The vagus nerve is a crucial part of our nervous system that plays a vital role in regulating various bodily functions. It is the longest cranial nerve and extends from the brainstem down to the abdomen, passing through various parts of the body, including the neck. Vagus nerve pain in the neck can cause significant discomfort and affect our daily lives. In this article, we will explore the causes, symptoms, and treatment options for vagus nerve pain, and offer insights on living with this condition.
What is the Vagus Nerve?
The vagus nerve, also known as the tenth cranial nerve, is a complex network of fibers that connects the brain to various organs in the body. It is responsible for controlling the parasympathetic nervous system, which helps regulate important functions such as heart rate, digestion, and breathing.
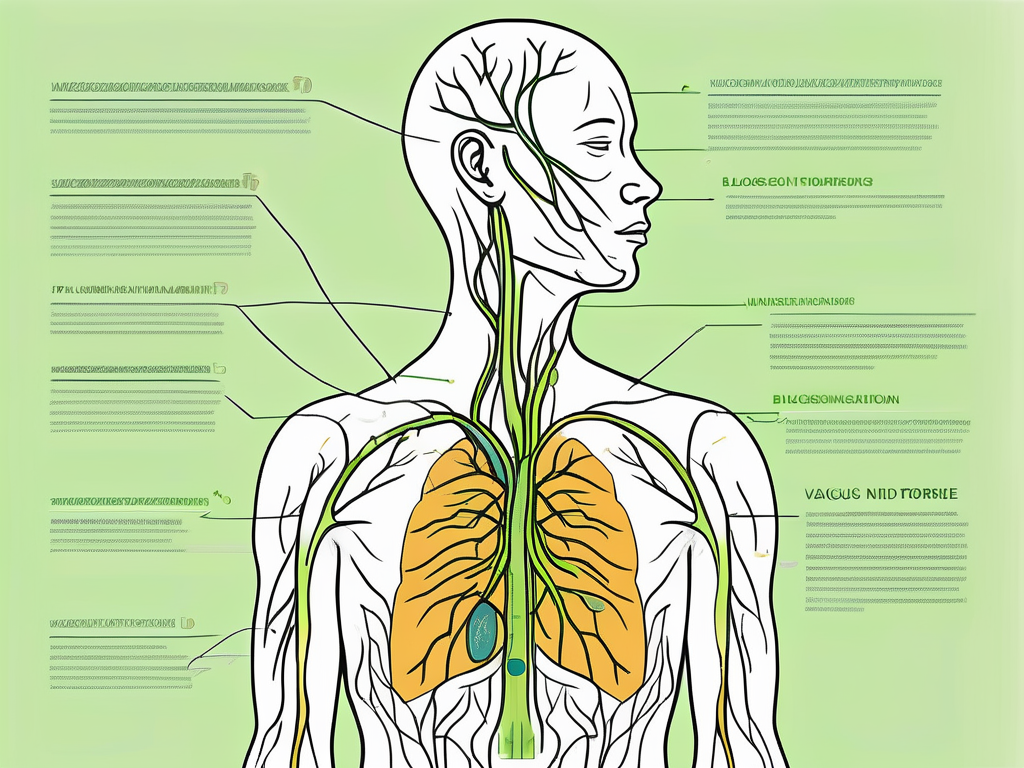
The vagus nerve is the longest cranial nerve in the body, extending from the medulla oblongata in the brainstem to the abdomen. It is named after the Latin word “vagus,” meaning “wandering,” because of its extensive distribution throughout the body.
The vagus nerve is composed of both sensory and motor fibers. Sensory fibers transmit information from the organs to the brain, while motor fibers carry signals from the brain to the organs, allowing for control and regulation.
Anatomy of the Vagus Nerve
The vagus nerve originates in the medulla oblongata, which is located at the base of the brain. It travels through the neck, chest, and abdomen, branching off to innervate various organs along the way.
As the vagus nerve descends through the neck, it gives off branches that innervate the larynx, pharynx, and esophagus. These branches play a crucial role in vocalization and swallowing, allowing us to produce speech and consume food and liquids.
Continuing its journey, the vagus nerve enters the thoracic cavity, where it gives off branches to the heart and lungs. These branches help regulate heart rate, blood pressure, and respiratory function. The vagus nerve’s influence on the heart is particularly significant, as it can slow down the heart rate and reduce blood pressure in response to relaxation or rest.
As the vagus nerve reaches the abdomen, it branches off to innervate various organs, including the stomach, liver, pancreas, and intestines. It plays a crucial role in controlling digestion and gut motility, ensuring the proper breakdown and absorption of nutrients.
Functions of the Vagus Nerve
The vagus nerve has a wide range of functions, including:
- Regulating heart rate and blood pressure: The vagus nerve helps maintain cardiovascular homeostasis by influencing heart rate and blood pressure. It can increase or decrease heart rate depending on the body’s needs.
- Controlling digestion and gut motility: The vagus nerve plays a vital role in the digestive process by stimulating the release of digestive enzymes, enhancing nutrient absorption, and promoting gut motility.
- Influencing respiratory function: The vagus nerve helps regulate breathing by controlling the muscles involved in respiration. It can slow down or speed up breathing rate depending on oxygen and carbon dioxide levels in the body.
- Mediating the release of certain hormones: The vagus nerve is involved in the release of various hormones, including oxytocin, which is known as the “love hormone” and plays a role in social bonding and trust.
- Playing a role in vocalization and swallowing: The vagus nerve innervates the muscles responsible for vocalization and swallowing, allowing us to speak and consume food and liquids smoothly.
Overall, the vagus nerve is a crucial component of the autonomic nervous system, responsible for maintaining homeostasis and ensuring the proper functioning of various organs and systems in the body.
Causes of Vagus Nerve Pain in the Neck
Vagus nerve pain in the neck can occur due to various factors. Understanding the underlying causes can help in managing and treating this condition effectively. Some common causes include:
Physical Trauma
One of the leading causes of vagus nerve pain in the neck is physical trauma. Whiplash injuries, often associated with car accidents, can cause sudden and forceful movements of the neck, leading to damage to the vagus nerve. The impact can result in inflammation and pain along the pathway of the nerve. Additionally, other types of trauma to the neck, such as falls or sports injuries, can also lead to vagus nerve dysfunction and subsequent neck pain.
It is important to note that the severity of the trauma and the extent of the nerve damage can vary from person to person. In some cases, the symptoms may appear immediately after the injury, while in others, they may develop gradually over time.
Infections and Diseases
Infections can also contribute to vagus nerve pain in the neck. Sinusitis, a common condition characterized by inflammation of the sinuses, can cause pressure and irritation on the vagus nerve, leading to neck pain. Additionally, viral infections like shingles, which affect the nerves, can also result in vagus nerve inflammation and subsequent discomfort.
Furthermore, certain diseases can contribute to vagus nerve dysfunction and pain in the neck. For example, individuals with diabetes may experience nerve damage, including the vagus nerve, due to high blood sugar levels. Autoimmune disorders, such as rheumatoid arthritis or lupus, can also affect the nerves and contribute to neck pain.
Lifestyle Factors
Several lifestyle factors can contribute to vagus nerve pain in the neck. Poor posture, often associated with prolonged sitting or incorrect positioning of the neck and shoulders, can put excessive strain on the vagus nerve, leading to discomfort and pain. Additionally, repetitive strain injuries caused by activities like typing or carrying heavy loads can also contribute to nerve irritation and subsequent neck pain.
Chronic stress, a common issue in today’s fast-paced world, can also impact the vagus nerve. Stress can lead to muscle tension and inflammation, which can affect the nerve’s function and contribute to neck pain. It is important to manage stress through relaxation techniques, exercise, and seeking support when needed to minimize its impact on the vagus nerve and overall well-being.
Understanding the various causes of vagus nerve pain in the neck can help individuals identify potential triggers and seek appropriate treatment. It is essential to consult with a healthcare professional for an accurate diagnosis and personalized management plan to alleviate discomfort and promote healing.
Recognizing the Symptoms of Vagus Nerve Pain
Vagus nerve pain in the neck can manifest in various ways, including:
When it comes to vagus nerve pain, the symptoms can be quite diverse and may vary from person to person. Here are some of the physical symptoms that individuals may experience:
Physical Symptoms
– Pain or discomfort in the neck or throat area
One of the most common symptoms of vagus nerve pain is a persistent pain or discomfort in the neck or throat area. This pain can range from mild to severe and may be accompanied by a feeling of tightness or pressure.
– Headaches or migraines
In some cases, vagus nerve pain can also lead to frequent headaches or migraines. These headaches may be accompanied by other symptoms such as sensitivity to light or sound.
– Hoarseness or difficulty swallowing
Individuals with vagus nerve pain may also experience hoarseness or difficulty swallowing. This can make it challenging to speak or eat comfortably.
– Heart palpitations or irregular heartbeats
Another physical symptom of vagus nerve pain is heart palpitations or irregular heartbeats. These sensations can be quite alarming and may cause individuals to feel anxious or worried.
– Digestive issues like nausea, bloating, or difficulty passing stools
Vagus nerve pain can also affect the digestive system, leading to symptoms such as nausea, bloating, or difficulty passing stools. These symptoms can significantly impact an individual’s quality of life.
– Breathing difficulties or shortness of breath
Some individuals with vagus nerve pain may experience breathing difficulties or shortness of breath. This can make it challenging to engage in physical activities or even perform simple tasks.
– Dizziness or fainting spells
Dizziness or fainting spells can also be associated with vagus nerve pain. These episodes can be sudden and may occur without warning, posing a risk to the individual’s safety.
– Dry mouth or excessive saliva production
Lastly, vagus nerve pain can lead to dry mouth or excessive saliva production. These symptoms can be uncomfortable and may affect an individual’s ability to speak or swallow properly.
Emotional and Psychological Symptoms
Chronic vagus nerve pain can also have an impact on mental well-being, leading to symptoms such as anxiety, depression, irritability, or mood swings.
In addition to the physical symptoms, vagus nerve pain can also take a toll on an individual’s emotional and psychological well-being. Living with chronic pain can be mentally exhausting and may lead to various emotional symptoms, including:
– Anxiety
Constant pain and discomfort can cause individuals to feel anxious about their condition and its impact on their daily lives. This anxiety may manifest as restlessness, racing thoughts, or a constant sense of unease.
– Depression
Living with chronic pain can also lead to feelings of sadness, hopelessness, or a loss of interest in activities once enjoyed. Depression can significantly affect an individual’s overall quality of life.
– Irritability
Dealing with persistent pain can make individuals more prone to irritability or moodiness. The frustration of not being able to find relief or engage in regular activities can contribute to feelings of irritability.
– Mood swings
Vagus nerve pain can also cause individuals to experience sudden and unpredictable mood swings. These mood swings can range from feeling elated one moment to feeling down or irritable the next.
It is important to note that everyone’s experience with vagus nerve pain may be different, and not all individuals will experience the same symptoms. If you suspect you may be experiencing vagus nerve pain, it is always best to consult with a healthcare professional for an accurate diagnosis and appropriate treatment.
Diagnostic Procedures for Vagus Nerve Pain
If you are experiencing symptoms suggestive of vagus nerve pain in the neck, it is important to seek medical evaluation. Your doctor may conduct several diagnostic procedures to accurately diagnose and treat your condition.
Medical History and Physical Examination
During your medical evaluation, your doctor will begin by asking about your symptoms, medical history, and any recent injuries or infections. This information will help them understand the potential causes of your vagus nerve pain. They will also perform a thorough physical examination, paying close attention to your neck and throat area. By examining the affected area, your doctor can assess any visible signs of inflammation, swelling, or tenderness.
Additionally, your doctor may examine your vital signs, such as your heart rate and blood pressure, as the vagus nerve plays a crucial role in regulating these functions. They may also check for any associated symptoms like difficulty swallowing or hoarseness, which can provide further clues to the underlying cause of your vagus nerve pain.
Imaging Tests
To further evaluate the structures in your neck and identify any potential nerve damage, your doctor may order imaging tests such as X-rays, CT scans, or MRI scans. These tests can provide detailed images of the bones, muscles, and soft tissues in your neck, allowing your doctor to assess the integrity of the vagus nerve and identify any structural abnormalities or compression.
X-rays use low levels of radiation to produce images of the bones in your neck. They can help detect fractures, dislocations, or any abnormalities in the bony structures that may be affecting the vagus nerve.
CT scans, also known as computed tomography scans, use a combination of X-rays and computer technology to create cross-sectional images of the neck. This imaging technique provides more detailed information about the soft tissues, blood vessels, and nerves, allowing your doctor to evaluate the vagus nerve and surrounding structures more thoroughly.
MRI scans, or magnetic resonance imaging scans, use powerful magnets and radio waves to create detailed images of the structures in your neck. This imaging technique is particularly useful in assessing soft tissues, such as the nerves and blood vessels. By obtaining high-resolution images, MRI scans can help your doctor identify any nerve damage or abnormalities that may be contributing to your vagus nerve pain.
Nerve Conduction Studies
In some cases, your doctor may recommend nerve conduction studies to evaluate the functioning of the vagus nerve and determine if any abnormalities are present. During this procedure, small electrodes are placed on your skin over the vagus nerve pathway. These electrodes deliver small electrical impulses to stimulate the nerve and measure its response.
By measuring the speed and strength of the electrical signals transmitted by the vagus nerve, nerve conduction studies can help identify any disruptions or abnormalities in the nerve’s function. This diagnostic test can provide valuable information about the integrity of the vagus nerve and its potential involvement in your pain symptoms.
It is important to note that these diagnostic procedures are not exhaustive and may vary depending on your specific case. Your doctor will determine the most appropriate tests based on your symptoms, medical history, and physical examination findings. The results of these diagnostic procedures will guide your doctor in developing an individualized treatment plan to address your vagus nerve pain and improve your overall well-being.
Treatment Options for Vagus Nerve Pain
The treatment of vagus nerve pain in the neck will depend on the underlying cause and severity of symptoms. It is important to consult with a healthcare professional before starting any treatment. Some common treatment options include:
Medications and Drugs
Pain medications, anti-inflammatory drugs, muscle relaxants, or antidepressants may be prescribed to manage pain and alleviate symptoms associated with vagus nerve pain. These should only be taken under medical supervision.
In addition to these medications, there are other drug-based treatment options available. For example, nerve blocks may be used to temporarily numb the vagus nerve and provide relief from pain. These blocks can be performed by injecting local anesthetics or steroids near the affected area.
Furthermore, there are emerging pharmaceutical treatments being researched for vagus nerve pain. Scientists are exploring the potential of novel drugs that target specific receptors in the vagus nerve to modulate its activity and reduce pain. These advancements in pharmacology hold promise for more targeted and effective treatment options in the future.
Physical Therapy and Exercises
A physical therapist can help develop a personalized exercise program to strengthen the neck muscles, improve posture, and alleviate pain. They may also use techniques such as heat or cold therapy, manual therapy, or electrical stimulation to relieve symptoms.
In addition to these traditional physical therapy methods, alternative therapies can also be beneficial in managing vagus nerve pain. For instance, acupuncture, a practice rooted in traditional Chinese medicine, involves the insertion of thin needles into specific points on the body. This technique is believed to stimulate the body’s natural healing processes and promote pain relief.
Another alternative therapy that has gained popularity is chiropractic care. Chiropractors use manual adjustments and spinal manipulation techniques to improve the alignment of the spine and alleviate nerve compression, which can contribute to vagus nerve pain.
Surgical Interventions
In severe cases where conservative treatments have failed, surgical interventions such as nerve decompression, vagus nerve stimulation, or nerve grafts may be considered. These procedures should only be performed by skilled surgeons and after thorough evaluation.
One surgical option is nerve decompression surgery, which involves relieving pressure on the vagus nerve by removing or repositioning surrounding structures that may be compressing it. This can help alleviate pain and restore normal nerve function.
Vagus nerve stimulation (VNS) is another surgical procedure that can be used to manage chronic vagus nerve pain. It involves implanting a device that delivers electrical impulses to the vagus nerve, helping to regulate its activity and reduce pain signals.
In cases where the vagus nerve has been damaged or severed, nerve grafts may be performed. This involves taking a healthy nerve from another part of the body and using it to bridge the gap in the damaged vagus nerve, promoting regeneration and restoring function.
It is important to note that surgical interventions are typically reserved for severe and refractory cases of vagus nerve pain, and the decision to undergo surgery should be carefully considered in consultation with a healthcare professional.
Living with Vagus Nerve Pain
Vagus nerve pain in the neck can often be a chronic condition that requires long-term management. While there is no cure for this condition, there are several strategies that can help improve quality of life:
Living with vagus nerve pain in the neck can be a challenging and complex experience. The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body. It plays a crucial role in regulating various bodily functions, including heart rate, digestion, and even mood. When this nerve becomes irritated or damaged, it can lead to persistent pain and discomfort in the neck.
Pain Management Techniques
Various pain management techniques can provide temporary relief from vagus nerve pain. Applying heat or cold packs to the affected area can help soothe inflammation and reduce discomfort. Additionally, practicing relaxation techniques such as deep breathing exercises or meditation can help calm the nervous system and alleviate pain. Over-the-counter pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), may also be recommended by healthcare professionals to manage pain. However, it is important to consult with a healthcare professional before trying any new pain management techniques to ensure they are safe and appropriate for your specific condition.
Living with chronic pain can be physically and emotionally draining. It is essential to find effective ways to manage pain and improve overall well-being. In addition to medical interventions, incorporating lifestyle changes and home remedies can play a significant role in reducing vagus nerve pain.
Lifestyle Changes and Home Remedies
Maintaining good posture is crucial for individuals with vagus nerve pain in the neck. Poor posture can strain the neck and exacerbate symptoms. Practicing proper ergonomics, such as using an ergonomic chair or adjusting the height of computer screens, can help alleviate stress on the neck and reduce pain. Additionally, avoiding activities that strain the neck, such as heavy lifting or repetitive motions, can prevent further irritation of the vagus nerve.
Stress management techniques can also be beneficial in managing vagus nerve pain. Chronic stress can worsen pain symptoms and contribute to overall discomfort. Engaging in activities that promote relaxation, such as yoga or tai chi, can help reduce stress levels and improve overall well-being. Adopting a healthy diet rich in anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids, can also support pain management and reduce inflammation in the body.
Home remedies can provide additional relief for individuals living with vagus nerve pain. Taking hot showers or applying warm compresses to the neck can help relax tense muscles and alleviate discomfort. Gentle neck stretching exercises, under the guidance of a healthcare professional, can also help improve flexibility and reduce pain.
Psychological Support and Coping Strategies
Living with chronic pain can take a toll on mental and emotional well-being. It is important to seek psychological support to cope with the emotional impact of vagus nerve pain in the neck. Mental health professionals, such as therapists or counselors, can provide guidance and support in managing the psychological challenges associated with chronic pain. Joining support groups or connecting with others who are experiencing similar challenges can also provide a sense of community and understanding.
Practicing coping strategies such as meditation or mindfulness can help individuals develop resilience and manage stress associated with vagus nerve pain. These techniques can help redirect focus away from pain and promote a sense of calm and relaxation. Additionally, engaging in activities that bring joy and fulfillment, such as hobbies or creative outlets, can help improve overall well-being and distract from pain.
In conclusion, living with vagus nerve pain in the neck can be a complex and multifaceted experience. Understanding the causes and symptoms of this condition is crucial for effective management. While there may not be a one-size-fits-all treatment approach, a combination of medical interventions, lifestyle changes, pain management techniques, and psychological support can help individuals find relief and improve their overall well-being. It is important to remember that each person’s experience with vagus nerve pain is unique, and consulting with a healthcare professional is essential for personalized treatment and guidance.
If you’re seeking to deepen your understanding of the vagus nerve and its profound impact on your health, “My Vagus Nerve & Me Book” is an invaluable resource. This comprehensive guide delves into the intricacies of one of the most sophisticated systems in the human body, offering insights into its functions and the role it plays in regulating essential processes like heart rate, digestion, and mental health. Discover natural and artificial methods to stimulate your vagus nerve for improved well-being. Take the first step towards harnessing the power of your vagus nerve by getting your copy of the My Vagus Nerve & Me eBook today.