If you’ve been experiencing unexplained pain or discomfort in your body, it’s important to consider all possible causes. One potential culprit could be vagus nerve pain. Understanding the symptoms of vagus nerve pain can help you determine if this may be the source of your discomfort and guide you in seeking appropriate medical attention. In this article, we will explore the role of the vagus nerve in the body, common symptoms of vagus nerve pain, possible causes, diagnosis methods, treatment options, and strategies for living with this condition.
What is the Vagus Nerve?
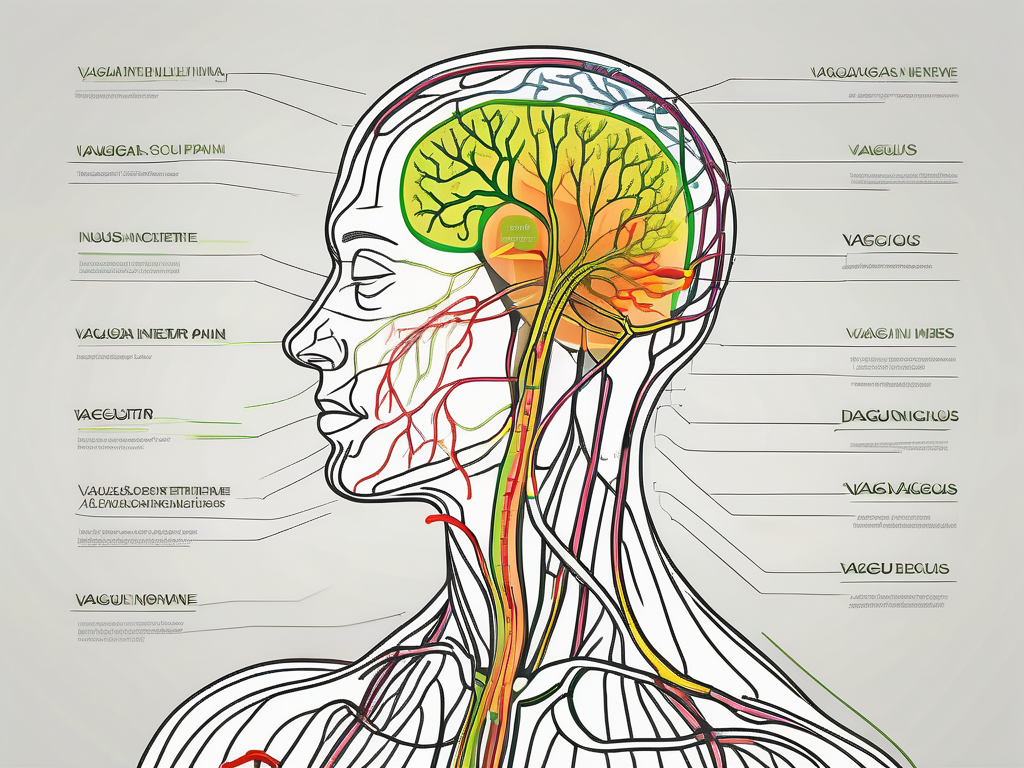
The vagus nerve is one of the cranial nerves, which are a set of nerves that originate in the brain and extend down through the neck and into the body. Also known as the tenth cranial nerve, the vagus nerve is the longest and most complex of the cranial nerves. It reaches various organs in the body, including the heart, lungs, liver, and digestive system.
The vagus nerve, also known as the wandering nerve, derives its name from its extensive and meandering path throughout the body. It branches out like a network of highways, connecting the brain to different organs and systems, ensuring effective communication and regulation.
As a key component of the parasympathetic nervous system, the vagus nerve plays a crucial role in maintaining homeostasis and promoting relaxation. It is often referred to as the “rest and digest” nerve, as it helps regulate bodily functions during periods of rest, relaxation, and digestion.
The Role of the Vagus Nerve in the Body
The vagus nerve plays a vital role in regulating numerous bodily functions, such as heart rate, digestion, and respiratory function. It serves as a communication pathway between the brain and various organs, transmitting signals that control important bodily processes.
When it comes to heart rate regulation, the vagus nerve acts as a natural pacemaker. It helps slow down the heart rate during times of relaxation and rest, promoting a state of calmness and reducing stress levels. Additionally, the vagus nerve influences the release of acetylcholine, a neurotransmitter that helps regulate heart rate and blood pressure.
In terms of digestion, the vagus nerve is responsible for stimulating the production of stomach acid and digestive enzymes, aiding in the breakdown and absorption of nutrients. It also plays a role in regulating the movement of food through the digestive tract, ensuring efficient digestion and absorption.
Furthermore, the vagus nerve is involved in respiratory function, controlling the muscles responsible for breathing. It helps regulate the depth and rate of breathing, ensuring an optimal exchange of oxygen and carbon dioxide in the lungs.
The Anatomy of the Vagus Nerve
The vagus nerve consists of both sensory and motor fibers. The sensory fibers carry information from the body’s organs to the brain, allowing the brain to monitor and regulate their function. On the other hand, the motor fibers carry signals from the brain to the body’s organs, enabling the brain to control their activity.
The sensory fibers of the vagus nerve provide important feedback to the brain, allowing it to constantly monitor the state of the body’s organs. For example, sensory fibers from the digestive system transmit information about the presence of food, acidity levels, and the overall state of digestion. This feedback helps the brain make necessary adjustments to maintain optimal functioning.
Meanwhile, the motor fibers of the vagus nerve carry signals from the brain to the organs, allowing the brain to exert control over their activity. For instance, the brain can increase or decrease heart rate by sending signals through the vagus nerve to the heart. It can also regulate the release of digestive enzymes and control the contraction of smooth muscles in the digestive tract.
The vagus nerve’s intricate anatomy and its extensive connections throughout the body make it a crucial player in maintaining overall health and well-being. Its influence on various bodily functions highlights its significance in ensuring the smooth operation of vital processes.
Identifying Vagus Nerve Pain
Recognizing the symptoms of vagus nerve pain is crucial for getting an accurate diagnosis. The following are some common symptoms associated with vagus nerve pain:
Common Symptoms of Vagus Nerve Pain
- Sharp or stabbing pain in the chest or abdomen
- Difficulty breathing or shortness of breath
- Heart palpitations or irregular heartbeats
- Nausea or vomiting
- Lightheadedness or dizziness
Differences Between Vagus Nerve Pain and Other Pains
Vagus nerve pain can sometimes be confused with other types of pain, such as musculoskeletal pain or pain related to other medical conditions. It is essential to consider the context in which the pain occurs and any accompanying symptoms to differentiate vagus nerve pain from other sources of discomfort. Consulting with a healthcare professional is advised to obtain an accurate diagnosis.
The vagus nerve, also known as the tenth cranial nerve, is one of the longest and most complex nerves in the body. It plays a vital role in regulating various bodily functions, including heart rate, digestion, and breathing. When the vagus nerve becomes irritated or damaged, it can lead to the development of vagus nerve pain.
One of the most common symptoms of vagus nerve pain is a sharp or stabbing pain in the chest or abdomen. This pain can range from mild to severe and may be accompanied by a sense of tightness or pressure. Some individuals may also experience difficulty breathing or shortness of breath, as the vagus nerve is involved in controlling the muscles responsible for respiration.
In addition to chest and abdominal pain, vagus nerve pain can manifest as heart palpitations or irregular heartbeats. This occurs because the vagus nerve helps regulate the heart’s electrical activity. When the nerve is affected, it can disrupt the normal rhythm of the heart, leading to palpitations or irregular beats.
Another symptom commonly associated with vagus nerve pain is nausea or vomiting. The vagus nerve plays a crucial role in controlling the digestive system, and when it is irritated, it can cause a disruption in normal digestion. This can result in feelings of nausea and, in some cases, vomiting.
Lightheadedness or dizziness is also a symptom that may accompany vagus nerve pain. The vagus nerve helps regulate blood pressure and circulation, so when it is affected, it can lead to a drop in blood pressure and a feeling of lightheadedness or dizziness.
It is important to note that vagus nerve pain can sometimes be confused with other types of pain. Musculoskeletal pain, such as that caused by strained muscles or joint inflammation, can sometimes mimic the symptoms of vagus nerve pain. Additionally, pain related to other medical conditions, such as gastrointestinal issues or heart problems, may also present similar symptoms.
To differentiate vagus nerve pain from other sources of discomfort, it is crucial to consider the context in which the pain occurs and any accompanying symptoms. For example, if the pain is primarily felt in the chest or abdomen and is accompanied by difficulty breathing, heart palpitations, or lightheadedness, it may be indicative of vagus nerve pain. However, consulting with a healthcare professional is advised to obtain an accurate diagnosis.
In conclusion, recognizing the symptoms of vagus nerve pain is essential for obtaining an accurate diagnosis. By understanding the common symptoms associated with vagus nerve pain and considering the context in which the pain occurs, individuals can seek appropriate medical attention and treatment for their condition.
Causes of Vagus Nerve Pain
There are various factors that can contribute to vagus nerve pain. Medical conditions related to the vagus nerve and certain lifestyle factors can trigger or exacerbate this type of pain.
The vagus nerve, also known as the tenth cranial nerve, is a crucial component of the autonomic nervous system. It plays a vital role in regulating various bodily functions, including heart rate, digestion, and respiratory rate. When the vagus nerve becomes irritated or damaged, it can result in pain and discomfort.
Medical Conditions Related to Vagus Nerve Pain
Medical conditions such as cervical spondylosis, gastroesophageal reflux disease (GERD), and post-traumatic stress disorder (PTSD) have been linked to vagus nerve pain. Cervical spondylosis is a degenerative condition that affects the cervical spine, potentially causing compression or irritation of the vagus nerve. GERD, a chronic digestive disorder, can lead to acid reflux, which may irritate the vagus nerve. PTSD, a mental health condition triggered by traumatic experiences, can also impact the vagus nerve, contributing to pain symptoms.
In addition to these conditions, other factors such as tumors, infections, and nerve damage can affect the vagus nerve, resulting in pain. Tumors or growths near the vagus nerve can exert pressure on the nerve, leading to discomfort. Infections, such as Lyme disease or viral infections, can cause inflammation and irritation of the nerve. Nerve damage, whether due to injury or certain medical procedures, can disrupt the normal functioning of the vagus nerve, causing pain.
Lifestyle Factors that Can Trigger Vagus Nerve Pain
Stress, anxiety, and certain dietary habits can also contribute to vagus nerve pain. High-stress levels and anxiety can activate the fight-or-flight response, affecting the normal functioning of the vagus nerve. The fight-or-flight response is a natural survival mechanism that prepares the body to either confront or flee from a perceived threat. However, chronic stress or anxiety can lead to overstimulation of the sympathetic nervous system, which can interfere with the vagus nerve’s ability to regulate bodily functions properly.
Furthermore, dietary habits can play a role in vagus nerve pain. Consuming spicy or fatty foods, alcohol, or caffeine in excess can irritate the vagus nerve, potentially triggering pain symptoms. Spicy foods, for example, can cause acid reflux, leading to irritation of the nerve. Excessive alcohol consumption can also contribute to acid reflux and inflammation, further exacerbating vagus nerve pain.
It is important to note that while these factors can contribute to vagus nerve pain, each individual’s experience may vary. Consulting with a healthcare professional is crucial for an accurate diagnosis and appropriate treatment plan.
Diagnosis of Vagus Nerve Pain
Proper diagnosis is essential for determining the underlying cause of vagus nerve pain and developing an appropriate treatment plan. Vagus nerve pain can be a complex condition, and healthcare professionals may employ various medical tests to detect and evaluate it.
One of the common tests used to diagnose vagus nerve pain is an electrocardiogram (ECG). This non-invasive test measures the electrical activity of the heart and can help identify any abnormalities that may be affecting the vagus nerve. By analyzing the ECG results, healthcare providers can gain valuable insights into the functioning of the vagus nerve and its potential role in the pain experienced by the patient.
In addition to an ECG, healthcare professionals may also recommend an upper gastrointestinal endoscopy. This procedure involves inserting a flexible tube with a camera into the esophagus, stomach, and upper small intestine to examine the lining of these organs. By visualizing the area around the vagus nerve, doctors can look for any signs of inflammation, irritation, or other abnormalities that may be causing the pain.
Imaging studies such as magnetic resonance imaging (MRI) or computed tomography (CT) scans can also aid in the diagnosis of vagus nerve pain. These imaging techniques provide detailed images of the structures in the body, allowing healthcare providers to assess the condition of the vagus nerve and surrounding tissues. MRI uses powerful magnets and radio waves to create detailed cross-sectional images, while CT scans use X-rays and computer technology to generate images from different angles.
Understanding Your Diagnosis
Once a diagnosis is made, it is crucial to understand the findings and any underlying conditions contributing to the vagus nerve pain. Your healthcare provider will explain the results of the tests and their implications in detail. It is important to ask questions and seek clarification to ensure a thorough understanding of your condition.
Furthermore, understanding the underlying conditions that may be contributing to vagus nerve pain is essential for developing an appropriate treatment plan. Vagus nerve pain can be caused by various factors, including inflammation, compression, or dysfunction of the nerve. By identifying and addressing these underlying causes, healthcare providers can help alleviate the pain and improve the patient’s quality of life.
During the discussion with your healthcare provider, you may also explore different treatment options available for vagus nerve pain. These can range from conservative approaches such as physical therapy, medication, and lifestyle modifications to more advanced interventions like nerve blocks or surgical procedures. Your healthcare provider will consider various factors, including the severity of your symptoms, underlying conditions, and your overall health, to determine the most suitable treatment plan for you.
Remember, open and effective communication with your healthcare provider is key to understanding your diagnosis and making informed decisions about your treatment. Don’t hesitate to ask questions, express any concerns, and actively participate in your healthcare journey.
Treatment Options for Vagus Nerve Pain
Treatment for vagus nerve pain depends on the underlying cause and severity of symptoms. It may include a combination of medication and non-pharmaceutical therapies. The vagus nerve is a crucial part of the autonomic nervous system, responsible for regulating various bodily functions such as heart rate, digestion, and breathing. When the vagus nerve becomes inflamed or compressed, it can lead to pain and discomfort.
Medications for vagus nerve pain can help alleviate symptoms and improve quality of life. Pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids, may be prescribed to manage the pain. Muscle relaxants can help reduce muscle tension and spasms that may be contributing to the pain. Additionally, healthcare professionals may prescribe medications specifically targeting the symptoms of vagus nerve pain, such as anticonvulsants or antidepressants. However, it is crucial to consult with a doctor before taking any medication to ensure it is suitable for your specific situation. They will consider factors such as your medical history, potential side effects, and possible drug interactions.
In addition to medication, non-pharmaceutical treatments can play a significant role in managing vagus nerve pain. Lifestyle modifications, such as maintaining a healthy diet and regular exercise, can help improve overall well-being and reduce inflammation in the body. Stress management techniques, such as deep breathing exercises, meditation, or yoga, can help calm the nervous system and alleviate symptoms. Physical therapy may be recommended to improve muscle strength, flexibility, and posture, which can help relieve pressure on the vagus nerve.
Complementary therapies, such as acupuncture or chiropractic care, can also be beneficial in managing vagus nerve pain. Acupuncture involves the insertion of thin needles into specific points on the body to stimulate the flow of energy and promote healing. Chiropractic care focuses on the alignment of the spine and musculoskeletal system, aiming to relieve nerve compression and restore proper function. These approaches aim to alleviate symptoms and improve overall well-being.
It is important to work closely with healthcare professionals to develop a comprehensive treatment plan that addresses the underlying cause of vagus nerve pain and targets individual symptoms. They can provide guidance on the most suitable combination of medication and non-pharmaceutical therapies to manage the pain effectively. Regular follow-up appointments and open communication with your healthcare team are essential to monitor progress and make any necessary adjustments to the treatment plan.
Living with Vagus Nerve Pain
Vagus nerve pain can have a significant impact on daily life. It can manifest in various ways, such as sharp, shooting pain or a constant dull ache. This pain can radiate throughout the body, affecting different areas like the neck, throat, chest, and abdomen. The vagus nerve, also known as the “wandering nerve,” is responsible for regulating various bodily functions, including heart rate, digestion, and breathing. When this nerve becomes irritated or damaged, it can lead to chronic pain and discomfort.
Living with vagus nerve pain requires developing coping strategies and embracing long-term management techniques. It is important to remember that what works for one person may not work for another, so it may take some trial and error to find the most effective strategies.
Coping Strategies for Vagus Nerve Pain
Exploring relaxation techniques can be beneficial in managing vagus nerve pain. Deep breathing exercises, for example, can help calm the nervous system and reduce stress levels. By taking slow, deep breaths and focusing on the inhalation and exhalation, individuals can promote relaxation and alleviate pain. Meditation and yoga are also effective practices that can help manage stress and promote overall well-being.
Engaging in activities that bring joy and practicing self-care are equally important in coping with chronic pain. Finding hobbies or activities that distract from the pain can provide a much-needed mental escape. Whether it’s painting, reading, or spending time with loved ones, these activities can help shift the focus away from the pain and improve overall mood.
Long-Term Management of Vagus Nerve Pain
While coping strategies can provide temporary relief, long-term management of vagus nerve pain requires a comprehensive approach. Working closely with healthcare professionals is crucial in developing an effective management plan. These professionals can provide guidance on pain management techniques, suggest appropriate medications, and offer referrals to other specialists if necessary.
Developing healthy lifestyle habits is another essential aspect of long-term care for vagus nerve pain. This includes maintaining a balanced diet, getting regular exercise, and prioritizing sleep. A healthy lifestyle can help reduce inflammation in the body and improve overall well-being, which may alleviate some of the symptoms associated with vagus nerve pain.
Open communication with healthcare professionals is vital in managing vagus nerve pain. Regular check-ups and adjustments to treatment plans may be necessary to ensure ongoing support. It is important to keep track of any changes in symptoms or any new developments and discuss them with your healthcare provider.
In conclusion, living with vagus nerve pain can be challenging, but with the right strategies and support, individuals can improve their quality of life. Coping techniques such as relaxation exercises and engaging in enjoyable activities can help manage the pain on a day-to-day basis. Long-term management involves working closely with healthcare professionals, adopting healthy lifestyle habits, and maintaining open communication about symptom management. By taking a proactive approach to managing vagus nerve pain, individuals can find relief and regain control over their lives.
If you’re seeking to deepen your understanding of the vagus nerve and its profound impact on your health, “My Vagus Nerve & Me Book” is an invaluable resource. Embark on a journey through the complexities of this remarkable system, from its role in regulating essential bodily functions to innovative ways to stimulate it for enhanced well-being. Discover the secrets of your body’s internal processes and learn practical strategies for supporting your vagus nerve health. Ready to unlock the full potential of your vagus nerve? Get My Vagus Nerve & Me eBook today and take the first step towards a harmonious balance of mind, body, and spirit.