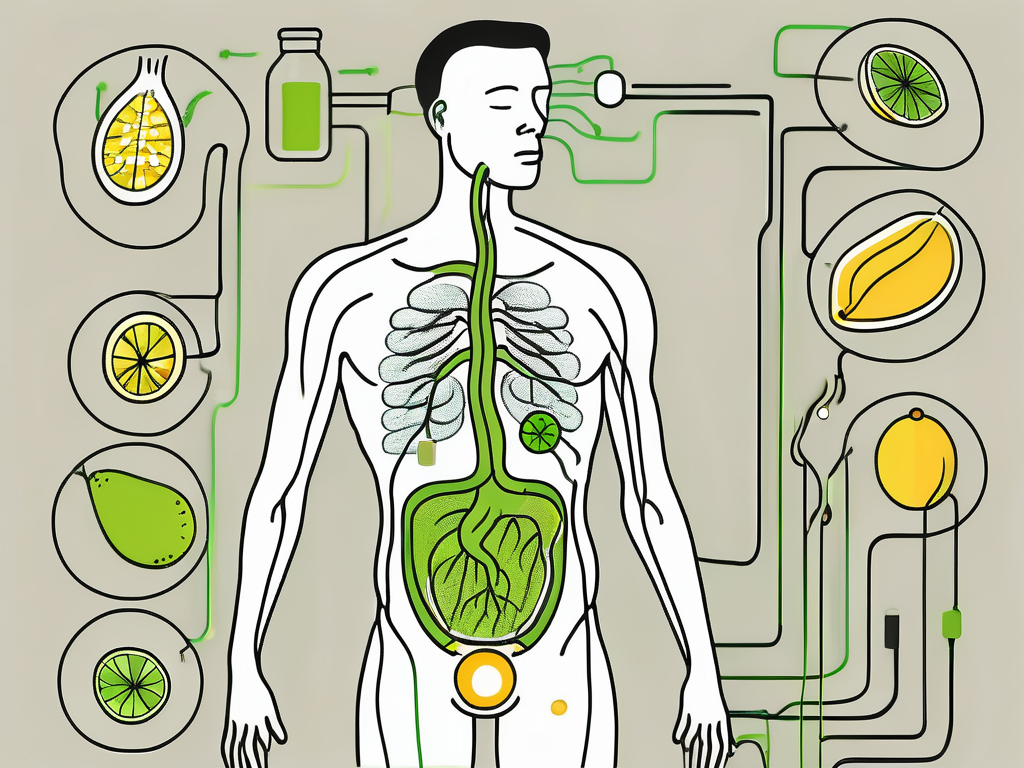
Gastroparesis is a complex digestive disorder that affects the normal movement of food from the stomach to the small intestine. It is characterized by delayed stomach emptying, leading to symptoms such as nausea, vomiting, abdominal pain, bloating, and early satiety. Traditional treatment options for gastroparesis include dietary modifications, medications to manage symptoms, and in severe cases, surgical interventions. However, in recent years, there has been growing interest in the potential of vagus nerve stimulation (VNS) as a treatment approach for gastroparesis.
Understanding Gastroparesis
Gastroparesis is a condition that disrupts the normal functions of the stomach. The exact causes of gastroparesis are not fully understood, but it is commonly associated with diabetes, post-surgical complications, and neurological disorders. The primary underlying problem in gastroparesis is the malfunctioning of the muscles and nerves responsible for controlling stomach contractions, which leads to delayed gastric emptying.
Gastroparesis can have a significant impact on a person’s quality of life. Imagine waking up every morning feeling nauseous and having to deal with constant abdominal pain throughout the day. This is the reality for many individuals living with gastroparesis. The condition can make it challenging to enjoy meals and can lead to malnutrition and weight loss if not properly managed.
The Pathophysiology of Gastroparesis
Gastroparesis can occur due to damage or dysfunction of the vagus nerve, which plays a crucial role in regulating the digestive system. When this nerve is not functioning properly, the coordination of muscle contractions in the stomach is disrupted, resulting in delayed emptying of food.
Furthermore, the muscles in the stomach may become weak and lose their ability to contract effectively. This can further contribute to the delayed emptying of food from the stomach. The exact mechanisms behind the damage or dysfunction of the vagus nerve are still being studied, but it is believed that inflammation, autoimmune reactions, and viral infections may play a role.
Symptoms and Diagnosis of Gastroparesis
Common symptoms of gastroparesis include nausea, vomiting, abdominal pain, bloating, and a feeling of fullness even after eating small amounts of food. These symptoms can vary in severity and may worsen over time. Individuals with gastroparesis often find themselves avoiding certain foods that they know will trigger their symptoms, leading to a limited and restrictive diet.
Diagnosing gastroparesis can be challenging, as the symptoms can mimic other gastrointestinal disorders. Healthcare providers may perform various tests to confirm the diagnosis. Gastric emptying studies involve consuming a meal with a small amount of radioactive material and tracking its movement through the digestive system using a special camera. This test can determine the rate at which the stomach empties and identify any delays.
Endoscopy may also be performed to rule out any structural abnormalities in the stomach that could be causing the symptoms. During this procedure, a thin, flexible tube with a camera on the end is inserted through the mouth and into the stomach. This allows the healthcare provider to visualize the lining of the stomach and check for any signs of inflammation or obstruction.
Gastric manometry is another test that can be used to evaluate the function of the muscles in the stomach. A thin tube with pressure sensors is inserted through the nose and into the stomach. The sensors measure the pressure changes in the stomach as it contracts, providing valuable information about the strength and coordination of the muscle contractions.
Overall, gastroparesis is a complex condition that requires a multidisciplinary approach for effective management. Treatment options may include dietary modifications, medications to improve stomach motility, and in severe cases, surgical interventions. It is important for individuals with gastroparesis to work closely with their healthcare team to develop a personalized treatment plan that addresses their specific needs and symptoms.
The Role of the Vagus Nerve in Digestion
The vagus nerve, also known as the tenth cranial nerve, is a crucial part of the autonomic nervous system. It carries nerve signals between the brain and various organs, including the stomach, heart, and intestines. In digestion, the vagus nerve controls the movement and contraction of muscles in the gastrointestinal tract, including the stomach.
Anatomy and Function of the Vagus Nerve
The vagus nerve is a long nerve that originates in the brainstem and extends down through the neck, chest, and abdomen. It is composed of both sensory and motor fibers, allowing it to transmit signals from the brain to the stomach and vice versa. The vagus nerve is responsible for regulating gastric motility, secretion of gastric juices, and coordinating the digestive process.
Within the gastrointestinal tract, the vagus nerve branches out extensively, forming a complex network of nerve fibers. These fibers innervate the muscles of the stomach, allowing for precise control over its contractions. Additionally, the vagus nerve communicates with specialized cells in the stomach lining, known as enteroendocrine cells, which play a crucial role in the secretion of gastric juices.
Furthermore, the vagus nerve acts as a vital link between the brain and the gut. It relays information about the state of the digestive system to the brain, allowing for the regulation of hunger, satiety, and other aspects of appetite control. This bidirectional communication between the brain and the stomach is essential for maintaining a healthy digestive process.
The Vagus Nerve and Gastric Motility
In the context of gastroparesis, the vagus nerve’s role in regulating gastric motility becomes particularly relevant. Gastroparesis is a condition characterized by delayed gastric emptying, where the stomach takes longer than usual to empty its contents into the small intestine. This can lead to symptoms such as nausea, vomiting, and bloating.
When the vagus nerve is not functioning properly, the coordinated contractions of the stomach muscles are disrupted, leading to delayed gastric emptying. This dysfunction can be caused by various factors, including diabetes, surgery, or certain medications. Understanding the role of the vagus nerve in gastric motility has prompted researchers to explore potential treatments targeting this nerve.
One approach being investigated is vagus nerve stimulation (VNS), a technique that involves delivering electrical impulses to the vagus nerve. By stimulating the vagus nerve, researchers aim to restore normal gastric motility and alleviate symptoms associated with gastroparesis. Preliminary studies have shown promising results, with some patients experiencing improvements in gastric emptying and symptom relief.
Moreover, the vagus nerve’s involvement in digestion extends beyond gastric motility. It also plays a role in the regulation of other digestive processes, such as the release of digestive enzymes and the absorption of nutrients. Dysfunction of the vagus nerve can disrupt these processes, leading to digestive disorders and nutrient deficiencies.
Understanding the intricate relationship between the vagus nerve and digestion is crucial for developing targeted therapies for various gastrointestinal conditions. Further research into the mechanisms by which the vagus nerve influences digestive function may uncover new treatment options and improve the quality of life for individuals with digestive disorders.
Vagus Nerve Stimulation: An Overview
Vagus nerve stimulation (VNS) is a therapeutic technique that involves the use of electrical impulses to stimulate the vagus nerve. The vagus nerve, also known as the tenth cranial nerve, is a long and complex nerve that connects the brain to various organs in the body, including the heart, lungs, and gastrointestinal tract. It plays a crucial role in regulating many bodily functions, such as heart rate, digestion, and mood.
VNS has been used successfully in the treatment of various neurological disorders, such as epilepsy and depression. By delivering mild electrical impulses to the vagus nerve, VNS can modulate neural activity, reduce inflammation, and influence the release of neurotransmitters. These effects have shown to be beneficial in managing seizures and improving mood in patients with treatment-resistant depression.
More recently, researchers have investigated the potential of VNS in managing gastroparesis and restoring normal gastric motility. Gastroparesis is a condition characterized by delayed stomach emptying, which can lead to symptoms such as nausea, vomiting, and bloating. Traditional treatment options for gastroparesis include dietary modifications, medications, and in severe cases, surgical interventions. However, these approaches may not always be effective for all patients, leading to the exploration of alternative therapies like VNS.
The Science Behind Vagus Nerve Stimulation
VNS works by delivering mild electrical impulses to the vagus nerve, which can have various effects on the body. The vagus nerve is a major component of the parasympathetic nervous system, which is responsible for promoting rest and relaxation. When VNS is applied, it activates the parasympathetic response, leading to a decrease in heart rate and blood pressure.
Furthermore, VNS has been found to have anti-inflammatory effects. Inflammation is a common underlying factor in many chronic diseases, including neurological disorders and gastrointestinal conditions. By reducing inflammation, VNS may help alleviate symptoms associated with gastroparesis and improve gastric motility.
Additionally, VNS can influence the release of neurotransmitters in the brain, such as serotonin and norepinephrine. These neurotransmitters play a crucial role in regulating mood and emotions. By modulating their release, VNS may have a positive impact on mood disorders commonly associated with gastroparesis, such as anxiety and depression.
Current Applications of Vagus Nerve Stimulation
While VNS is still considered an experimental treatment for gastroparesis, it has shown promising results in some clinical trials. Research studies have reported improvements in symptoms, such as reduced nausea and vomiting, and improvements in gastric emptying rates. These findings suggest that VNS may have the potential to be a valuable addition to the treatment options available for gastroparesis patients.
However, it is important to note that VNS is not a one-size-fits-all solution. The optimal application of VNS in gastroparesis management is still being explored. Factors such as the intensity and frequency of electrical stimulation, as well as the duration of treatment, need to be carefully considered to maximize its effectiveness.
Furthermore, more research is needed to fully understand the long-term effects of VNS and its potential side effects. As with any medical intervention, the benefits and risks must be weighed carefully before considering VNS as a treatment option for gastroparesis.
In conclusion, Vagus nerve stimulation is an exciting and evolving field of research that holds promise for the management of various neurological and gastrointestinal disorders. While more studies are needed to establish its efficacy and optimal application, VNS has the potential to improve the quality of life for patients suffering from gastroparesis and other related conditions.
Vagus Nerve Stimulation as a Treatment for Gastroparesis
Vagus nerve stimulation is being explored as a potential treatment option for patients with refractory gastroparesis, meaning those who have not responded adequately to standard therapies. The idea behind using VNS is to stimulate the vagus nerve and improve the function of the stomach muscles, ultimately leading to more efficient gastric emptying.
The Potential of Vagus Nerve Stimulation
Early studies suggest that VNS may have the potential to improve gastric emptying and alleviate symptoms in some patients with gastroparesis. However, it is important to note that not all patients may respond equally to VNS, and further research is needed to determine which patients are most likely to benefit.
Mechanism of Action in Gastroparesis
The exact mechanism by which VNS improves gastric motility in gastroparesis is not fully understood. Some theories suggest that VNS can modulate the nerve signals involved in stomach contractions, while others propose that it may have anti-inflammatory effects that reduce the inflammation associated with gastroparesis.
One possible mechanism of action is that VNS stimulates the release of acetylcholine, a neurotransmitter that plays a crucial role in regulating gastrointestinal motility. By increasing the release of acetylcholine, VNS may enhance the communication between the nerves and muscles in the stomach, leading to improved gastric emptying.
Another theory suggests that VNS may have an impact on the brain-gut axis, which is the bidirectional communication between the central nervous system and the gastrointestinal tract. It is believed that VNS can modulate this communication, leading to improved coordination between the brain and the stomach, and ultimately resulting in better gastric motility.
Furthermore, VNS has been shown to have anti-inflammatory effects in various conditions. Inflammation is a common feature of gastroparesis, and it is thought to contribute to the dysfunction of the stomach muscles. By reducing inflammation, VNS may help restore normal gastric motility and alleviate symptoms in patients with gastroparesis.
It is worth noting that VNS is typically delivered through a small device that is implanted in the chest. This device sends electrical impulses to the vagus nerve, which then transmits these signals to the stomach. The intensity and frequency of the electrical stimulation can be adjusted based on the individual needs of each patient.
While VNS shows promise as a treatment for gastroparesis, it is important to consider the potential risks and side effects. Common side effects of VNS include hoarseness, cough, and shortness of breath, which are typically mild and temporary. However, more serious complications, such as infection or nerve damage, can occur, although they are rare.
In conclusion, vagus nerve stimulation is an emerging treatment option for patients with refractory gastroparesis. While the exact mechanism of action is not fully understood, VNS has shown potential in improving gastric emptying and alleviating symptoms in some patients. Further research is needed to better understand which patients are most likely to benefit from VNS and to optimize its effectiveness and safety.
Risks and Benefits of Vagus Nerve Stimulation for Gastroparesis
As with any medical intervention, there are risks and benefits to consider when evaluating VNS as a treatment option for gastroparesis. It is important to consult with a healthcare provider to discuss the individual risks and benefits based on the patient’s specific medical history and condition.
Gastroparesis, a condition characterized by delayed stomach emptying, can significantly impact a person’s quality of life. Symptoms such as nausea, vomiting, abdominal pain, and bloating can be debilitating and make it difficult to carry out daily activities. While there are various treatment options available, Vagus Nerve Stimulation (VNS) has emerged as a potential therapeutic approach.
Evaluating the Risks
Potential risks of VNS for gastroparesis include surgical complications, infection at the implant site, and unwanted side effects from the electrical stimulation, such as hoarseness or voice changes. Surgical complications, though rare, can include bleeding, nerve damage, or device malfunction. Infection at the implant site is also a concern, as it can lead to further complications and require additional medical intervention.
Moreover, the electrical stimulation provided by VNS may result in hoarseness or voice changes due to the proximity of the vagus nerve to the vocal cords. While these side effects are generally temporary and resolve over time, they can still cause discomfort and affect a person’s ability to communicate effectively.
Each patient’s case should be thoroughly evaluated to determine if the potential benefits outweigh the risks. Factors such as the severity of gastroparesis symptoms, the patient’s overall health, and their willingness to undergo a surgical procedure should all be considered in the risk assessment process.
Weighing the Benefits
The potential benefits of VNS for gastroparesis can offer a ray of hope to individuals struggling with this chronic condition. Improved symptom control is often reported by patients who undergo VNS therapy. The electrical stimulation delivered by the VNS device helps regulate the function of the stomach, leading to a reduction in symptoms such as nausea, vomiting, and abdominal pain.
Additionally, VNS can potentially reduce the reliance on medication for symptom management. Gastroparesis often requires the use of medications such as prokinetics, antiemetics, and pain relievers. By providing a more targeted approach to symptom control, VNS may allow patients to decrease their medication intake, minimizing potential side effects and improving overall well-being.
Enhanced quality of life is another significant benefit that VNS can offer to individuals with gastroparesis. The debilitating nature of the condition can limit a person’s ability to engage in social activities, enjoy meals, and maintain a healthy weight. With improved symptom control and reduced medication reliance, VNS can potentially restore a sense of normalcy and enable individuals to participate more fully in their daily lives.
It is important to note that the degree of benefit may vary depending on the individual. Each person’s response to VNS therapy can differ, and close monitoring by healthcare professionals is essential to assess the treatment’s effectiveness. Regular follow-up appointments and adjustments to the stimulation settings may be necessary to optimize outcomes and ensure the best possible results.
In conclusion, while Vagus Nerve Stimulation for gastroparesis carries certain risks, the potential benefits it offers in terms of symptom control, reduced medication reliance, and enhanced quality of life cannot be overlooked. By working closely with healthcare providers and considering individual circumstances, patients can make informed decisions about whether VNS is the right treatment option for them.
Future Perspectives on Vagus Nerve Stimulation for Gastroparesis
While VNS shows promise as a treatment approach for gastroparesis, there is still ongoing research and development in this field. Scientists and healthcare professionals are continually exploring ways to refine the technique and gain a better understanding of its effects on gastric motility.
One area of ongoing research focuses on optimizing the parameters and delivery of VNS in gastroparesis patients to achieve better outcomes. Studies are exploring the use of different waveforms, stimulation frequencies, and durations to determine the most effective VNS settings for individual patients. By tailoring the stimulation to each patient’s specific needs, researchers hope to maximize the benefits of VNS and improve gastric motility.
Another exciting development in the field of VNS for gastroparesis is the exploration of novel techniques and technologies. Researchers are investigating the use of closed-loop systems, where the VNS device can automatically adjust its stimulation based on real-time feedback from the patient’s gastric activity. This personalized approach has the potential to optimize treatment and provide better symptom relief.
The Future of Gastroparesis Treatment
With the advances in VNS and ongoing research, the future of gastroparesis treatment holds the potential for more personalized and effective therapies. As our understanding of gastroparesis and the vagus nerve deepens, we may see further innovations that revolutionize the management of this challenging condition.
One area of interest is the potential combination of VNS with other treatment modalities. Researchers are exploring the use of VNS in conjunction with medications, such as prokinetic agents, to enhance the therapeutic effects. By combining different treatment approaches, healthcare providers hope to achieve synergistic effects and improve overall patient outcomes.
Furthermore, advancements in neuroimaging techniques may provide valuable insights into the mechanisms underlying VNS and its effects on gastric motility. Functional magnetic resonance imaging (fMRI) and positron emission tomography (PET) scans can help visualize the changes in brain activity and neural pathways associated with VNS. This knowledge can contribute to a deeper understanding of the therapeutic mechanisms and guide further refinements in VNS therapy.
In conclusion, vagus nerve stimulation represents a promising treatment approach for gastroparesis. While it is still considered experimental, early studies have shown positive results in improving gastric motility and alleviating symptoms. However, it is important to consult with a healthcare provider to determine the suitability of VNS based on individual medical history and condition. The field of vagus nerve stimulation for gastroparesis is evolving, and with ongoing research and advancements, we may witness further breakthroughs in the management of this complex condition.
If you’re intrigued by the potential of vagus nerve stimulation for managing gastroparesis and wish to delve deeper into the wonders of this vital nerve, “My Vagus Nerve & Me Book” is your essential guide. Discover the profound impact the vagus nerve has on your health, from digestion and heart rate to mental well-being and immune system function. Learn about its intricate role in your body’s operations and explore natural and artificial methods to stimulate this incredible nerve for optimal health. Get My Vagus Nerve & Me eBook today and embark on a journey to better understand and harness the power of your vagus nerve for a healthier, more balanced life.