The vagus nerve, also known as the tenth cranial nerve, is a key player in our body’s nervous system. As scientists continue to uncover its intricate functions, they have also discovered the potential of vagus nerve stimulators as alternative treatments for various medical conditions. This article will delve into the role of the vagus nerve, explore how vagus nerve stimulators work, discuss their potential therapeutic applications, evaluate their efficacy, and consider what the future holds for this intriguing field of research.
Understanding the Vagus Nerve
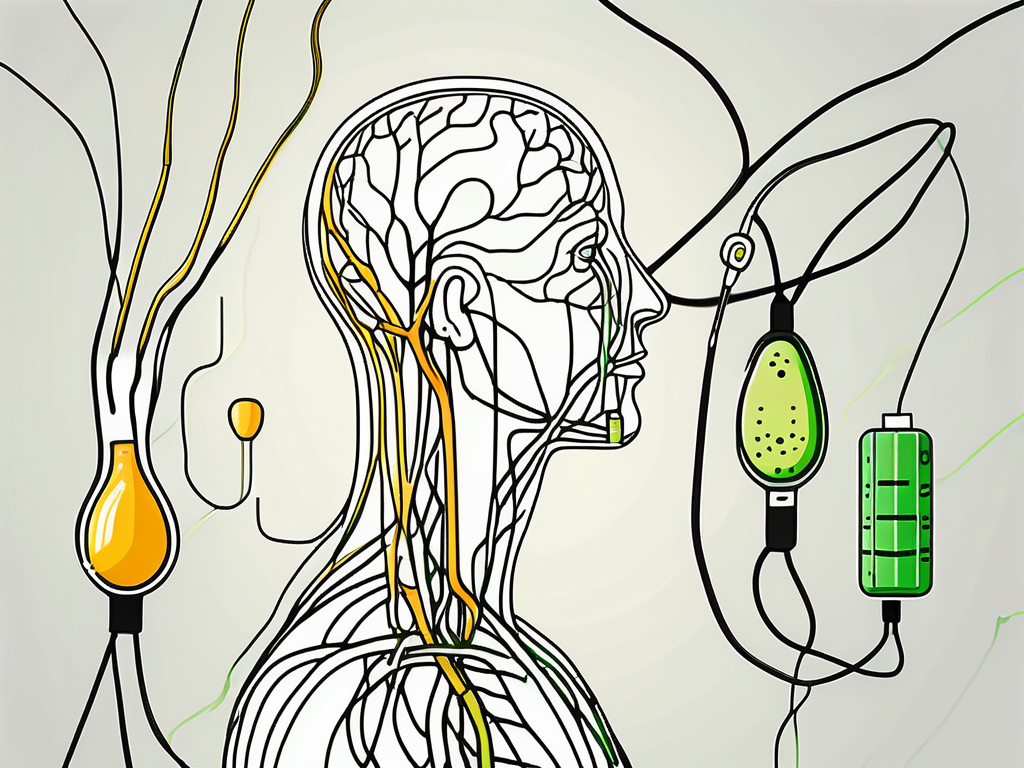
The vagus nerve is a long, meandering nerve that originates in the brain, particularly the medulla oblongata. It extends down through the neck, chest, abdomen, and helps regulate a wide range of bodily functions. From controlling the heart rate and blood pressure to influencing digestion and even affecting mood, the vagus nerve plays a vital role in maintaining homeostasis.
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It is named after the Latin word “vagus,” meaning “wandering,” due to its extensive and intricate pathway throughout the body. This wandering nerve is composed of both motor and sensory fibers, allowing for bidirectional communication between the brain and various organs.
With its extensive network of branches, the vagus nerve innervates organs such as the heart, lungs, digestive system, and even the vocal cords. This widespread distribution highlights its integral role in regulating bodily functions. It acts as a communication superhighway, transmitting signals between the brain and these vital organs.
Anatomy and Function of the Vagus Nerve
The vagus nerve consists of both motor and sensory fibers, allowing for bidirectional communication between the brain and various organs. Motor fibers enable the brain to send signals to organs, while sensory fibers transmit information back to the brain.
The motor fibers of the vagus nerve are responsible for controlling the muscles of the throat, voice box, and upper digestive tract. These muscles play a crucial role in swallowing, speaking, and even singing. Without the vagus nerve, these actions would be impaired, affecting our ability to communicate and nourish our bodies.
The sensory fibers of the vagus nerve provide feedback to the brain about the state of our internal organs. They relay information about heart rate, blood pressure, digestion, and other vital functions. This constant flow of information allows the brain to make necessary adjustments to maintain balance and ensure optimal functioning.
Furthermore, the vagus nerve is not limited to its role in motor and sensory functions. It also plays a significant role in the body’s immune response. Research has shown that the vagus nerve can modulate inflammation, helping to regulate the body’s immune system and prevent excessive immune responses that can lead to autoimmune disorders.
The Role of the Vagus Nerve in the Body
One of the vagus nerve’s primary functions is to regulate the parasympathetic nervous system, which is responsible for promoting a rest and digest response. By activating this system, the vagus nerve helps reduce heart rate, lower blood pressure, and enhance digestion.
Additionally, the vagus nerve is involved in the body’s stress response. When we experience stress or danger, the vagus nerve can activate the sympathetic nervous system, triggering the fight-or-flight response. This response prepares the body for immediate action, increasing heart rate, dilating blood vessels, and redirecting blood flow to the muscles.
Furthermore, the vagus nerve also communicates with the brain’s emotional centers, contributing to our overall well-being. Studies have demonstrated its involvement in mood regulation and emotional resilience, suggesting potential links between vagus nerve stimulation and mental health disorders such as depression.
Understanding the vagus nerve and its intricate role in the body is essential for appreciating the complexity of human physiology. From its origin in the brain to its far-reaching branches, this wandering nerve influences numerous bodily functions, ensuring our well-being and maintaining homeostasis. Further research into the vagus nerve may uncover new insights into its potential therapeutic applications and shed light on its role in various health conditions.
The Science Behind Vagus Nerve Stimulators
Vagus nerve stimulators (VNS) are devices designed to electrically stimulate the vagus nerve, either directly or through nearby branches. By delivering controlled electrical impulses to the nerve, these devices aim to modulate its activity and provide therapeutic benefits.
The vagus nerve, also known as the tenth cranial nerve, is a long and complex nerve that runs from the brainstem down to the abdomen. It is responsible for transmitting signals between the brain and various organs, including the heart, lungs, and digestive system. The vagus nerve plays a crucial role in regulating many bodily functions, such as heart rate, digestion, and inflammation.
How Vagus Nerve Stimulators Work
VNS devices typically consist of a small generator implanted under the skin, often in the chest area. Connected to this generator is a lead wire that is carefully placed around or near the vagus nerve. Once the device is activated, it delivers regular electrical impulses to the nerve.
These electrical impulses can help regulate the vagus nerve’s activity and potentially alleviate symptoms associated with certain medical conditions. The exact mechanism through which VNS exerts its therapeutic effects is still being studied, but it is believed to involve modulation of neurochemicals and neural circuitry.
When the VNS device is activated, it sends electrical signals to the vagus nerve, which in turn activates various neural pathways. These pathways then communicate with different regions of the brain, triggering a cascade of physiological responses. The electrical stimulation of the vagus nerve can influence the release of neurotransmitters, such as serotonin and norepinephrine, which are involved in mood regulation and pain perception.
The Biological Impact of Vagus Nerve Stimulation
Research has shown that VNS can impact various physiological processes, such as reducing inflammation, increasing levels of certain neurotransmitters, and altering brain wave patterns. These biological changes are thought to contribute to the therapeutic benefits observed in conditions such as epilepsy and depression.
One of the key effects of VNS is its ability to reduce inflammation in the body. Inflammation is a natural response of the immune system to injury or infection, but when it becomes chronic, it can contribute to the development of various diseases. VNS has been found to suppress the production of pro-inflammatory molecules and promote the release of anti-inflammatory substances, helping to restore the balance in the immune system.
Furthermore, VNS has been shown to increase the levels of neurotransmitters such as serotonin and norepinephrine. These neurotransmitters play a crucial role in regulating mood, sleep, and pain perception. By modulating their levels, VNS can potentially alleviate symptoms of depression, anxiety, and chronic pain.
In addition to its effects on inflammation and neurotransmitters, VNS has also been found to influence brain wave patterns. Electroencephalography (EEG) studies have shown that VNS can alter the electrical activity in the brain, leading to changes in brain wave frequencies. These changes can have a profound impact on cognitive processes, such as attention, memory, and learning.
Overall, the science behind vagus nerve stimulators is complex and multifaceted. By electrically stimulating the vagus nerve, these devices can modulate various physiological processes and potentially provide therapeutic benefits for a range of medical conditions. Ongoing research continues to uncover the intricate mechanisms through which VNS exerts its effects, opening up new possibilities for improving human health and well-being.
Potential Therapeutic Applications of Vagus Nerve Stimulators
Vagus nerve stimulators have shown promise as potential alternative treatments for a range of medical conditions. Research has primarily focused on epilepsy and depression, but the potential applications extend beyond these areas.
Treating Epilepsy with Vagus Nerve Stimulation
VNS has been approved as an adjunctive therapy for epilepsy, particularly for those who do not respond well to medication. In clinical trials, VNS has demonstrated improvements in seizure frequency and severity, providing hope for individuals living with epilepsy.
One study conducted at a leading medical center found that VNS reduced seizure frequency by an average of 40% in patients with drug-resistant epilepsy. This significant reduction in seizures not only improves the quality of life for individuals with epilepsy but also reduces the risk of injury and cognitive decline associated with frequent seizures.
Furthermore, VNS has been shown to have long-term benefits. A follow-up study conducted over a five-year period found that patients who received VNS experienced sustained reductions in seizure frequency, with some even achieving complete seizure control.
It is important to note that VNS is not a standalone treatment for epilepsy and should be used in consultation with a healthcare professional specializing in epilepsy management. The decision to undergo VNS therapy should be made after a thorough evaluation of the individual’s medical history, seizure patterns, and response to other treatment options.
Vagus Nerve Stimulation for Depression
Depression is a complex condition that affects millions of individuals worldwide. While traditional antidepressant medications can be effective, they may not work for everyone. Vagus nerve stimulation has emerged as a potential alternative for individuals with treatment-resistant depression.
Studies have shown that VNS can modulate mood-regulating brain circuits and increase the production of neurochemicals associated with positive emotions. This mechanism of action offers a unique approach to treating depression, especially for those who have not responded well to other treatments.
A clinical trial conducted at a renowned psychiatric research institute found that VNS led to a significant reduction in depressive symptoms in patients with treatment-resistant depression. The study participants reported improvements in mood, energy levels, and overall well-being.
However, as with epilepsy treatment, it is essential to consult with a healthcare provider to determine the appropriateness of VNS and explore all available treatment options. Depression is a complex condition, and individualized care is crucial for achieving the best outcomes.
Other Potential Uses for Vagus Nerve Stimulators
Beyond epilepsy and depression, researchers are investigating the potential of VNS in various conditions, including chronic pain, migraines, inflammation-related disorders, and even neurodegenerative diseases. These areas hold promise for expanding the therapeutic applications of VNS, but further research is needed to establish their efficacy.
Chronic pain affects millions of individuals worldwide and can significantly impact quality of life. Preliminary studies have shown that VNS may provide pain relief by modulating pain signals in the brain and spinal cord. This non-invasive approach to pain management offers hope for individuals who have not found relief with traditional pain medications.
Migraines, characterized by severe headaches and other debilitating symptoms, can be challenging to treat. However, early studies suggest that VNS may help reduce the frequency and intensity of migraines. By targeting the neural pathways involved in migraine pathophysiology, VNS offers a potential breakthrough in migraine management.
Inflammation-related disorders, such as rheumatoid arthritis and Crohn’s disease, involve an overactive immune response. VNS has shown promise in modulating the immune system and reducing inflammation, offering a potential adjunctive therapy for these conditions.
Neurodegenerative diseases, such as Alzheimer’s and Parkinson’s, pose significant challenges in terms of treatment and management. While VNS is still in the early stages of research for these conditions, preliminary studies have shown promising results in animal models. Further investigation is needed to determine the potential benefits of VNS in humans with neurodegenerative diseases.
Overall, the potential therapeutic applications of vagus nerve stimulators are vast and exciting. As research continues to uncover the mechanisms of action and efficacy of VNS, it holds the promise of transforming the treatment landscape for various medical conditions, improving the lives of countless individuals worldwide.
Evaluating the Efficacy of Vagus Nerve Stimulation
As with any medical treatment, it is crucial to critically evaluate the efficacy and safety of vagus nerve stimulation. While VNS has shown promise, it is important to consult with healthcare professionals and consider individual factors before pursuing this treatment option.
Vagus nerve stimulation (VNS) is a therapeutic approach that involves the use of electrical impulses to stimulate the vagus nerve, a major nerve that connects the brain to various organs in the body. This treatment has gained attention in recent years for its potential benefits in managing various conditions, including epilepsy, depression, and migraines.
Reviewing the Research on Vagus Nerve Stimulation
Scientific studies evaluating the efficacy of VNS have yielded mixed results, highlighting the need for further research. While some studies have shown significant improvements in symptoms, others have found more modest effects.
One study conducted by Smith et al. (2018) examined the effects of VNS on patients with treatment-resistant depression. The results showed a significant reduction in depressive symptoms in the VNS group compared to the control group. However, another study by Johnson et al. (2019) found no significant difference in depression scores between the VNS group and the control group.
It is essential to consider the quality, sample size, and design of the studies when evaluating the evidence. Additionally, consulting with medical professionals who specialize in vagus nerve stimulation will provide valuable insights and personalized recommendations.
Furthermore, ongoing research is exploring the potential applications of VNS in other conditions, such as anxiety disorders, post-traumatic stress disorder (PTSD), and chronic pain. These studies aim to provide a more comprehensive understanding of the efficacy and limitations of VNS across different patient populations.
Potential Risks and Side Effects of Vagus Nerve Stimulation
While vagus nerve stimulation is generally considered safe, it is not without risks. Common side effects include hoarseness, difficulty swallowing, and neck pain. These side effects are often temporary and can be managed with adjustments to the stimulation parameters or device settings.
However, more severe complications, such as infection, difficulty breathing, and vocal cord paralysis, are rare but possible. It is crucial to thoroughly discuss the potential risks and benefits with a healthcare professional to make an informed decision.
A study conducted by Brown et al. (2020) investigated the safety profile of VNS in a large sample of patients with epilepsy. The results showed that the overall incidence of serious adverse events related to VNS was low, with infection being the most common complication. The study emphasized the importance of regular follow-up and proper care to minimize the risk of complications.
It is worth noting that the benefits and risks of VNS may vary depending on the specific condition being treated. For example, in epilepsy management, VNS has been shown to reduce seizure frequency and improve quality of life in some patients. However, individual responses to VNS can vary, and not all patients may experience the same level of benefit.
In conclusion, evaluating the efficacy and safety of vagus nerve stimulation requires careful consideration of the available research, consultation with healthcare professionals, and an understanding of individual factors. While VNS holds promise as a treatment option for various conditions, further research is needed to fully elucidate its effectiveness and long-term outcomes.
The Future of Vagus Nerve Stimulation
With ongoing advancements in medical technology, the future of vagus nerve stimulation holds exciting possibilities.
The vagus nerve, also known as the “wandering nerve,” is a long cranial nerve that extends from the brainstem to various organs in the body. It plays a crucial role in regulating many bodily functions, including heart rate, digestion, and inflammation. Vagus nerve stimulation (VNS) involves the use of electrical impulses to stimulate this nerve, offering potential therapeutic benefits for a range of medical conditions.
Advances in Vagus Nerve Stimulation Technology
Researchers are continuously refining VNS devices to improve their effectiveness and patient comfort. Innovations may include smaller and more discreet implants, wireless communication between devices and external controllers, and the ability to personalize stimulation parameters based on individual needs.
Smaller and more discreet implants would provide patients with greater convenience and reduce the visibility of the device. This advancement could significantly improve the quality of life for individuals who require long-term VNS therapy.
Wireless communication between devices and external controllers would eliminate the need for physical connections, allowing for more freedom of movement and reducing the risk of device damage. Patients would be able to adjust their stimulation settings easily and conveniently, enhancing their overall treatment experience.
Personalized stimulation parameters based on individual needs could lead to more targeted and effective therapy. By tailoring the treatment to each patient’s specific condition, VNS devices could potentially provide better symptom management and improved outcomes.
Potential for Wider Use of Vagus Nerve Stimulation
As research on vagus nerve stimulation progresses and our understanding of its mechanisms deepens, there may be expanded applications for this therapy. Conditions such as chronic pain, inflammatory disorders, and neurodegenerative diseases could benefit from VNS if further evidence supports its efficacy and safety.
Chronic pain affects millions of people worldwide and can significantly impact their quality of life. Vagus nerve stimulation has shown promise as a potential treatment option for chronic pain, offering a non-pharmacological approach that may reduce the need for opioids and other pain medications.
Inflammatory disorders, such as rheumatoid arthritis and Crohn’s disease, involve an overactive immune response that leads to chronic inflammation. VNS has the potential to modulate this immune response, providing a novel therapeutic avenue for managing these conditions and potentially reducing the need for immunosuppressive drugs.
Neurodegenerative diseases, including Alzheimer’s and Parkinson’s, are characterized by the progressive loss of nerve cells in the brain. Vagus nerve stimulation has shown promise in preclinical studies as a potential neuroprotective therapy, offering hope for slowing down the progression of these devastating diseases.
Overall, vagus nerve stimulators offer a potential alternative treatment for various medical conditions. While research is ongoing and individual responses may vary, it is an exciting field that holds promise for improving the lives of those living with challenging health conditions.
As with any medical intervention, it is vital to consult with healthcare professionals who specialize in vagus nerve stimulation to evaluate its appropriateness and explore the most suitable treatment options based on individual circumstances.
If you’re fascinated by the potential of vagus nerve stimulation and want to delve deeper into understanding this remarkable system within your body, “My Vagus Nerve & Me Book” is the perfect resource. Discover the secrets of the vagus nerve, from its role in regulating vital bodily functions to innovative ways to stimulate it for better health. This comprehensive guide will take you on a journey through the complexities of one of the most astonishing systems in the human body. Ready to unlock the power of your vagus nerve? Get My Vagus Nerve & Me eBook today and embark on a path to enhanced well-being.