional well-being highlight the importance of comprehensive postoperative care and support.
Medical Procedures Involving the Vagus Nerve
Several medical procedures involve the vagus nerve, aiming to treat specific conditions or improve overall health. Two prominent procedures are vagus nerve stimulation therapy and vagotomy.
Vagus Nerve Stimulation Therapy
Vagus nerve stimulation therapy involves the implantation of a small device that delivers regular electrical impulses to the vagus nerve. This treatment is primarily used for individuals with epilepsy that is not adequately controlled by medications.
By stimulating the vagus nerve, the therapy may reduce the frequency and severity of seizures. It works by altering the electrical activity in the brain, providing relief for individuals who do not respond to conventional epilepsy treatments.
Risks and Benefits of Vagotomy
Vagotomy is a surgical procedure that involves cutting or removing a portion of the vagus nerve. It is performed to treat conditions such as peptic ulcers or severe gastroparesis when other treatments have proven ineffective.
While vagotomy can alleviate specific conditions, it carries certain risks. Reduced vagus nerve function may result in digestive complications or changes in heart rate and blood pressure regulation. However, for some individuals, the benefits of improved symptom control outweigh the potential risks.
Recovery and Rehabilitation After Vagus Nerve Damage
After the vagus nerve is cut or damaged, recovery and rehabilitation play a crucial role in helping individuals adapt to the changes and regain functionality. Therapeutic approaches and lifestyle adjustments can contribute to postoperative healing.
Therapeutic Approaches for Vagus Nerve Damage
Physical therapy and occupational therapy can assist in regaining strength and function. These therapies focus on restoring mobility, coordination, and muscle control in areas affected by the vagus nerve damage. Additionally, speech therapy may be beneficial for individuals experiencing difficulty with swallowing or speech after the procedure.
Pain management strategies are also essential during the recovery period. Medications or alternative pain relief techniques may be prescribed to alleviate discomfort and support overall well-being.
Lifestyle Adjustments for Living with Vagus Nerve Damage
Living with vagus nerve damage may require certain lifestyle adjustments. Dietary modifications can help manage digestive symptoms, focusing on smaller, frequent meals and specific food choices that are easier to digest.
Individuals should also be aware of their heart rate and blood pressure fluctuations and learn techniques for managing stress and anxiety. Emotional support and counseling can be valuable resources for individuals navigating the challenges associated with vagus nerve damage.
Future Research and Developments
Advancements in medical research and technology continue to explore innovative approaches to vagus nerve treatments and regenerative medicine. These developments offer hope for further improving outcomes and minimizing the impact of vagus nerve damage.
Innovations in Vagus Nerve Treatment
Researchers are investigating novel methods of vagus nerve stimulation, including more precise targeting and personalized therapy. By refining stimulation techniques, the therapeutic benefits may become even more effective while minimizing potential side effects.
Bioelectronic medicine, an emerging field that utilizes electrical impulses to regulate the body’s functions, shows promise in treating conditions by modulating neural circuits such as the vagus nerve. Harnessing the body’s natural neuroregeneration capabilities is also an area of active research.
The Potential of Regenerative Medicine
Regenerative medicine, a rapidly developing field, seeks to restore damaged tissues and organs to their normal state. In the context of the vagus nerve, researchers are exploring strategies to promote nerve regeneration and restore functionality.
Using stem cells, tissue engineering, and other regenerative techniques, scientists are working towards the development of interventions that can repair or replace damaged vagus nerve fibers. While still in the experimental stages, these approaches hold great promise for the future.
As our understanding of the vagus nerve and its intricacies deepens, the medical community can better address the challenges associated with cutting or damaging this essential nerve. By exploring new therapies, rehabilitation techniques, and advancements in regenerative medicine, we strive to improve the quality of life for individuals affected by vagus nerve-related conditions.
Cutting the vagus nerve has significant implications and requires careful consideration. Medical professionals can guide patients through the decision-making process, ensuring adequate informed consent and providing appropriate postoperative care. As research progresses, we hope to enhance current treatment options and pave the way for innovative interventions that harness the power of the vagus nerve to improve human health and well-being.
If you’re fascinated by the critical role the vagus nerve plays in your health and are eager to delve deeper into its functions and how to care for it, “My Vagus Nerve & Me Book” is an invaluable resource. Discover the secrets of one of the most sophisticated systems in the human body, and learn practical ways to stimulate your vagus nerve for improved well-being. From understanding its complex role in your immune system to exploring its impact on your mental health, this book is your guide to harnessing the power of the vagus nerve. Ready to embark on a journey to optimal health? Get My Vagus Nerve & Me eBook today and take the first step towards a deeper understanding of your body’s inner workings.