Vagus nerve inflammation, also known as vaginitis, is a condition that can cause a variety of uncomfortable symptoms. Understanding the triggers of this inflammation is crucial in managing and preventing its occurrence. In this article, we will delve into the factors that can lead to vagus nerve inflammation and explore the science behind it.
Understanding the Vagus Nerve: A Comprehensive Overview
The vagus nerve, also known as cranial nerve X, is an incredibly important and fascinating component of the human body. It is not only one of the longest nerves, but also plays a crucial role in regulating numerous bodily functions. By delving deeper into the intricacies of the vagus nerve, we can gain a profound understanding of its impact on our overall well-being.
The Role and Function of the Vagus Nerve
The vagus nerve, being the longest parasympathetic nerve in the body, acts as a vital communication pathway between the brain and various organs. It facilitates the transmission of signals to and from organs such as the heart, lungs, and digestive tract. This nerve is responsible for controlling the “rest and digest” response, which promotes relaxation, optimal organ function, and efficient digestion.
Furthermore, the vagus nerve is intricately involved in the regulation of inflammation. It helps maintain a delicate balance between pro-inflammatory and anti-inflammatory signals, ensuring appropriate immune responses. When the vagus nerve itself becomes inflamed, this equilibrium is disrupted, potentially leading to a range of health complications.
The Anatomy of the Vagus Nerve
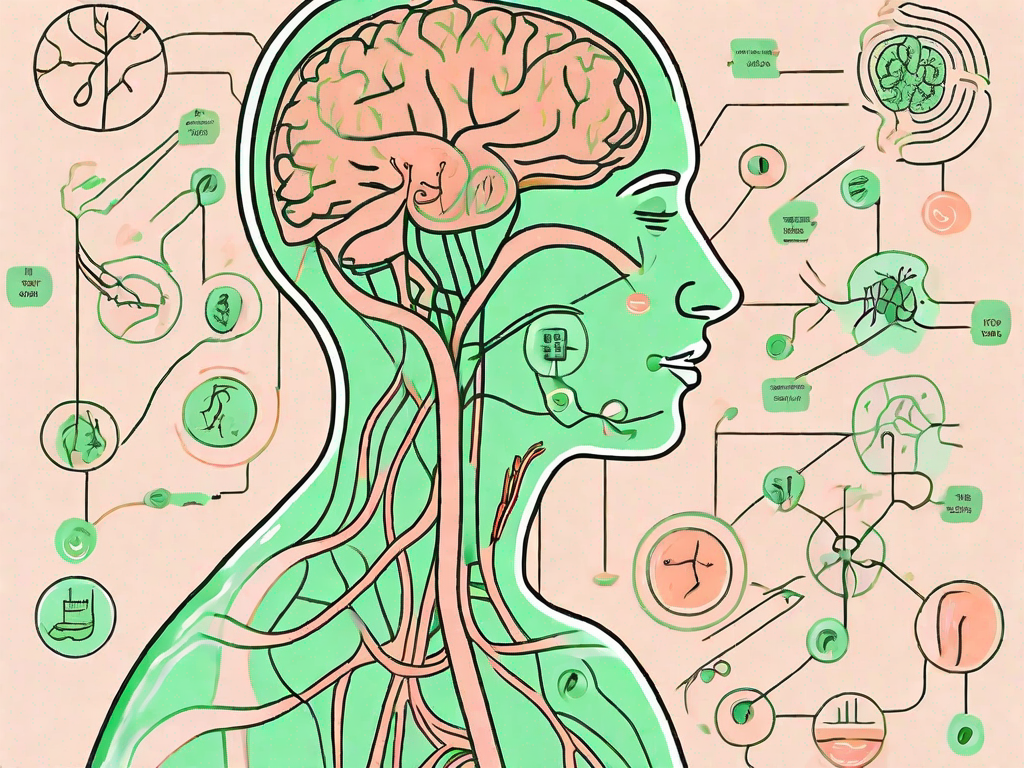
The vagus nerve is a remarkably complex structure that originates in the brainstem and extends down the neck to the chest and abdomen. It consists of both sensory and motor fibers, allowing it to transmit information from various organs to the brain and execute the brain’s responses. Understanding the anatomy of the vagus nerve provides valuable insight into the potential points of inflammation and the associated symptoms.
Within the brainstem, the vagus nerve emerges from the medulla oblongata, a crucial part of the brain responsible for controlling vital functions such as breathing and heart rate. From there, it branches out and travels through the neck, sending branches to the larynx, pharynx, and tongue, contributing to speech and swallowing. As it continues its journey, the vagus nerve reaches the chest and abdomen, where it innervates organs such as the heart, lungs, stomach, and intestines.
It is important to note that the vagus nerve is not a single entity, but rather a complex network of fibers. These fibers are divided into two main components: the sensory fibers, which transmit information from the organs to the brain, and the motor fibers, which carry signals from the brain to the organs, enabling them to function optimally.
By understanding the intricate details of the vagus nerve, we can appreciate its immense significance in maintaining our overall health and well-being. From regulating heart rate and digestion to modulating inflammation, this remarkable nerve truly deserves our attention and admiration.
The Science Behind Vagus Nerve Inflammation
To comprehend the causes of vagus nerve inflammation, it is essential to grasp the biological process of inflammation and how it affects this crucial nerve.
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It originates in the brainstem and extends down to various organs in the body, including the heart, lungs, and digestive system. Its primary function is to regulate many essential bodily functions, such as heart rate, digestion, and immune response.
The Biological Process of Inflammation
Inflammation is the body’s natural response to injury, infection, or irritation. It is a complex process involving various immune cells, chemical signals, and molecular pathways. When tissue damage occurs, the body releases chemical signals, such as cytokines and prostaglandins, which attract immune cells to the affected area.
These immune cells, including neutrophils and macrophages, help eliminate pathogens, clear debris, and initiate the healing process. Inflammation is characterized by redness, swelling, heat, and pain, which are all signs of increased blood flow and immune cell activity in the area.
While inflammation is usually a protective response, chronic inflammation can be detrimental to the nerves, including the vagus nerve. Chronic inflammation can damage the nerve fibers and interfere with their ability to transmit signals effectively. This disruption can manifest in various symptoms, depending on the location and severity of the inflammation.
For example, if the vagus nerve is inflamed near the heart, it may lead to heart rhythm abnormalities. If the inflammation occurs in the gastrointestinal tract, it can cause digestive issues such as abdominal pain, bloating, and altered bowel movements. Inflammation near the respiratory system can result in breathing difficulties and respiratory disorders.
How Inflammation Affects the Vagus Nerve
When the vagus nerve becomes inflamed, its ability to regulate bodily functions and control inflammation itself is compromised. This can lead to a range of symptoms, including gastrointestinal issues, heart rhythm abnormalities, and respiratory difficulties.
Furthermore, inflammation of the vagus nerve can disrupt the balance between pro-inflammatory and anti-inflammatory signals, leading to heightened immune responses and further inflammation. The vagus nerve plays a crucial role in the “cholinergic anti-inflammatory pathway,” which helps dampen excessive inflammation in the body.
However, when the vagus nerve is inflamed, this pathway may become dysregulated, resulting in an overactive immune response and chronic inflammation. This vicious cycle of inflammation and nerve damage can be challenging to break without identifying and addressing the underlying triggers.
It is important to note that vagus nerve inflammation can be caused by various factors, including autoimmune diseases, infections, trauma, and chronic stress. Identifying the root cause of the inflammation is crucial for developing an effective treatment plan.
In conclusion, understanding the science behind vagus nerve inflammation involves comprehending the biological process of inflammation and how it affects the intricate functions of this vital nerve. Chronic inflammation can disrupt the vagus nerve’s ability to regulate bodily functions and control inflammation itself, leading to a wide range of symptoms and a dysregulated immune response. Further research is needed to unravel the complex mechanisms underlying vagus nerve inflammation and develop targeted therapies to alleviate its effects.
Common Triggers of Vagus Nerve Inflammation
Vagus nerve inflammation can be triggered by various factors, both physical and emotional. Understanding and recognizing these triggers are crucial steps in managing and preventing inflammation episodes.
Physical Triggers: Injuries and Illnesses
Injury or trauma to the head, neck, or chest area can directly affect the vagus nerve and trigger inflammation. Additionally, certain illnesses, such as viral or bacterial infections, can indirectly cause inflammation of the nerve.
It is important to seek appropriate medical care for injuries and infections to reduce the risk of vagus nerve inflammation and its associated complications.
Emotional and Psychological Triggers
Emotional and psychological factors can also contribute to vagus nerve inflammation. Stress, anxiety, and depression can disrupt the body’s immune response and increase inflammation levels.
Adopting stress management techniques, seeking therapy or counseling, and ensuring a healthy work-life balance can help minimize emotional triggers and reduce the risk of vagus nerve inflammation episodes.
Symptoms and Diagnosis of Vagus Nerve Inflammation
Recognizing the symptoms of vagus nerve inflammation is crucial for early diagnosis and effective treatment. While the presentation may vary among individuals, certain common symptoms can indicate possible nerve inflammation.
Recognizing the Symptoms
Some common symptoms of vagus nerve inflammation include dizziness, irregular heart rate, difficulty swallowing, gastrointestinal disturbances, and shortness of breath. These symptoms can range from mild discomfort to severe distress, affecting the quality of life for those experiencing them.
If you suspect vagus nerve inflammation, it is essential to consult with a healthcare professional who can accurately diagnose the condition based on your medical history, symptoms, and physical examination.
Diagnostic Procedures for Vagus Nerve Inflammation
To confirm a suspected diagnosis of vagus nerve inflammation, your healthcare provider may recommend various diagnostic procedures. These may include imaging tests, such as MRI or CT scans, nerve conduction studies, and blood tests to assess inflammation markers.
Accurate diagnosis is crucial for developing a personalized treatment plan and managing the symptoms effectively.
Treatment Options for Vagus Nerve Inflammation
Managing and treating vagus nerve inflammation involves a comprehensive approach that combines medical treatments, procedures, and lifestyle changes.
Medical Treatments and Procedures
Depending on the severity and underlying cause of vagus nerve inflammation, your healthcare provider may prescribe medications to reduce inflammation, relieve symptoms, or manage underlying conditions contributing to nerve inflammation.
In certain cases, specialized procedures, such as nerve blocks, electrical nerve stimulation, or surgical interventions, may be recommended to alleviate symptoms and restore normal nerve function.
Lifestyle Changes and Home Remedies
Complementary to medical treatments, adopting lifestyle changes can significantly contribute to managing and preventing vagus nerve inflammation episodes. These may include stress management techniques, regular exercise, a balanced diet, and adequate sleep.
Additionally, incorporating relaxation practices, such as deep breathing exercises and meditation, can help improve vagus nerve function and reduce inflammation.
Conclusion
Understanding the triggers of vagus nerve inflammation is essential in managing and preventing this condition. By comprehending the role of the vagus nerve, the science behind inflammation, and the common triggers, individuals can take proactive steps to reduce the risk of inflammation and its associated symptoms.
Remember, if you suspect vagus nerve inflammation, consult with a healthcare professional for accurate diagnosis and personalized treatment options. With the right approach, it is possible to regain control over your health and well-being.