The vagus nerve is an essential part of the body’s nervous system. It plays a vital role in regulating many bodily functions, including heart rate, digestion, and breathing. When the vagus nerve becomes aggravated, it can lead to a variety of uncomfortable symptoms and medical conditions. Understanding what aggravates the vagus nerve is crucial in finding effective solutions. Let’s explore the anatomy and function of the vagus nerve, common symptoms and medical conditions associated with its aggravation, as well as the causes and potential solutions for this issue.
Understanding the Vagus Nerve
Anatomy and Function of the Vagus Nerve
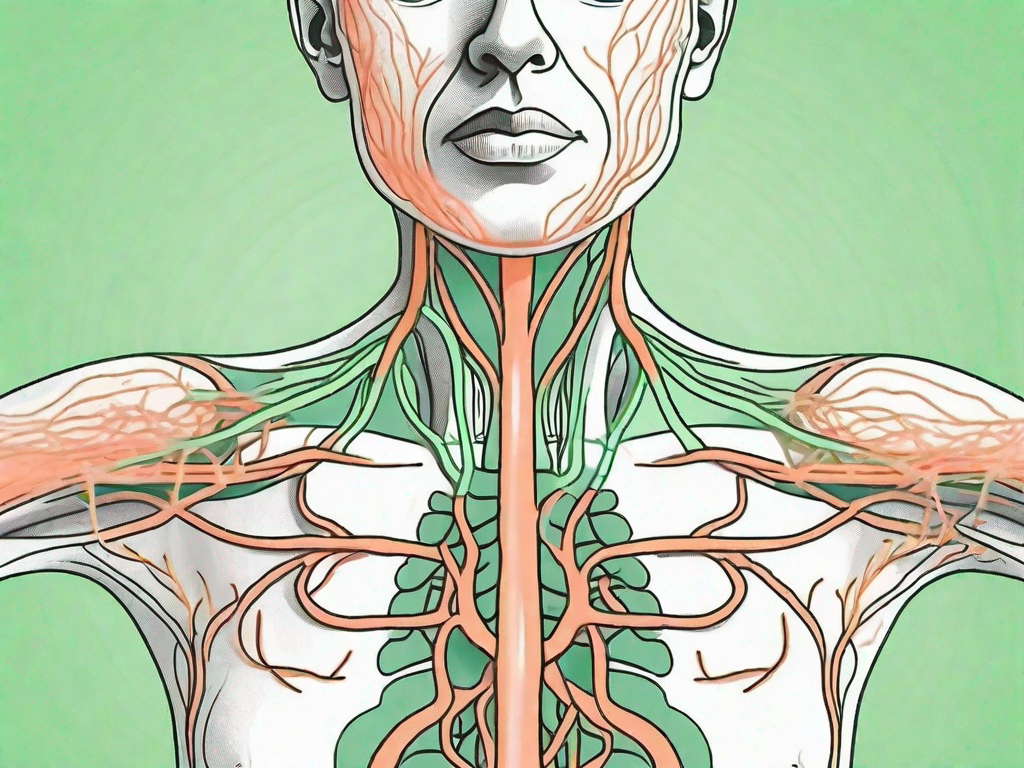
The vagus nerve, also known as the tenth cranial nerve, is the longest cranial nerve in the body. It extends from the brain stem to various organs in the body, including the heart, lungs, stomach, and intestines. The vagus nerve consists of both sensory and motor fibers, allowing it to transmit signals between the brain and these organs.
Functionally, the vagus nerve plays a crucial role in regulating the parasympathetic nervous system, which is responsible for rest and digestion. It helps to slow down the heart rate, stimulate digestion, promote relaxation, and control inflammation. The vagus nerve is also involved in the body’s stress response, helping to reduce anxiety and promote a sense of calmness.
When it comes to the anatomy of the vagus nerve, it is fascinating to note that it is not a single nerve but a complex network of fibers. These fibers branch out and innervate various organs, allowing for precise control and coordination. The vagus nerve’s extensive reach and connectivity make it a vital component of the autonomic nervous system, which regulates involuntary bodily functions.
Moreover, the vagus nerve is not limited to its role in the parasympathetic nervous system. It has far-reaching effects on other bodily functions as well. For instance, the vagus nerve influences the release of certain chemicals in the brain, including serotonin and acetylcholine. Serotonin is a neurotransmitter known for its role in mood regulation, while acetylcholine is involved in memory and learning. Thus, the vagus nerve’s activity can impact our emotional well-being and cognitive abilities.
Another intriguing aspect of the vagus nerve is its communication with the gut microbiota. The gut microbiota refers to the community of microorganisms residing in our digestive system. Research has shown that the vagus nerve plays a crucial role in maintaining a healthy balance of beneficial bacteria in the gut. This communication between the vagus nerve and the gut microbiota highlights the intricate connection between our nervous system and the microorganisms that inhabit our bodies.
The Role of the Vagus Nerve in the Body
Aside from its role in regulating the parasympathetic nervous system, the vagus nerve is involved in several other bodily functions. It influences the release of certain chemicals in the brain, including serotonin and acetylcholine, which play a role in mood regulation, memory, and learning. The vagus nerve also communicates with the gut microbiota, affecting the balance of beneficial bacteria in the digestive system.
Furthermore, the vagus nerve has been found to have an impact on inflammation in the body. It possesses anti-inflammatory properties and can help regulate the immune response. By modulating inflammation, the vagus nerve aids in maintaining a healthy immune system and preventing chronic inflammatory conditions.
Additionally, the vagus nerve is involved in the regulation of heart rate variability (HRV). HRV refers to the variation in time intervals between consecutive heartbeats. A higher HRV is generally associated with better cardiovascular health and overall well-being. The vagus nerve’s influence on HRV highlights its role in maintaining a healthy heart and cardiovascular system.
Moreover, recent studies have shown that the vagus nerve may have a role in pain modulation. It has been found that stimulating the vagus nerve can help alleviate chronic pain conditions, such as migraines and fibromyalgia. This discovery opens up new possibilities for non-pharmacological pain management techniques.
In conclusion, the vagus nerve is a remarkable component of our nervous system, with far-reaching effects on various bodily functions. Its intricate network of fibers allows for precise control and coordination, influencing everything from heart rate and digestion to mood regulation and pain modulation. Understanding the vagus nerve’s anatomy and function provides valuable insights into the complex interplay between our brain, body, and overall well-being.
Identifying Vagus Nerve Aggravation
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions. When this nerve becomes aggravated, it can manifest in various symptoms that can greatly impact an individual’s well-being.
Common Symptoms of Vagus Nerve Aggravation
When the vagus nerve is aggravated, it can give rise to a range of distressing symptoms. One of the most common symptoms is dizziness, which can make it difficult for individuals to maintain their balance and perform daily activities. Lightheadedness is another prevalent symptom, causing individuals to feel a sense of unsteadiness or faintness.
In some cases, vagus nerve aggravation can lead to fainting, a sudden and temporary loss of consciousness. This can be a frightening experience for those affected and may require medical attention to determine the underlying cause.
Rapid heart rate, also known as tachycardia, is another symptom that can occur when the vagus nerve is aggravated. This can cause individuals to feel their heart pounding or racing, which can be accompanied by feelings of anxiety or discomfort.
The digestive system can also be affected by vagus nerve aggravation. Individuals may experience symptoms such as nausea and vomiting, which can greatly impact their quality of life. Difficulty swallowing, known as dysphagia, can also occur, making it challenging for individuals to consume food and liquids comfortably.
Some individuals may notice excessive sweating when their vagus nerve is aggravated. This can be particularly bothersome and may occur even in situations where sweating is not typically expected, such as during periods of rest or relaxation.
In addition, chest pain can be a symptom of vagus nerve aggravation. This can be a cause for concern, as chest pain can be associated with various medical conditions, including heart problems. It is important to seek medical evaluation to determine the underlying cause of chest pain and ensure appropriate treatment.
Changes in blood pressure can also occur when the vagus nerve is aggravated. Some individuals may experience a sudden drop in blood pressure, leading to feelings of lightheadedness or fainting. Others may experience an increase in blood pressure, which can have its own set of health implications.
It’s important to note that vagus nerve aggravation can present differently in each individual, so symptoms may vary. It is always recommended to consult with a healthcare professional for an accurate diagnosis and appropriate management of symptoms.
Medical Conditions Related to Vagus Nerve Aggravation
The aggravation of the vagus nerve can be associated with certain medical conditions. One such condition is gastroparesis, a disorder characterized by delayed stomach emptying. This can lead to symptoms such as bloating, abdominal discomfort, nausea, and vomiting. Individuals with gastroparesis may experience difficulties in digesting food properly, which can significantly impact their nutritional intake and overall well-being.
Arrhythmias, which are abnormal heart rhythms, can also be linked to vagus nerve aggravation. The vagus nerve plays a role in regulating the heart rate, and when it becomes aggravated, it can disrupt the normal electrical signals that control the heart’s rhythm. This can result in irregular heartbeats, palpitations, and other symptoms associated with arrhythmias.
Gastroesophageal reflux disease (GERD) is another medical condition that may be related to vagus nerve aggravation. This chronic condition occurs when stomach acid flows back into the esophagus, causing symptoms such as heartburn, chest pain, and regurgitation. The vagus nerve is involved in the regulation of the lower esophageal sphincter, which helps prevent the backflow of stomach acid. When the vagus nerve is aggravated, it can contribute to the dysfunction of this sphincter, leading to the development or worsening of GERD symptoms.
Chronic inflammatory conditions, such as rheumatoid arthritis and inflammatory bowel disease, have also been associated with vagus nerve aggravation. Inflammation plays a significant role in these conditions, and the vagus nerve, as part of the body’s inflammatory response system, can become activated and aggravated in the presence of chronic inflammation. This can further contribute to the symptoms experienced by individuals with these conditions.
Understanding the relationship between vagus nerve aggravation and these medical conditions can help healthcare professionals develop more effective treatment strategies and improve the overall management of symptoms.
Causes of Vagus Nerve Aggravation
Lifestyle Factors that Aggravate the Vagus Nerve
Several lifestyle factors can contribute to vagus nerve aggravation. Chronic stress, lack of sleep, poor dietary choices, excessive alcohol consumption, and sedentary behavior can all affect the function of the vagus nerve. Stress, in particular, has a significant impact on the vagus nerve, as it activates the body’s fight-or-flight response and inhibits the parasympathetic nervous system’s function.
Medical Conditions that Aggravate the Vagus Nerve
In addition to lifestyle factors, certain medical conditions can exacerbate vagus nerve aggravation. Conditions such as diabetes, autoimmune diseases, thyroid disorders, and heart diseases can disrupt the normal functioning of the vagus nerve. Additionally, gastrointestinal disorders like irritable bowel syndrome (IBS) and conditions that cause nerve compression, such as herniated discs, can also contribute to the aggravation of the vagus nerve.
Diagnosing Vagus Nerve Aggravation
Medical Tests for Vagus Nerve Aggravation
If you suspect vagus nerve aggravation, it’s essential to seek proper medical evaluation. A healthcare professional can perform various tests to assess its function. These may include autonomic function tests, electrocardiograms (ECG), gastroenterological tests, and imaging studies like MRI or CT scans. These tests can help identify any underlying medical conditions and determine the extent of vagus nerve aggravation.
Understanding Your Diagnosis
Once a diagnosis of vagus nerve aggravation is confirmed, it’s important to understand the implications and potential treatment options. Your healthcare provider will be able to explain the causes behind the aggravation and discuss appropriate treatment plans. Remember, each individual may have unique factors contributing to their vagus nerve aggravation, so treatment approaches can vary.
Solutions for Vagus Nerve Aggravation
Medical Treatments for Vagus Nerve Aggravation
In severe cases, medical interventions may be necessary to alleviate vagus nerve aggravation. These can include medications to manage symptoms such as antiemetics for nausea or antianxiety medications for stress-related symptoms. In some cases, surgical procedures or nerve stimulation techniques may be recommended by a healthcare professional.
Natural Remedies for Vagus Nerve Aggravation
For milder cases or as complementary therapies, there are natural remedies that can help soothe the vagus nerve. Deep breathing exercises, yoga, meditation, and mindfulness techniques can all promote relaxation and stimulate the vagus nerve’s function. Ensuring adequate sleep, maintaining a healthy diet, and engaging in regular physical activity are also beneficial in managing vagus nerve aggravation.
In conclusion, understanding what aggravates the vagus nerve is crucial in finding effective solutions. By recognizing the symptoms, identifying potential causes, seeking appropriate medical evaluation, and exploring various treatment options, individuals can better manage vagus nerve aggravation. Whether through medical treatments or natural remedies, prioritizing the health of the vagus nerve can contribute to overall well-being and improved quality of life.
If you’re fascinated by the remarkable capabilities of the vagus nerve and its profound impact on your health, “My Vagus Nerve & Me Book” is the perfect resource to deepen your understanding. Discover the secrets of this intricate system that governs everything from your heart rate to your digestion, and learn practical ways to stimulate your vagus nerve for optimal well-being. Whether you’re interested in natural or artificial methods, this book covers it all, including its role in immune function, mental health, and vital organ support. Don’t miss out on the opportunity to unlock the full potential of your vagus nerve. Get My Vagus Nerve & Me eBook today and take the first step towards a healthier, more harmonious life.