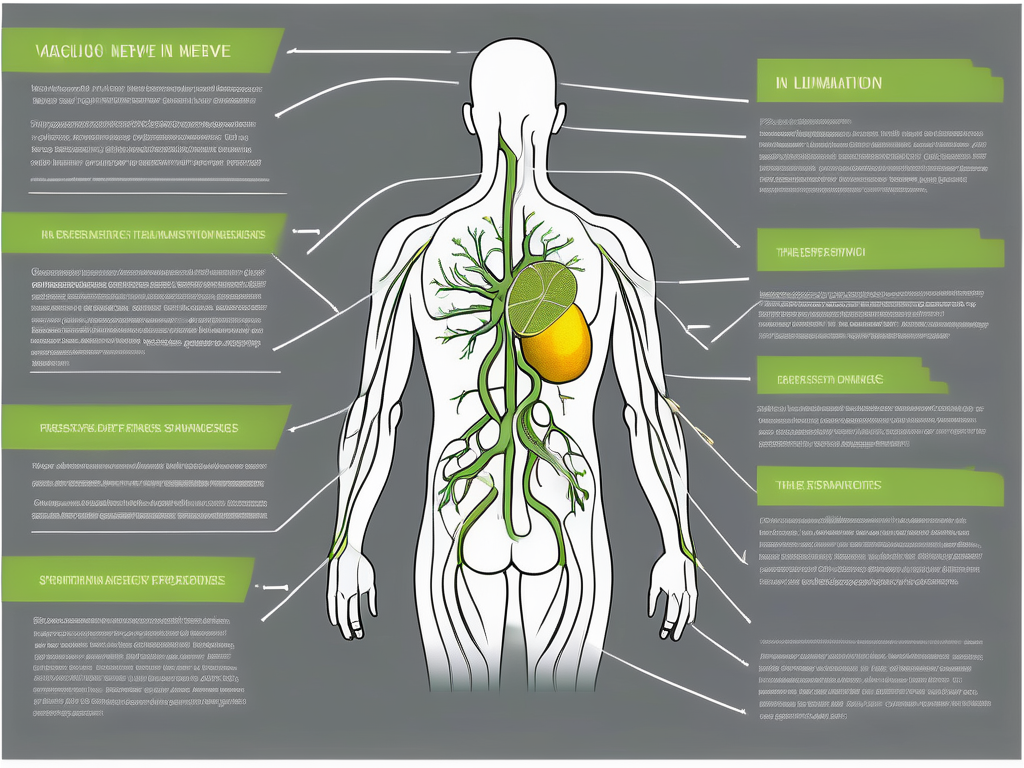
The vagus nerve is a key player in the intricate network of nerves that make up our autonomic nervous system. This nerve, also known as the “wandering nerve,” travels from the brainstem down to the abdomen, innervating various organs along the way. The vagus nerve plays a vital role in regulating our heart rate, digestion, and other essential bodily functions.
What is the Vagus Nerve?
The vagus nerve, officially called the tenth cranial nerve or CN X, is the longest cranial nerve in our body. It is responsible for transmitting sensory and motor signals between the brain and various parts of the body. This nerve is involved in both voluntary and involuntary actions, making it an essential component of our overall well-being.
But what exactly does the vagus nerve do? Let’s delve deeper into its role and function.
The Role and Function of the Vagus Nerve
The vagus nerve is primarily responsible for regulating many involuntary activities, including heart rate, digestion, breathing, and even the reflexes involved in vomiting or coughing. It acts as a communication highway between the brain and organs, ensuring the smooth coordination of bodily functions.
When it comes to heart rate, the vagus nerve plays a crucial role in maintaining a healthy rhythm. It helps to slow down the heart rate during periods of relaxation and rest, allowing the body to conserve energy. On the other hand, during times of stress or excitement, the vagus nerve reduces its influence, allowing the heart to beat faster and pump more blood to meet the increased demand.
In terms of digestion, the vagus nerve is responsible for regulating the movement of food through the digestive tract. It stimulates the release of digestive enzymes and promotes the absorption of nutrients from the intestines. Additionally, the vagus nerve also plays a role in controlling the sensation of fullness and satiety, helping to prevent overeating.
When it comes to breathing, the vagus nerve helps to regulate the muscles involved in respiration. It controls the rate and depth of breathing, ensuring that the body receives an adequate supply of oxygen and removes carbon dioxide efficiently. This automatic control allows us to breathe effortlessly without having to consciously think about it.
Furthermore, the vagus nerve is involved in various reflexes, such as vomiting and coughing. When we ingest something harmful or irritating, the vagus nerve triggers the reflex to expel the substance from our body, protecting us from potential harm.
Anatomy of the Vagus Nerve
The vagus nerve originates in the medulla oblongata, which is the lower part of the brainstem. It extends down through the neck and chest, innervating various organs such as the heart, lungs, stomach, and intestines. This complex network of fibers allows the vagus nerve to carry both sensory information from the organs to the brain and motor signals from the brain to the organs.
As the vagus nerve travels through the body, it branches out extensively, forming connections with numerous organs and tissues. These connections allow the nerve to relay information back and forth, ensuring proper communication and coordination between the brain and the rest of the body.
Interestingly, the vagus nerve doesn’t just transmit signals related to bodily functions. It also plays a role in the mind-body connection. Studies have shown that the vagus nerve is involved in regulating mood, emotions, and even social interactions. It is often referred to as the “wandering nerve” due to its extensive reach and influence throughout the body.
In conclusion, the vagus nerve is a remarkable part of our nervous system. Its extensive network of fibers and its role in regulating various bodily functions make it an essential component of our overall health and well-being. Understanding the intricacies of the vagus nerve helps us appreciate the complex interplay between our brain and body, highlighting the remarkable nature of human physiology.
Understanding Vagus Nerve Spasms
Vagus nerve spasms, also known as vagal paroxysms, are sudden and involuntary contractions of the vagus nerve. These spasms can cause a range of symptoms, from mild discomfort to more severe episodes. Understanding the nature of vagus nerve spasms can help individuals recognize and manage their symptoms effectively.
Defining Vagus Nerve Spasms
Vagus nerve spasms occur when the normal rhythmic contractions of the vagus nerve become irregular or overly intense. These spasms can cause a variety of symptoms that may differ depending on the individual and the underlying cause. However, common symptoms include palpitations, dizziness, chest discomfort, gastrointestinal disturbances, and even fainting spells.
The vagus nerve, also known as the tenth cranial nerve, is a crucial component of the autonomic nervous system. It plays a vital role in regulating various bodily functions, including heart rate, digestion, and breathing. When the vagus nerve experiences spasms, these functions can be disrupted, leading to the manifestation of symptoms.
It is important to note that vagus nerve spasms can vary in duration and intensity. Some individuals may experience brief episodes that resolve on their own, while others may have more prolonged and severe spasms that require medical intervention. Understanding the severity and duration of the spasms can help individuals seek appropriate medical care and management.
Common Triggers of Vagus Nerve Spasms
Vagus nerve spasms can be triggered by various factors, including emotional stress, anxiety, intense physical exertion, certain medications, and medical conditions such as epilepsy or autonomic dysfunction. It is important to identify and understand these triggers to minimize the occurrence and severity of vagus nerve spasms.
Emotional stress and anxiety can have a profound impact on the functioning of the vagus nerve. When individuals experience high levels of stress or anxiety, the body’s fight-or-flight response is activated, leading to an increase in sympathetic nervous system activity. This heightened activity can potentially trigger vagus nerve spasms, resulting in the manifestation of symptoms.
In addition to emotional triggers, intense physical exertion can also stimulate vagus nerve spasms. Activities such as heavy lifting, strenuous exercise, or even coughing vigorously can put strain on the vagus nerve, leading to spasms. It is important for individuals engaging in physical activities to be mindful of their limits and take appropriate breaks to prevent overexertion.
Certain medications, such as anti-arrhythmics or anti-seizure drugs, can also influence the functioning of the vagus nerve. These medications may affect the electrical signals transmitted by the nerve, potentially leading to spasms. It is essential for individuals taking such medications to be aware of the possible side effects and consult their healthcare provider if they experience any symptoms related to vagus nerve spasms.
Furthermore, underlying medical conditions, such as epilepsy or autonomic dysfunction, can predispose individuals to vagus nerve spasms. In epilepsy, abnormal electrical activity in the brain can trigger seizures, which may involve vagus nerve spasms. Autonomic dysfunction, on the other hand, refers to a condition where the autonomic nervous system does not function properly, leading to disturbances in various bodily functions, including vagus nerve activity.
By understanding the common triggers of vagus nerve spasms, individuals can take proactive measures to minimize their occurrence. This may involve stress management techniques, regular exercise within one’s limits, and close monitoring of medication usage. Additionally, individuals with underlying medical conditions should work closely with their healthcare providers to develop a comprehensive management plan that addresses the specific triggers and symptoms associated with vagus nerve spasms.
Causes of Vagus Nerve Spasms
While vagus nerve spasms can be distressing, they are often associated with underlying medical conditions or lifestyle factors. Identifying the potential causes of these spasms is crucial for effective management and treatment.
Medical Conditions Linked to Vagus Nerve Spasms
Several medical conditions have been associated with the occurrence of vagus nerve spasms. These include epilepsy, gastroesophageal reflux disease (GERD), certain heart disorders, anxiety disorders, and autonomic dysfunction. Understanding and addressing these underlying conditions is crucial in managing vagus nerve spasms.
Epilepsy is a neurological disorder characterized by recurrent seizures. It has been found that seizures originating from the temporal lobe can cause vagus nerve spasms. In such cases, antiepileptic medications or surgical intervention may be necessary to control both the seizures and the spasms.
GERD, also known as acid reflux, occurs when stomach acid flows back into the esophagus. The irritation caused by this acid reflux can stimulate the vagus nerve and lead to spasms. Lifestyle modifications, such as avoiding trigger foods and elevating the head while sleeping, can help manage GERD and reduce the occurrence of vagus nerve spasms.
Certain heart disorders, such as arrhythmias or abnormal heart rhythms, can affect the vagus nerve and cause spasms. These spasms may manifest as palpitations or a fluttering sensation in the chest. Treatment options for heart-related vagus nerve spasms may include medication, pacemaker implantation, or other interventions recommended by a cardiologist.
Anxiety disorders, such as panic disorder or generalized anxiety disorder, can trigger vagus nerve spasms due to the heightened stress response. The body’s fight-or-flight response can activate the vagus nerve, leading to spasms. Cognitive-behavioral therapy, relaxation techniques, and medications can be helpful in managing anxiety and reducing the occurrence of spasms.
Autonomic dysfunction refers to a condition where the autonomic nervous system, which controls involuntary bodily functions, does not function properly. This dysfunction can affect the vagus nerve and result in spasms. Treatment for autonomic dysfunction may involve medications, lifestyle changes, and therapies aimed at improving autonomic function.
Lifestyle Factors and Vagus Nerve Spasms
Various lifestyle factors can also contribute to the occurrence of vagus nerve spasms. Excessive stress, anxiety, inadequate sleep, poor diet, and lack of physical activity can all play a role in triggering or exacerbating these spasms. Making positive lifestyle changes and adopting stress management techniques can be beneficial for individuals prone to vagus nerve spasms.
Stress is a common trigger for vagus nerve spasms. When the body is under stress, the sympathetic nervous system becomes activated, which can in turn stimulate the vagus nerve and lead to spasms. Engaging in stress-reducing activities such as meditation, deep breathing exercises, or yoga can help manage stress levels and reduce the occurrence of spasms.
Inadequate sleep can also contribute to the occurrence of vagus nerve spasms. Sleep deprivation can disrupt the body’s natural rhythms and increase stress levels, making individuals more susceptible to spasms. Establishing a consistent sleep schedule and practicing good sleep hygiene can promote better sleep quality and reduce the likelihood of spasms.
Poor diet, particularly one high in processed foods, can contribute to inflammation in the body. This inflammation can affect the vagus nerve and lead to spasms. Adopting a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help reduce inflammation and support overall nerve health.
Lack of physical activity can also impact the occurrence of vagus nerve spasms. Regular exercise promotes circulation, reduces stress, and supports overall well-being. Engaging in activities such as walking, swimming, or yoga can help maintain a healthy vagus nerve function and minimize spasms.
Recognizing the Symptoms of Vagus Nerve Spasms
As mentioned earlier, vagus nerve spasms can manifest in a variety of ways. Recognizing the symptoms is vital for early intervention and appropriate management.
Vagus nerve spasms can be a distressing experience, affecting both the physical and psychological well-being of an individual. Understanding the different symptoms associated with these spasms is crucial in order to provide effective care and support.
Physical Symptoms of Vagus Nerve Spasms
Physical symptoms of vagus nerve spasms can include heart palpitations, chest tightness or discomfort, lightheadedness or fainting, shortness of breath, nausea, and gastrointestinal disturbances. These symptoms can vary in intensity and duration, causing significant discomfort and concern for those experiencing them.
Heart palpitations, for example, are characterized by a rapid or irregular heartbeat, often accompanied by a pounding sensation in the chest. This can be alarming and may lead to feelings of anxiety or fear. Chest tightness or discomfort can also be a common physical symptom, causing individuals to feel a sense of pressure or constriction in their chest.
Lightheadedness or fainting can occur as a result of decreased blood flow to the brain during a vagus nerve spasm. This can lead to dizziness, blurred vision, and a feeling of unsteadiness. Shortness of breath is another physical symptom that can be associated with vagus nerve spasms, making it difficult for individuals to breathe deeply or catch their breath.
In addition, vagus nerve spasms can also affect the gastrointestinal system, resulting in symptoms such as nausea, vomiting, abdominal pain, and changes in bowel movements. These gastrointestinal disturbances can further contribute to the discomfort and distress experienced by individuals with vagus nerve spasms.
Psychological Symptoms of Vagus Nerve Spasms
In addition to physical symptoms, vagus nerve spasms can also present with psychological symptoms. Anxiety, panic attacks, feelings of impending doom, and a sense of loss of control may accompany these spasms. The psychological impact of vagus nerve spasms should not be underestimated, as it can significantly affect an individual’s quality of life and overall mental well-being.
Anxiety, for instance, is a common psychological symptom experienced by individuals with vagus nerve spasms. It can manifest as excessive worry, restlessness, irritability, and difficulty concentrating. Panic attacks, characterized by sudden and intense feelings of fear or terror, can also occur during or after a vagus nerve spasm, further exacerbating the psychological distress.
Feelings of impending doom are another psychological symptom that individuals may experience. This can involve a persistent sense of fear or a belief that something terrible is about to happen. The loss of control is also a common psychological response to vagus nerve spasms, as individuals may feel helpless or powerless in the face of these unpredictable and unsettling episodes.
It is important to consider both the physical and psychological aspects when assessing and managing vagus nerve spasms. A holistic approach that addresses both the physical symptoms and the psychological impact can help individuals better cope with and manage their condition.
Diagnostic Procedures for Vagus Nerve Spasms
When experiencing symptoms suggestive of vagus nerve spasms, seeking medical evaluation is essential for accurate diagnosis and appropriate treatment.
Medical History and Physical Examination
During the initial consultation, your healthcare provider will conduct a thorough medical history interview and physical examination. This process aims to gather information about your symptoms, triggers, medical conditions, and overall health. A comprehensive understanding of your medical background can help guide the diagnostic process.
During the medical history interview, your healthcare provider will ask you detailed questions about your symptoms. They will inquire about the frequency, duration, and intensity of the spasms. They may also ask about any triggers that seem to provoke the spasms, such as stress, certain foods, or specific activities.
The physical examination will involve a comprehensive assessment of your body. Your healthcare provider will check your vital signs, such as your heart rate and blood pressure. They will also examine your head and neck, looking for any visible signs of nerve dysfunction. They may gently palpate your neck to assess the vagus nerve and surrounding structures.
In addition to the physical examination, your healthcare provider may perform specific tests to evaluate the function of the vagus nerve. These tests can include measuring your heart rate variability, assessing your gag reflex, or performing an electrocardiogram (ECG) to monitor your heart’s electrical activity.
Laboratory Tests and Imaging
To rule out other potential causes and confirm the presence of vagus nerve spasms, your healthcare provider may recommend certain laboratory tests or imaging studies. These tests can help identify underlying medical conditions, assess organ function, and provide valuable insights into your overall health status.
Common laboratory tests that may be ordered include blood tests to assess your electrolyte levels, liver and kidney function, and thyroid hormone levels. These tests can help identify any abnormalities that may contribute to the development of vagus nerve spasms.
In some cases, your healthcare provider may also recommend imaging studies to further evaluate the structure and function of your organs. Magnetic resonance imaging (MRI) or computed tomography (CT) scans can provide detailed images of your brain, neck, and chest, helping to identify any structural abnormalities or nerve compression that may be causing the spasms.
Additionally, your healthcare provider may suggest specialized tests to assess the function of the vagus nerve directly. These tests can include nerve conduction studies or electromyography (EMG), which measure the electrical activity of the nerves and muscles.
By combining the information obtained from the medical history, physical examination, laboratory tests, and imaging studies, your healthcare provider can make an accurate diagnosis of vagus nerve spasms. This comprehensive approach ensures that other potential causes are ruled out and that appropriate treatment can be initiated to alleviate your symptoms and improve your quality of life.
Treatment Options for Vagus Nerve Spasms
The management of vagus nerve spasms depends on the underlying cause, severity of symptoms, and individual factors. A tailored approach is often required to effectively alleviate symptoms and improve quality of life.
Medications for Vagus Nerve Spasms
For individuals with severe or frequent vagus nerve spasms, medications may be prescribed to help alleviate symptoms. Medications such as anti-seizure drugs or beta-blockers can be used to regulate the activity of the vagus nerve and reduce the occurrence of spasms. It is crucial to work closely with your healthcare provider to find the most suitable medication and dosage.
Non-Pharmacological Treatments for Vagus Nerve Spasms
In addition to medications, various non-pharmacological treatments can be beneficial in managing vagus nerve spasms. Stress management techniques, deep breathing exercises, mindfulness practices, and lifestyle modifications such as regular exercise and a balanced diet can all contribute to symptom relief. It is important to explore these options under the guidance of a healthcare professional.
Living with Vagus Nerve Spasms
While vagus nerve spasms can be challenging to manage, individuals can find ways to lead fulfilling lives with proper support and self-care.
Lifestyle Modifications for Managing Vagus Nerve Spasms
Adopting a holistic approach to managing vagus nerve spasms is vital. Exploring stress reduction techniques, incorporating regular exercise into your routine, prioritizing sleep hygiene, and maintaining a healthy diet can all contribute to symptom improvement. Making gradual lifestyle modifications and being mindful of triggers can make a significant difference in overall well-being.
Support and Resources for Individuals with Vagus Nerve Spasms
Living with vagus nerve spasms can sometimes feel isolating. Seeking support from healthcare professionals, joining support groups, or connecting with others who experience similar challenges can provide valuable emotional support and resources. Remember, it is essential to consult with your healthcare provider for personalized advice and guidance.
In conclusion, understanding vagus nerve spasms and their causes, symptoms, and treatment options is crucial for individuals who experience these distressing episodes. By seeking appropriate medical evaluation, identifying triggers, and adopting a comprehensive approach to management, individuals can find relief and improve their overall quality of life. Remember, each individual’s journey with vagus nerve spasms is unique, and consulting with a healthcare professional is always recommended for personalized advice and guidance.
If you’re intrigued by the vital role the vagus nerve plays in your health and are eager to delve deeper into its functions and the ways you can nurture it, “My Vagus Nerve & Me Book” is the perfect resource for you. Discover the secrets of one of the most sophisticated systems in the human body, and learn practical tips for stimulating your vagus nerve to enhance your immune system, digestion, heart rate, and mental health. Embark on a journey of understanding and caring for your vagus nerve. Get My Vagus Nerve & Me eBook today and take the first step towards optimal well-being.