Fainting, also known as syncope, can be a frightening and bewildering experience. It often occurs suddenly, leaving individuals feeling weak, dizzy, and disoriented. While fainting can have various causes, one factor that has gained attention in recent years is the role of the vagus nerve. The vagus nerve, also called the tenth cranial nerve, plays a crucial role in regulating numerous bodily functions. In this article, we will delve into the anatomy of the vagus nerve, its connection to fainting, the symptoms and diagnosis of vagus nerve disorders, treatment options, and the impact these conditions can have on an individual’s quality of life. It is important to note that this article aims to provide information only and should not be used as a substitute for professional medical advice. If you experience fainting or suspect a vagus nerve disorder, please consult with a healthcare professional for a thorough evaluation.
The Anatomy of the Vagus Nerve
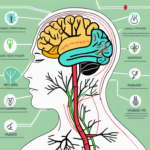
The vagus nerve, also known as the cranial nerve X, is an essential component of the nervous system. It is one of the longest nerves in the body, extending from the brainstem to the abdomen. The word “vagus” comes from the Latin term for “wandering,” which accurately describes the nerve’s extensive pathway throughout the body.
The vagus nerve is divided into two main branches: the left and right vagus nerves. These branches intertwine and innervate various organs and tissues, including the heart, lungs, liver, stomach, and intestines. Their extensive reach allows the vagus nerve to have a profound impact on multiple bodily functions.
The Role of the Vagus Nerve in the Body
As part of the parasympathetic nervous system, the vagus nerve plays a crucial role in regulating the body’s involuntary functions. It acts as a communication highway between the brain and various organs, facilitating the transmission of signals that control heart rate, blood pressure, digestion, and respiratory function.
Furthermore, the vagus nerve is not limited to physical functions alone. It also influences the mind-body connection, impacting mood, memory, and overall well-being. This connection between the vagus nerve and emotional well-being has led to its nickname as the “wandering nerve of compassion.”
The Vagus Nerve and the Autonomic Nervous System
The autonomic nervous system is responsible for regulating and maintaining the body’s internal environment. It consists of two branches: the sympathetic and parasympathetic nervous systems. The sympathetic branch prepares the body for “fight or flight” responses, while the parasympathetic branch oversees rest and relaxation.
The vagus nerve is a major component of the parasympathetic system, working in harmony with the sympathetic branch to maintain balance within the body. While the sympathetic branch prepares the body for action, the vagus nerve counterbalances its effects by promoting rest, relaxation, and digestion.
When the body experiences stress or danger, the sympathetic branch becomes dominant, releasing stress hormones and increasing heart rate and blood pressure. However, the vagus nerve steps in to restore balance once the threat has passed, reducing heart rate, blood pressure, and promoting digestion and healing.
Moreover, the vagus nerve is not just a passive bystander in the autonomic nervous system. It has the ability to sense and respond to changes in the body’s internal environment, making it a crucial regulator of homeostasis.
In conclusion, the vagus nerve is a remarkable structure that extends its influence throughout the body. Its intricate network of branches and its role in the parasympathetic system make it a vital component of our overall well-being. Understanding the anatomy and function of the vagus nerve allows us to appreciate the complexity and interconnectedness of our body’s systems.
The Connection Between the Vagus Nerve and Fainting
Fainting can occur when there is a sudden drop in blood pressure and reduced blood flow to the brain. The vagus nerve is intimately involved in regulating blood pressure and heart rate, making it a key player in the occurrence of fainting episodes.
How the Vagus Nerve Influences Blood Pressure
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in maintaining homeostasis within the body. It helps control blood pressure by sending signals to the heart and blood vessels. When blood pressure drops, the vagus nerve responds by slowing down the heart rate and dilating blood vessels to increase blood flow. This intricate mechanism ensures that vital organs, including the brain, receive an adequate supply of oxygen and nutrients.
However, in some cases, an excessive response from the vagus nerve can lead to a sudden drop in blood pressure, causing fainting. This response, known as vasovagal syncope, is a common cause of fainting episodes.
The Mechanism of Vasovagal Syncope
Vasovagal syncope is one type of fainting that occurs due to overstimulation of the vagus nerve. This response can be triggered by various factors, such as emotional stress, pain, dehydration, or even standing up too quickly. The vagus nerve, being a complex network of fibers, is highly sensitive to these triggers.
When the vagus nerve is excessively activated, it causes a sudden decrease in heart rate and blood pressure, leading to a temporary loss of consciousness. This response is a protective mechanism of the body, as it redirects blood flow to the brain and prevents further injury during potentially dangerous situations.
During a vasovagal syncope episode, the brain temporarily loses its blood supply, resulting in a brief loss of consciousness. This can be a frightening experience for the individual, as they may feel lightheaded, dizzy, or even experience a sensation of tunnel vision before fainting.
It is important to note that while vasovagal syncope is generally harmless and resolves on its own, it can sometimes be a symptom of an underlying medical condition. Individuals who experience frequent or recurrent fainting episodes should seek medical evaluation to determine the cause and appropriate management.
In conclusion, the vagus nerve plays a vital role in regulating blood pressure and heart rate, making it a key player in the occurrence of fainting episodes. Understanding the connection between the vagus nerve and fainting can help individuals recognize and manage these episodes effectively.
Symptoms and Diagnosis of Vagus Nerve Disorders
Recognizing the signs of a vagus nerve disorder is crucial for proper diagnosis and treatment. It’s important to note that the symptoms of vagus nerve disorders can vary significantly among individuals. Consultation with a healthcare professional is essential for an accurate diagnosis.
The vagus nerve, also known as the tenth cranial nerve, plays a vital role in regulating various bodily functions. It extends from the brainstem to the abdomen, innervating organs such as the heart, lungs, stomach, and intestines. When the vagus nerve is not functioning properly, it can lead to a wide range of symptoms that can significantly impact a person’s quality of life.
Recognizing the Signs of a Vagus Nerve Disorder
Vagus nerve disorders can manifest in diverse ways, impacting different bodily functions. Common symptoms include dizziness, lightheadedness, fainting episodes, digestive issues, difficulty swallowing, voice changes, and changes in heart rate.
Dizziness and lightheadedness are often experienced as a result of a drop in blood pressure, known as vasovagal syncope. This occurs when the vagus nerve overreacts to certain triggers, causing a sudden decrease in heart rate and blood flow to the brain. Fainting episodes can be alarming and may occur without warning, making it crucial to identify the underlying cause.
Digestive issues, such as gastroparesis, can also be linked to vagus nerve dysfunction. Gastroparesis is a condition in which the stomach muscles do not contract properly, leading to delayed emptying of the stomach. This can cause symptoms like bloating, nausea, vomiting, and a feeling of fullness even after eating small amounts of food.
Difficulty swallowing, known as dysphagia, can occur when the vagus nerve fails to coordinate the muscles involved in the swallowing process. This can lead to discomfort, choking, and even aspiration of food or liquids into the lungs, which can be dangerous if not addressed promptly.
Vagus nerve disorders can also affect the voice, resulting in changes in vocal quality, pitch, and volume. This can be attributed to the disruption of the nerves that control the muscles responsible for vocalization.
Furthermore, the vagus nerve is intricately connected to the mind-body connection. Dysfunction of this nerve can contribute to mental health concerns such as anxiety and depression. The vagus nerve plays a role in regulating the release of neurotransmitters like serotonin and dopamine, which are essential for mood regulation.
Diagnostic Tests for Vagus Nerve Dysfunction
Diagnosing vagus nerve dysfunction typically involves a thorough medical history review, physical examination, and possibly additional tests. A healthcare professional will carefully evaluate the individual’s symptoms and medical history to determine the most appropriate diagnostic approach.
One common test used to assess vagus nerve function is an electrocardiogram (ECG). This test records the electrical activity of the heart and can help identify any irregularities in heart rate or rhythm that may be associated with vagus nerve dysfunction.
An echocardiogram may also be performed to evaluate the structure and function of the heart. This non-invasive test uses sound waves to create images of the heart, providing valuable information about its overall health and any potential abnormalities.
In some cases, a tilt table test may be recommended. This test involves lying on a table that is tilted to different angles while various measurements, such as heart rate and blood pressure, are monitored. The aim is to provoke symptoms and assess how the vagus nerve responds to changes in position.
Electroencephalogram (EEG) is another diagnostic tool that can be used to evaluate vagus nerve dysfunction. This test measures the electrical activity of the brain and can help identify any abnormalities that may be contributing to the symptoms experienced.
In certain situations, imaging studies such as magnetic resonance imaging (MRI) or computed tomography (CT) scans may be ordered to assess the structures surrounding the vagus nerve. These imaging techniques can provide detailed images of the brain, neck, and chest, helping to identify any potential causes of vagus nerve dysfunction.
It is important to remember that the diagnosis of vagus nerve disorders requires a comprehensive evaluation by a healthcare professional. They will consider the individual’s symptoms, medical history, and the results of any diagnostic tests to make an accurate diagnosis and develop an appropriate treatment plan.
Treatment Options for Vagus Nerve-Related Fainting
Managing vagus nerve-related fainting often requires a comprehensive approach that addresses the underlying cause and aims to prevent future episodes. Treatment options may include lifestyle changes, medical interventions, or a combination of both. It is crucial to work closely with a healthcare professional to develop an individualized treatment plan.
Lifestyle Changes to Manage Vagus Nerve Disorders
Adopting certain lifestyle modifications can help reduce the occurrence and severity of fainting episodes. These may include staying well-hydrated, avoiding triggers (such as prolonged standing or stress), practicing stress management techniques (such as deep breathing or meditation), and maintaining a healthy diet and exercise routine. However, each individual’s situation is unique, so it is important to consult with a healthcare professional for personalized recommendations.
Staying well-hydrated is essential for individuals with vagus nerve-related fainting. Dehydration can exacerbate symptoms and increase the likelihood of fainting episodes. It is recommended to drink an adequate amount of water throughout the day, especially during hot weather or when engaging in physical activities.
Avoiding triggers that can activate the vagus nerve is another crucial aspect of managing fainting episodes. Prolonged standing or being in situations that induce stress can stimulate the vagus nerve and lead to fainting. It is important to identify these triggers and take necessary precautions to minimize their impact. For example, if standing for long periods is a trigger, taking breaks to sit or lie down can help prevent fainting episodes.
Practicing stress management techniques can also be beneficial for individuals with vagus nerve-related fainting. Deep breathing exercises, meditation, and other relaxation techniques can help regulate the autonomic nervous system, which includes the vagus nerve. By reducing stress levels, the likelihood of fainting episodes may decrease.
Furthermore, maintaining a healthy diet and exercise routine is essential for overall well-being and can have a positive impact on vagus nerve function. A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can provide the necessary nutrients to support optimal nerve health. Regular exercise, such as walking or swimming, can improve cardiovascular fitness and promote better blood circulation, which can help prevent fainting episodes.
Medical Interventions for Vagus Nerve-Related Fainting
In some cases, medical interventions may be necessary to manage vagus nerve-related fainting. These interventions could include medications to regulate heart rate and blood pressure, pacemaker implantation to control heart rhythms, or surgical procedures to address underlying conditions. The specific approach will depend on the individual’s symptoms, medical history, and the underlying cause of the vagus nerve dysfunction.
Medications can be prescribed to help regulate heart rate and blood pressure, which are often affected by vagus nerve dysfunction. These medications may include beta-blockers, calcium channel blockers, or other medications that target specific aspects of the autonomic nervous system. It is important to work closely with a healthcare professional to determine the most appropriate medication and dosage for each individual.
In some cases, pacemaker implantation may be recommended to control heart rhythms. A pacemaker is a small device that is surgically implanted under the skin and helps regulate the electrical signals in the heart. By ensuring a steady and consistent heartbeat, the risk of fainting episodes can be significantly reduced.
Surgical procedures may also be considered to address underlying conditions that contribute to vagus nerve dysfunction. For example, if there is an anatomical abnormality or a structural issue in the heart or blood vessels, surgery may be necessary to correct the problem and alleviate the symptoms of fainting.
It is important to note that the decision to pursue medical interventions should be made in consultation with a healthcare professional. They will assess the individual’s specific situation, conduct necessary tests and evaluations, and recommend the most appropriate course of action.
The Impact of Vagus Nerve Disorders on Quality of Life
Living with a vagus nerve disorder can significantly impact an individual’s quality of life. Symptoms such as fainting, digestive issues, or changes in heart rate can make everyday activities challenging and affect overall well-being.
Living with a Vagus Nerve Disorder
Coping with a vagus nerve disorder requires adaptability and self-care. It is important to educate oneself about the condition, follow the prescribed treatment plan, and communicate openly with healthcare providers. Additionally, seeking support from friends, family, and support groups can provide valuable emotional support and practical tips for managing daily life challenges.
Living with a vagus nerve disorder can be a complex journey. Individuals may find themselves navigating through a range of symptoms that can vary in intensity and frequency. These symptoms may include not only fainting and digestive issues but also dizziness, anxiety, and even difficulty swallowing. The impact of these symptoms can extend beyond physical discomfort, affecting one’s ability to engage in social activities, pursue hobbies, or maintain employment.
Adapting to life with a vagus nerve disorder often involves making lifestyle modifications. For example, individuals may need to carefully plan their daily activities to avoid triggers that can exacerbate symptoms. This may mean avoiding crowded places, extreme temperatures, or situations that induce stress. Creating a supportive environment at home and work can also play a crucial role in managing the challenges associated with a vagus nerve disorder.
Coping Strategies for Vagus Nerve-Related Fainting
For individuals experiencing vagus nerve-related fainting, adopting coping strategies can be beneficial in minimizing the impact of fainting episodes. These strategies may include ensuring a safe environment by removing potential hazards, sitting or lying down when feeling lightheaded, and seeking immediate medical attention if fainting occurs. Practicing stress management techniques and maintaining a well-balanced lifestyle can also help manage symptoms and enhance overall well-being.
It is important to note that vagus nerve disorders can vary greatly from person to person. While some individuals may experience infrequent fainting episodes, others may face more frequent and severe symptoms. Understanding one’s own triggers and warning signs can be crucial in developing effective coping strategies.
In addition to physical coping strategies, emotional support is also vital for individuals living with vagus nerve disorders. Connecting with others who share similar experiences can provide a sense of validation, understanding, and encouragement. Support groups, both online and in-person, can serve as a valuable resource for individuals seeking to navigate the challenges of living with a vagus nerve disorder.
In conclusion, understanding the link between the vagus nerve and fainting can shed light on the underlying causes and guide appropriate treatment options. By recognizing the symptoms, seeking timely medical evaluation, and working collaboratively with healthcare professionals, individuals affected by vagus nerve disorders can enhance their quality of life and regain control over their health. If you suspect you have a vagus nerve-related disorder or experience fainting episodes, it is crucial to consult with a healthcare professional for accurate diagnosis and personalized guidance.
If you’re intrigued by the vital role the vagus nerve plays in your health and are seeking to deepen your understanding, “My Vagus Nerve & Me Book” is the perfect resource. Dive into the complexities of this remarkable system and discover how it influences everything from your immune response to your mental well-being. Learn practical ways to stimulate your vagus nerve for improved health and balance. Don’t miss out on the opportunity to unlock the secrets of one of the most fascinating aspects of human physiology. Get My Vagus Nerve & Me eBook today and embark on a journey to better health!