The vagus nerve is a crucial component of the human nervous system. It plays a pivotal role in the communication between the brain and various organs in the body. One fascinating aspect of the vagus nerve is its ability to cause referred pain. Referred pain is a phenomenon where pain is felt in a different area of the body than where the actual cause of the pain is located.
Anatomy of the Vagus Nerve
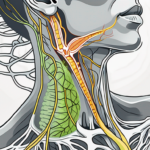
The vagus nerve, also known as the tenth cranial nerve, is the longest cranial nerve in the body. It originates in the brainstem and extends downwards, connecting various organs including the heart, lungs, stomach, and intestines. The nerve is composed of both sensory and motor fibers, allowing for bidirectional communication between the brain and the rest of the body.
As the vagus nerve branches out from the brainstem, it forms a complex network of fibers that innervate different regions of the body. These fibers are responsible for transmitting signals that regulate various bodily functions, ensuring the proper functioning of vital organs.
One of the key features of the vagus nerve is its extensive distribution throughout the body. It sends branches to the heart, where it helps regulate heart rate and rhythm. It also extends to the lungs, where it plays a role in controlling breathing patterns. In the gastrointestinal tract, the vagus nerve is involved in the regulation of digestion, controlling the movement of food through the stomach and intestines.
Role and Function of the Vagus Nerve
The vagus nerve plays a vital role in regulating many bodily functions, including heart rate, digestion, and breathing. It is involved in the parasympathetic nervous system, which is responsible for the body’s “rest and digest” response. When activated, the vagus nerve helps slow down the heart rate, increase digestive activity, and promote relaxation.
In addition to its role in the parasympathetic nervous system, the vagus nerve also has a significant impact on mental health and emotional well-being. It is known to be involved in the regulation of mood, anxiety, and stress responses. Activation of the vagus nerve can have a calming effect on the body, helping to reduce feelings of anxiety and promote a sense of relaxation.
Furthermore, the vagus nerve is also responsible for transmitting sensory information, such as pain signals, from the organs to the brain. This allows the brain to receive important feedback about the internal state of the body and respond accordingly. Dysfunction of the vagus nerve can lead to disruptions in this communication, resulting in various symptoms and health issues.
Location and Pathway of the Vagus Nerve
The vagus nerve travels through various regions of the body, making it susceptible to referred pain. It passes through the neck, chest, and abdomen, innervating multiple organs along its pathway. This extensive distribution allows the vagus nerve to monitor and regulate the functioning of these organs, ensuring their proper coordination and functioning.
When dysfunction occurs in these organs, the vagus nerve can transmit pain signals to different areas, leading to referred pain. For example, a problem in the stomach may cause pain to be felt in the chest or back, due to the shared pathway of the vagus nerve. This phenomenon highlights the interconnectedness of the body and the complex nature of pain perception.
Understanding the anatomy, role, and function of the vagus nerve provides valuable insights into the intricate workings of the human body. It underscores the importance of maintaining a healthy vagus nerve for overall well-being and highlights the potential impact that dysfunction in this nerve can have on various bodily functions.
Understanding Referred Pain
Referred pain is a phenomenon that can be confusing for both patients and healthcare professionals. It occurs when pain is felt in a location other than its actual origin. This is because the nerve pathways that transmit pain signals from different areas of the body can converge or overlap in the spinal cord or brain, leading to misinterpreted pain signals.
Referred pain can be a perplexing experience for individuals who are not familiar with its underlying mechanisms. It defies the conventional notion that pain is always localized to the area of injury or dysfunction. Instead, it manifests as a sensation of discomfort in a completely different part of the body. For example, a person experiencing a heart attack may feel pain radiating down their left arm, rather than directly in the chest where the cardiac event is occurring.
The concept of referred pain is rooted in the intricate network of nerves that exist within our bodies. These nerves serve as messengers, relaying information from various body parts to the brain. When a problem arises in one part of the body, the associated nerves send signals to the brain, causing pain to be perceived not only in the affected area but also in other regions that share neurological connections.
The Concept of Referred Pain
Referred pain occurs due to the convergence of sensory nerves in the spinal cord or brain. This convergence is a fascinating aspect of our nervous system and plays a significant role in the perception of pain. When sensory nerves from different areas of the body merge onto the same pathway in the spinal cord or brain, it creates the potential for confusion in pain perception.
Imagine a scenario where two roads merge into one. Similarly, when nerve pathways converge, the brain receives mixed signals, making it challenging to pinpoint the exact source of the pain. This phenomenon can lead to diagnostic difficulties, as healthcare professionals must carefully analyze the patient’s symptoms and medical history to determine the true origin of the pain.
How Referred Pain Works
The mechanism behind referred pain is not entirely understood. However, researchers have proposed various theories to explain this intriguing phenomenon. One prevailing theory is the concept of “visceral-somatic convergence.” This convergence occurs when the sensory nerves from internal organs and those from the skin and muscles merge onto the same spinal cord segments.
As a result of this convergence, the brain interprets the pain signals from the internal organs as originating from the skin and muscles in the referred pain area. For instance, a person experiencing gallbladder inflammation may feel pain in their right shoulder. This is because the sensory nerves from the gallbladder and the shoulder converge in the spinal cord, causing the brain to misinterpret the source of the pain.
Referred pain is not limited to specific conditions or body parts. It can manifest in various ways, depending on the individual and the underlying cause. Understanding the mechanisms behind referred pain is crucial for healthcare professionals to accurately diagnose and treat patients, as well as for patients to comprehend their own experiences of pain.
Further research is still needed to unravel the complexities of referred pain fully. By delving deeper into the intricacies of our nervous system, scientists hope to gain a more comprehensive understanding of this fascinating phenomenon and improve pain management strategies for those who are affected.
Vagus Nerve and Referred Pain
The vagus nerve can be a major player in the development of referred pain. Due to its extensive connections with various organs in the body, dysfunction in these organs can lead to pain being felt in remote regions. Understanding the connection between the vagus nerve and referred pain can be crucial in diagnosing and treating this condition effectively.
Connection between Vagus Nerve and Referred Pain
When there is dysfunction or inflammation in the organs innervated by the vagus nerve, such as the heart, lungs, or digestive system, the nerve can transmit pain signals to different areas of the body. This can manifest as referred pain in the neck, chest, back, or even the limbs. Identifying the underlying cause of the referred pain is essential for effective treatment.
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It originates in the brainstem and extends down to various organs in the body, including the heart, lungs, stomach, and intestines. This extensive network of connections allows the vagus nerve to play a crucial role in regulating various bodily functions, such as heart rate, digestion, and breathing.
When there is dysfunction or inflammation in any of the organs innervated by the vagus nerve, it can disrupt the normal flow of nerve signals. This disruption can lead to the transmission of pain signals along the vagus nerve pathways, causing referred pain in remote regions of the body.
For example, if there is dysfunction in the heart, the vagus nerve can transmit pain signals to the neck, chest, or left arm, mimicking the symptoms of a heart attack. Similarly, dysfunction in the lungs can cause referred pain in the back or shoulders. Dysfunction in the digestive system can lead to referred pain in the abdomen or even the lower back.
Symptoms of Vagus Nerve Referred Pain
Symptoms of vagus nerve referred pain can vary depending on the specific organ involved. However, common symptoms may include a dull, aching sensation in the chest, radiating pain in the neck or upper back, or discomfort in the abdomen. It is important to note that these symptoms can be indicative of other underlying medical conditions, and a thorough medical evaluation is necessary to determine the exact cause of the referred pain.
In addition to pain, other symptoms may accompany vagus nerve referred pain. These can include nausea, vomiting, shortness of breath, dizziness, or changes in heart rate. These additional symptoms can further complicate the diagnosis, as they may overlap with symptoms of other medical conditions.
Diagnosing vagus nerve referred pain requires a comprehensive evaluation of the patient’s medical history, physical examination, and possibly additional diagnostic tests. The healthcare provider will need to rule out other potential causes of the symptoms and identify any underlying dysfunction in the organs innervated by the vagus nerve.
Treatment for vagus nerve referred pain depends on the underlying cause. In some cases, addressing the dysfunction or inflammation in the affected organ can alleviate the referred pain. This may involve medication, lifestyle changes, or surgical interventions. In other cases, pain management techniques, such as physical therapy, acupuncture, or nerve blocks, may be recommended to help alleviate the symptoms.
It is important for individuals experiencing referred pain to seek medical attention promptly. Early diagnosis and treatment can help prevent further complications and improve the overall prognosis. With proper management, individuals with vagus nerve referred pain can find relief and regain their quality of life.
Causes of Vagus Nerve Referred Pain
Several medical conditions and lifestyle factors can contribute to the development of vagus nerve referred pain. Identifying and addressing these underlying causes can significantly improve the management of this condition.
Medical Conditions Leading to Vagus Nerve Referred Pain
Medical conditions, such as gastroesophageal reflux disease (GERD), myocardial infarction (heart attack), and gastrointestinal disorders, can cause vagus nerve referred pain. GERD, a condition characterized by the backward flow of stomach acid into the esophagus, can irritate the vagus nerve and lead to referred pain. In the case of a heart attack, the vagus nerve can be affected due to the lack of oxygen reaching the heart muscle, causing pain to radiate to other areas of the body. Gastrointestinal disorders, such as peptic ulcers or pancreatitis, can also result in referred pain along the path of the vagus nerve. Additionally, inflammation or dysfunction in the organs innervated by the vagus nerve, such as the stomach or intestines, can contribute to the development of referred pain. Seeking medical advice and appropriate diagnostic testing is crucial in determining the precise cause of the referred pain and ensuring proper treatment.
Lifestyle Factors Contributing to Vagus Nerve Referred Pain
While medical conditions play a significant role in vagus nerve referred pain, lifestyle factors can also contribute to its development or exacerbation. Poor posture, often caused by prolonged sitting or improper ergonomics, can put pressure on the vagus nerve and lead to referred pain. Stress, a common factor in modern life, can also affect the vagus nerve, as it is responsible for regulating the body’s stress response. Chronic stress can result in increased muscle tension and inflammation, which can trigger referred pain. Sedentary lifestyle habits, such as sitting for long periods without movement, can further contribute to muscle imbalances and tension, potentially affecting the vagus nerve. Unhealthy dietary habits, including consuming excessive amounts of processed foods, sugary drinks, or alcohol, can also contribute to inflammation and nerve irritation, leading to referred pain. Making positive lifestyle changes is essential in managing vagus nerve referred pain. Practicing good posture, using ergonomic furniture, and taking regular breaks from sitting can help alleviate pressure on the nerve. Engaging in regular physical activity, such as stretching, yoga, or low-impact exercises, can promote overall muscle health and reduce tension. Managing stress levels through techniques like meditation, deep breathing, or therapy can also have a positive impact on the vagus nerve. Adopting a balanced diet rich in whole foods, fruits, vegetables, and lean proteins can help reduce inflammation and support nerve health, minimizing the frequency and intensity of referred pain episodes.
Diagnosing Vagus Nerve Referred Pain
Diagnosing vagus nerve referred pain can be challenging due to its complex nature and overlapping symptoms with other medical conditions. However, healthcare professionals employ various methods to accurately diagnose and differentiate vagus nerve referred pain from other potential causes.
When a patient presents with symptoms that may be indicative of vagus nerve referred pain, healthcare professionals begin the diagnostic process by conducting a comprehensive clinical examination. This examination involves a thorough assessment of the patient’s medical history, including any previous medical conditions or surgeries that may be relevant to the current symptoms. Additionally, healthcare professionals will perform a physical examination, carefully observing and palpating the patient’s body to identify any areas of tenderness or abnormality.
During the clinical examination, healthcare professionals will also inquire about the nature and location of the pain. This information is vital in determining whether the pain may be originating from the vagus nerve or if it may be attributed to another source. The patient’s description of the pain, such as its intensity, duration, and any exacerbating or relieving factors, can provide valuable insights into the possibility of vagus nerve referred pain.
In addition to the clinical examination, healthcare professionals may also consider the patient’s symptoms and risk factors when assessing the likelihood of vagus nerve referred pain. Common symptoms associated with vagus nerve referred pain include chest discomfort, difficulty swallowing, heartburn, and a sensation of fullness in the throat. Risk factors that may increase the likelihood of vagus nerve referred pain include a history of gastrointestinal disorders, previous surgeries in the abdominal region, or conditions that affect the vagus nerve itself.
Clinical Examination and Diagnosis
During a clinical examination, healthcare professionals will conduct a thorough assessment of the patient’s medical history, perform a physical examination, and inquire about the nature and location of the pain. This information, combined with the patient’s symptoms and risk factors, can provide valuable insights into the possibility of vagus nerve referred pain.
Furthermore, healthcare professionals may utilize additional diagnostic tools to aid in the diagnosis of vagus nerve referred pain. These tools may include imaging studies, such as X-rays or magnetic resonance imaging (MRI), to visualize the structures surrounding the vagus nerve and identify any abnormalities or compressions. Additionally, nerve conduction studies may be performed to assess the function of the vagus nerve and determine if there are any disruptions or abnormalities in its signaling.
Diagnostic Tests for Vagus Nerve Referred Pain
To confirm the diagnosis and determine the underlying cause of vagus nerve referred pain, healthcare professionals may order additional diagnostic tests. These may include electrocardiograms (ECGs), endoscopic procedures, upper gastrointestinal imaging, or other specialized tests depending on the suspected source of the referred pain. Consulting with a healthcare professional is crucial in determining the most appropriate diagnostic approach.
Electrocardiograms (ECGs) are commonly used to evaluate the electrical activity of the heart and rule out any cardiac causes of the referred pain. This test can help differentiate between vagus nerve referred pain and conditions such as angina or myocardial infarction.
Endoscopic procedures, such as esophagogastroduodenoscopy (EGD), may be performed to visualize the esophagus, stomach, and duodenum. This can help identify any abnormalities or inflammation that may be contributing to the vagus nerve referred pain.
In some cases, healthcare professionals may order upper gastrointestinal imaging studies, such as barium swallow or upper gastrointestinal series, to obtain detailed images of the upper digestive tract. These tests can provide valuable information about the structure and function of the esophagus, stomach, and surrounding organs.
Depending on the suspected source of the referred pain, healthcare professionals may also recommend other specialized tests. For example, if a gastrointestinal disorder is suspected, additional tests such as gastric emptying studies or pH monitoring may be performed to assess the function of the digestive system and identify any abnormalities.
In conclusion, diagnosing vagus nerve referred pain requires a comprehensive approach that includes a thorough clinical examination, consideration of the patient’s symptoms and risk factors, and the use of diagnostic tests to confirm the diagnosis and determine the underlying cause. By employing these methods, healthcare professionals can accurately diagnose and differentiate vagus nerve referred pain, leading to appropriate treatment and management strategies.
Treatment Options for Vagus Nerve Referred Pain
Effective treatment options for vagus nerve referred pain aim to address the underlying cause of the pain, alleviate symptoms, and improve the patient’s quality of life. Treatment plans may involve a combination of medication, non-pharmacological interventions, and, in some cases, surgical interventions.
Medication and Drug Therapy
Depending on the underlying cause of the vagus nerve referred pain, healthcare professionals may prescribe medications to manage pain and reduce inflammation. Nonsteroidal anti-inflammatory drugs (NSAIDs), proton pump inhibitors (PPIs), or medications targeting specific conditions may be utilized. It is important to follow the prescribed medication regimen and consult with a healthcare professional regarding potential side effects or drug interactions.
Non-Pharmacological Interventions
Non-pharmacological interventions can play a significant role in managing vagus nerve referred pain. These may include physical therapy, stress management techniques, relaxation exercises, and lifestyle modifications. Implementing healthy lifestyle habits and reducing stress levels can contribute to improved pain management and overall well-being.
Surgical Treatments
In severe cases where other treatment options prove ineffective, healthcare professionals may consider surgical interventions. Surgical procedures targeting the underlying cause of the vagus nerve referred pain can provide long-lasting relief, but they carry certain risks and should only be considered after a thorough evaluation and consultation with a specialist.
Prevention and Management of Vagus Nerve Referred Pain
Preventing and effectively managing vagus nerve referred pain involves a holistic approach that focuses on lifestyle modifications and self-care strategies.
Lifestyle Modifications for Pain Management
Adopting a healthy lifestyle can help reduce the frequency and intensity of referred pain episodes. This includes maintaining good posture, engaging in regular physical activity, managing stress levels through relaxation techniques or therapy, and following a balanced diet. Making these positive changes can promote overall well-being and help manage vagus nerve referred pain.
Coping Strategies for Chronic Pain
Living with chronic pain can be challenging, both physically and emotionally. Adopting coping strategies such as mindfulness techniques, support groups, and seeking therapy can help individuals manage the psychological and emotional impact of vagus nerve referred pain. It is essential to seek professional guidance and explore coping mechanisms that work best for an individual’s specific needs.
In conclusion, understanding vagus nerve referred pain involves recognizing the intricate connections between the vagus nerve, various organs, and the perception of pain. Identifying the underlying causes, pursuing appropriate diagnostic testing, and implementing a comprehensive treatment plan are crucial in effectively managing this condition. If you experience persistent or worsening referred pain, it is essential to consult with a healthcare professional for an accurate diagnosis and tailored treatment approach.
If you’re intrigued by the role of the vagus nerve in referred pain and want to delve deeper into its remarkable functions and impact on your health, “My Vagus Nerve & Me Book” is the perfect resource. Discover the secrets of one of the most sophisticated systems in the human body and learn how to harness its power for your well-being. From understanding its complex anatomy to exploring ways to stimulate it for better immune function, digestion, heart rate, and mental health, this book covers it all. Ready to embark on a journey of discovery and enhance your health? Get My Vagus Nerve & Me eBook today and take the first step towards optimizing your body’s natural processes.