The use of Vagus Nerve Stimulator (VNS) has become increasingly common in the treatment of various medical conditions. However, like any medical procedure, there are potential complications that patients and their caregivers should be aware of. This comprehensive guide aims to provide a deeper understanding of Vagus Nerve Stimulator complications, their identification, management, and prevention.
What is a Vagus Nerve Stimulator?
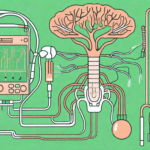
A Vagus Nerve Stimulator is a small electronic device that is surgically implanted under the skin. It is typically placed in the chest and connected to the vagus nerve, which is a vital part of the autonomic nervous system.
But what exactly does the vagus nerve do? Let’s delve into its role in the body.
The Role of the Vagus Nerve in the Body
The vagus nerve is the longest cranial nerve, running from the brainstem to the abdomen. It is a complex network of fibers that branches out to various organs and tissues throughout the body. This nerve plays a crucial role in regulating many bodily functions, including heart rate, digestion, and mood regulation.
When it comes to heart rate, the vagus nerve acts as a natural pacemaker, helping to slow down the heart rate when it becomes too fast. It also plays a role in controlling blood pressure, ensuring that it remains within a healthy range.
In terms of digestion, the vagus nerve is responsible for stimulating the release of digestive enzymes and promoting the movement of food through the gastrointestinal tract. It also plays a role in signaling feelings of fullness and satiety, helping to regulate appetite.
Additionally, the vagus nerve has been found to play a role in mood regulation. It is involved in the release of neurotransmitters such as serotonin and dopamine, which are known to affect mood and emotions. Dysfunction of the vagus nerve has been linked to conditions such as depression and anxiety.
The Purpose of Vagus Nerve Stimulation
Now that we understand the importance of the vagus nerve, let’s explore the purpose of Vagus Nerve Stimulation (VNS).
Vagus Nerve Stimulation is primarily used to manage treatment-resistant epilepsy and depression. For individuals with epilepsy, VNS can help reduce the frequency and severity of seizures. It does this by delivering electrical impulses to the vagus nerve, which in turn affects the brain’s electrical activity and helps prevent abnormal seizure activity.
When it comes to depression, Vagus Nerve Stimulation has shown promising results in alleviating symptoms for individuals who have not responded well to other forms of treatment. By stimulating the vagus nerve, VNS can modulate the brain’s neurotransmitter activity, leading to improvements in mood and overall well-being.
It’s important to note that Vagus Nerve Stimulation is a relatively safe procedure, with minimal side effects. The device can be programmed and adjusted to meet the individual’s specific needs, allowing for personalized treatment.
In conclusion, Vagus Nerve Stimulation is a remarkable medical intervention that harnesses the power of the vagus nerve to manage treatment-resistant epilepsy and depression. By understanding the intricate role of the vagus nerve in the body, we can appreciate the potential benefits that VNS offers to those who are seeking relief from these challenging conditions.
Potential Complications of Vagus Nerve Stimulation
While Vagus Nerve Stimulation has proven to be effective in many cases, it is essential to understand the potential complications that may arise.
When considering Vagus Nerve Stimulation as a treatment option, it is important to be aware of the various physical and psychological side effects that can occur. These side effects can vary in severity and may require medical attention or adjustments to the treatment plan.
Physical Side Effects
Physical side effects related to Vagus Nerve Stimulation can include hoarseness, coughing, difficulty swallowing, and shortness of breath. These symptoms may occur due to the stimulation of the vagus nerve, which can affect the muscles and function of the throat and respiratory system. It is crucial for patients to communicate any discomfort or changes in their ability to breathe or swallow to their healthcare provider.
In some cases, patients may also experience neck pain or tightness near the device implantation site. This can be a result of the surgical procedure or the presence of the device itself. It is important for patients to follow post-operative care instructions and report any persistent or worsening pain to their healthcare provider.
Psychological Side Effects
Psychological side effects are relatively rare but can occur in some patients undergoing Vagus Nerve Stimulation. These side effects may include changes in mood, irritability, depression, anxiety, or difficulties with concentration. It is crucial for patients to be aware of these potential changes and to monitor their emotional well-being closely.
If any emotional changes are noticed, it is important to discuss them with a healthcare provider. They can help determine if these changes are related to the Vagus Nerve Stimulation treatment or if there are other factors at play. In some cases, adjustments to the stimulation parameters or additional psychological support may be necessary to ensure the overall well-being of the patient.
It is important to note that not all patients will experience these side effects, and the benefits of Vagus Nerve Stimulation may outweigh the potential risks for many individuals. However, it is crucial for patients to have a thorough understanding of the possible complications and to have open and honest discussions with their healthcare provider before proceeding with this treatment option.
Identifying Vagus Nerve Stimulator Complications
Recognizing the signs and symptoms of potential complications is crucial for timely intervention and management.
The Vagus Nerve Stimulator (VNS) is a medical device that is implanted in patients with epilepsy to help control seizures. While it is generally a safe and effective treatment option, there are potential complications that can arise. Being aware of these complications and knowing when to seek medical attention is important for the well-being of the patient.
Symptoms to Watch For
Patients and caregivers should be vigilant for any red flags such as excessive pain, infection at the implantation site, persistent hoarseness or difficulty swallowing, unexpected changes in seizure frequency or depression symptoms, and unexplained mood swings.
Excessive pain at the implantation site can be an indication of a problem with the VNS device or the surgical procedure. Infection at the implantation site is another potential complication that should not be ignored. It can cause pain, redness, swelling, and discharge. Persistent hoarseness or difficulty swallowing may indicate that the VNS is affecting the vocal cords or the muscles involved in swallowing.
Changes in seizure frequency or the emergence of new symptoms such as depression or mood swings should also be taken seriously. While it is normal for seizure frequency to fluctuate, unexpected and significant changes may indicate a problem with the VNS device or its settings. Depression symptoms and unexplained mood swings can also be associated with the VNS and should be monitored closely.
When to Seek Medical Attention
If any concerning symptoms arise, it is crucial to contact a healthcare professional. They will be able to evaluate the patient’s condition, provide appropriate advice, and determine if further medical intervention is necessary.
When contacting a healthcare professional, it is important to provide detailed information about the symptoms experienced, including their severity, duration, and any factors that may have triggered them. This information will help the healthcare professional make an accurate assessment and determine the best course of action.
Depending on the symptoms and their severity, the healthcare professional may recommend a visit to the clinic or hospital for further evaluation. This may involve imaging tests, such as X-rays or MRIs, to assess the VNS device and its placement. Blood tests may also be conducted to check for signs of infection or other underlying issues.
In some cases, the healthcare professional may need to adjust the settings of the VNS device to better control seizures or address any complications. This can usually be done through a non-invasive programming device that communicates with the implanted VNS.
It is important for patients and caregivers to remember that seeking medical attention promptly is crucial in managing VNS complications. Early intervention can help prevent further complications and ensure the best possible outcome for the patient.
Managing and Treating Vagus Nerve Stimulator Complications
When complications occur, there are various approaches to manage and treat them effectively. The specific treatment options will depend on the nature and severity of the complication.
Complications related to Vagus Nerve Stimulator (VNS) can vary in their presentation and impact on the patient. It is crucial to identify and address these complications promptly to ensure the best possible outcome for the individual.
Non-Surgical Treatment Options
In some cases, non-surgical interventions such as adjusting the stimulation settings, medication adjustments, or therapy may help alleviate certain complications. These non-invasive approaches aim to optimize the functioning of the VNS device and minimize any adverse effects.
Adjusting the stimulation settings involves modifying the electrical impulses delivered by the VNS device. By fine-tuning the parameters, healthcare professionals can tailor the stimulation to the patient’s specific needs, potentially reducing complications such as voice changes, coughing, or shortness of breath.
Medication adjustments may be necessary to manage complications such as hoarseness, throat pain, or difficulty swallowing. By altering the dosage or type of medication, healthcare professionals can alleviate these symptoms and improve the patient’s overall comfort.
Therapy, including speech therapy or swallowing therapy, can be beneficial for individuals experiencing difficulties in these areas due to VNS complications. These therapeutic interventions aim to strengthen and improve the affected functions, enabling patients to regain their quality of life.
It is essential to work closely with a healthcare professional to determine the most appropriate course of action. They will assess the specific complications and tailor the non-surgical treatment options to the individual’s needs, ensuring the best possible outcome.
Surgical Treatment Options
In more severe cases, surgical intervention may be necessary to address the complications associated with VNS. This may involve the removal or repositioning of the Vagus Nerve Stimulator or related components.
Surgical removal of the VNS device may be considered if the complications are severe and unresponsive to non-surgical interventions. This procedure requires careful planning and execution to minimize any potential risks and ensure the patient’s safety.
Repositioning the VNS device involves surgically adjusting its placement to alleviate complications such as pain, discomfort, or skin irritation. This procedure aims to optimize the positioning of the device, reducing the likelihood of adverse effects and improving the patient’s overall experience with VNS therapy.
Only a skilled healthcare professional can determine the most suitable surgical approach based on individual circumstances. They will consider factors such as the nature and severity of the complications, the patient’s overall health, and their specific needs and preferences.
Preoperative evaluations, including imaging studies and thorough assessments, are essential to ensure the surgical procedure’s success and minimize any potential risks. Postoperative care and follow-up are equally important to monitor the patient’s progress and address any further complications that may arise.
In conclusion, managing and treating Vagus Nerve Stimulator complications requires a comprehensive approach that considers both non-surgical and surgical treatment options. By working closely with healthcare professionals, individuals can find the most suitable interventions to address their specific complications and improve their quality of life.
Prevention of Vagus Nerve Stimulator Complications
While complications are possible, there are steps that can be taken to minimize their occurrence.
Complications can arise from the implantation of a Vagus Nerve Stimulator, but with proper precautions and post-procedure care, these risks can be significantly reduced. It is important for patients to be well-informed about the procedure and its potential complications, as this knowledge can help them make an informed decision.
Pre-Procedure Precautions
Prior to the implantation of a Vagus Nerve Stimulator, thorough evaluations and discussions with a healthcare professional are essential. This includes a comprehensive review of a patient’s medical history, potential risks, and benefits of the procedure. Understanding the procedure and its potential complications can help patients make an informed decision.
During the pre-procedure phase, the healthcare team will conduct various tests and assessments to ensure that the patient is a suitable candidate for the Vagus Nerve Stimulator implantation. These evaluations may include neurological examinations, imaging studies, and psychological assessments. By thoroughly assessing the patient’s overall health and well-being, the healthcare team can identify any potential risks or contraindications that may increase the likelihood of complications.
Furthermore, it is crucial for patients to disclose any pre-existing medical conditions, allergies, or medications they are currently taking. This information allows the healthcare team to tailor the procedure and post-procedure care specifically to the patient’s needs, minimizing the risk of complications.
Post-Procedure Care and Maintenance
Following the implantation, it is crucial to adhere to the recommended post-procedure care and maintenance guidelines provided by the healthcare team. Regular follow-up appointments, proper hygiene of the implantation site, and maintaining an active line of communication with medical professionals are vital for minimizing complications.
Patients will be provided with detailed instructions on how to care for the implantation site, including proper cleaning techniques and any necessary dressing changes. It is important for patients to follow these instructions diligently to prevent infections or other complications. Additionally, patients should be aware of any signs or symptoms that may indicate a problem, such as increased pain, redness, or swelling at the implantation site, and promptly report them to their healthcare team.
Regular follow-up appointments will be scheduled to monitor the patient’s progress and address any concerns or complications that may arise. During these appointments, the healthcare team will assess the functioning of the Vagus Nerve Stimulator and make any necessary adjustments to optimize its effectiveness. Open and honest communication between the patient and the healthcare team is crucial during this phase, as it allows for timely intervention and prevention of potential complications.
In addition to the physical care of the implantation site, patients should also prioritize their overall well-being. This includes maintaining a healthy lifestyle, managing stress levels, and following any additional recommendations provided by the healthcare team. By taking a holistic approach to their health, patients can support the success of the Vagus Nerve Stimulator and minimize the risk of complications.
The Future of Vagus Nerve Stimulation
Research and ongoing developments in the field of Vagus Nerve Stimulation continue to explore potential advancements and alternatives.
Ongoing Research and Developments
Scientists and clinicians are continually investigating ways to optimize Vagus Nerve Stimulation therapy, reduce complications, and expand its application to other medical conditions. This includes advancements in implant technology, refinements in stimulation parameters, and the exploration of new treatment indications.
One area of ongoing research is focused on improving the longevity and durability of Vagus Nerve Stimulation devices. Researchers are exploring new materials and designs that can enhance the lifespan of the implants, reducing the need for frequent replacements and improving patient comfort. Additionally, efforts are being made to develop wireless and miniaturized devices that can be easily implanted and provide targeted stimulation to specific areas of the vagus nerve.
Another avenue of research is centered around optimizing the stimulation parameters used in Vagus Nerve Stimulation therapy. Scientists are studying the effects of different stimulation frequencies, pulse widths, and amplitudes to determine the most effective settings for specific medical conditions. By fine-tuning these parameters, researchers hope to enhance the therapeutic benefits of Vagus Nerve Stimulation and minimize any potential side effects.
Furthermore, there is ongoing exploration of new treatment indications for Vagus Nerve Stimulation. While it is currently approved for conditions such as epilepsy and depression, researchers are investigating its potential use in other neurological disorders, such as Alzheimer’s disease, Parkinson’s disease, and chronic pain. Preliminary studies have shown promising results, and further research is underway to establish the efficacy and safety of Vagus Nerve Stimulation in these new applications.
Potential Alternatives to Vagus Nerve Stimulation
While Vagus Nerve Stimulation is a valuable therapeutic option, alternative treatments and therapies are also being explored. These include deep brain stimulation, transcranial magnetic stimulation, and novel pharmacological approaches.
Deep brain stimulation (DBS) involves the implantation of electrodes in specific regions of the brain to deliver electrical impulses. It has been approved for the treatment of Parkinson’s disease, essential tremor, and dystonia. DBS offers a targeted approach to neuromodulation and has shown promising results in improving motor symptoms and quality of life in patients with these conditions.
Transcranial magnetic stimulation (TMS) is a non-invasive technique that uses magnetic fields to stimulate specific areas of the brain. It has been approved for the treatment of depression and is being investigated for other psychiatric disorders, such as obsessive-compulsive disorder and schizophrenia. TMS offers a non-surgical alternative to Vagus Nerve Stimulation and has shown efficacy in improving mood and reducing symptoms in certain patients.
Novel pharmacological approaches are also being explored as potential alternatives to Vagus Nerve Stimulation. Researchers are investigating the use of specific medications that can modulate the activity of the vagus nerve, mimicking the effects of stimulation. These pharmacological approaches aim to provide similar therapeutic benefits without the need for surgical implantation.
In conclusion, the future of Vagus Nerve Stimulation holds great promise. Ongoing research and developments are focused on optimizing therapy, expanding its applications, and exploring alternative treatments. With continued advancements in technology and a deeper understanding of the underlying mechanisms, Vagus Nerve Stimulation has the potential to revolutionize the field of neuromodulation and improve the lives of countless individuals suffering from neurological disorders.
If you’re fascinated by the incredible capabilities of the vagus nerve and its profound impact on your health, “My Vagus Nerve & Me Book” is an essential read. Dive into the complexities of this remarkable system that orchestrates your body’s most vital functions, from heart rate regulation to digestion, and discover both natural and artificial methods to stimulate this nerve for optimal well-being. Uncover the secrets of liver detoxification, blood sugar regulation, and much more. Ready to embark on a journey of discovery and harness the power of your vagus nerve? Get My Vagus Nerve & Me eBook today and take the first step towards understanding and enhancing your health.