Vagus nerve compression in the neck can lead to a range of symptoms that can significantly impact daily life. To better understand these symptoms, it is important to have a clear understanding of the anatomy of the vagus nerve and its role in the body.
Anatomy of the Vagus Nerve
The vagus nerve is one of the longest nerves in the body, stretching from the brainstem all the way down to the abdomen. It is a key component of the parasympathetic nervous system, which regulates involuntary bodily functions, such as heart rate, digestion, and breathing.
The Role of the Vagus Nerve in the Body
As part of the parasympathetic nervous system, the vagus nerve plays a crucial role in maintaining homeostasis and promoting relaxation. It helps to regulate heart rate, controls the muscles responsible for swallowing and speech, and stimulates the release of digestive enzymes.
But the vagus nerve’s influence extends beyond these basic functions. Recent research has shown that it also plays a role in modulating inflammation, stress responses, and even social behavior. The vagus nerve acts as a communication highway between the brain and various organs, allowing for bidirectional signaling and coordination of physiological responses.
For example, studies have found that stimulating the vagus nerve can have anti-inflammatory effects, reducing the production of pro-inflammatory molecules and promoting the release of anti-inflammatory substances. This has led to the development of vagus nerve stimulation as a potential therapy for conditions such as rheumatoid arthritis and inflammatory bowel disease.
Furthermore, the vagus nerve is involved in the body’s stress response system. When activated, it can dampen the release of stress hormones, such as cortisol, and promote a state of relaxation. This has implications for mental health, as chronic stress can contribute to the development of anxiety and depression. Understanding the role of the vagus nerve in stress regulation may lead to new approaches for managing these conditions.
Location and Structure of the Vagus Nerve
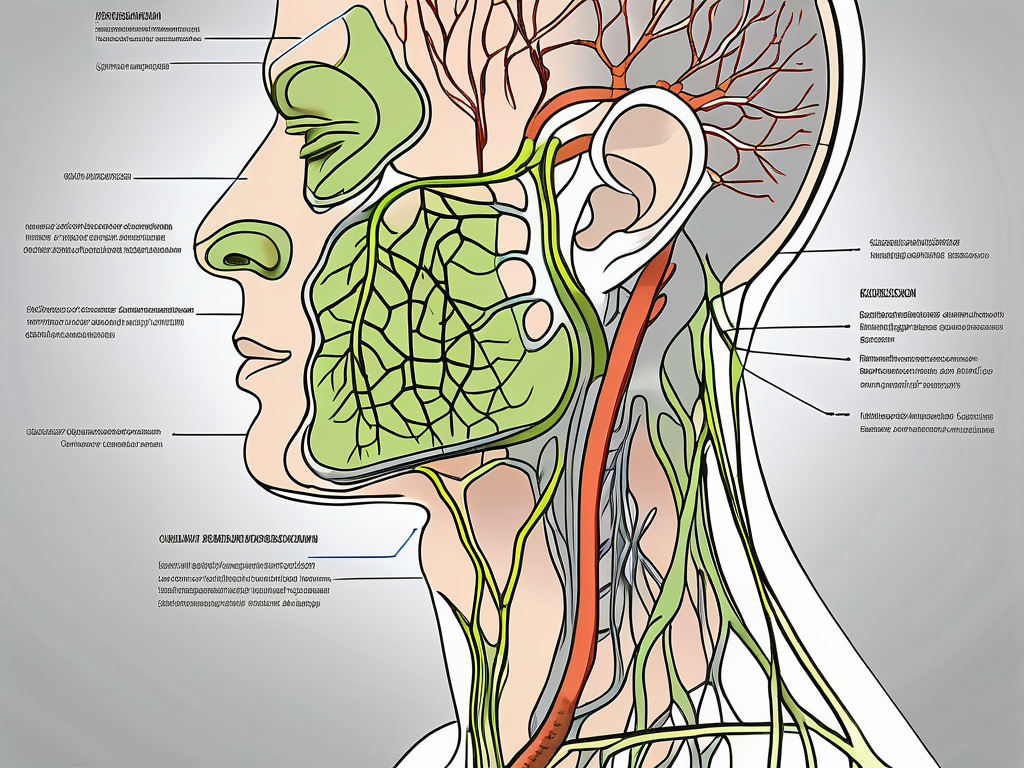
The vagus nerve is a complex structure that travels through various parts of the body. In the neck, it runs alongside the carotid artery, behind the jugular vein, and close to the spinal column. It then branches out to innervate the heart, lungs, digestive system, and other vital organs.
Within the brainstem, the vagus nerve originates from the medulla oblongata, a region responsible for controlling basic life-sustaining functions. From there, it extends downward, sending out numerous branches along its course. These branches innervate different organs and tissues, allowing for precise control and coordination of physiological processes.
Interestingly, the vagus nerve is not a single entity but rather a collection of nerve fibers bundled together. These fibers can be classified into different types based on their function and destination. Some fibers carry sensory information from the organs back to the brain, while others transmit motor signals from the brain to the organs. This intricate network of nerve fibers ensures efficient communication and regulation throughout the body.
In addition to its role in regulating bodily functions, the vagus nerve also interacts with the brain, influencing cognitive processes and emotional states. It forms connections with areas involved in memory, attention, and mood regulation, suggesting that it may play a role in mental well-being.
In conclusion, the vagus nerve is a remarkable structure with far-reaching effects on the body and mind. Its intricate anatomy and diverse functions make it a fascinating subject of study for researchers and medical professionals alike. By unraveling the mysteries of the vagus nerve, we can gain a deeper understanding of how our bodies function and potentially develop new therapies for a range of conditions.
What is Vagus Nerve Compression?
Vagus nerve compression occurs when there is pressure or impingement on the nerve, disrupting its normal functioning. This compression can result from various factors and conditions.
The vagus nerve, also known as the tenth cranial nerve, is a vital component of the autonomic nervous system. It plays a crucial role in regulating various bodily functions, including heart rate, digestion, and breathing. When the vagus nerve is compressed, these functions can be affected, leading to a range of symptoms.
Understanding the causes and risk factors associated with vagus nerve compression is essential for proper diagnosis and treatment.
Causes of Vagus Nerve Compression
There are several possible causes of vagus nerve compression in the neck. These can include trauma, such as whiplash or injury to the neck, as well as anatomical abnormalities, such as bone spurs or herniated discs. In some cases, tumors or infections may also lead to compression of the nerve.
Whiplash, a common injury resulting from sudden acceleration-deceleration forces, can cause the neck structures to move abruptly, potentially leading to vagus nerve compression. Anatomical abnormalities, such as bone spurs or herniated discs, can also exert pressure on the nerve, disrupting its normal function.
Tumors or infections in the neck region can be another cause of vagus nerve compression. These growths can exert pressure on the nerve, leading to symptoms such as difficulty swallowing, hoarseness, or changes in heart rate.
It is important to note that vagus nerve compression can also occur outside the neck region. Compression of the nerve can happen at various points along its pathway, including the chest, abdomen, or pelvis.
Identifying the underlying cause of vagus nerve compression is crucial for determining the most appropriate treatment approach.
Risk Factors for Vagus Nerve Compression
While vagus nerve compression can occur in anyone, there are certain factors that may increase the risk. These can include age, as the nerve may become more vulnerable to compression with age, as well as certain medical conditions, such as arthritis or degenerative disc disease.
As we age, the tissues surrounding the vagus nerve may undergo changes, becoming less flexible and more prone to compression. This can increase the risk of nerve impingement and subsequent symptoms.
Medical conditions that affect the structures around the vagus nerve, such as arthritis or degenerative disc disease, can also contribute to compression. In these conditions, the joints or discs may deteriorate, leading to abnormal pressure on the nerve.
Additionally, individuals who engage in activities or professions that involve repetitive neck movements or prolonged neck flexion may be at a higher risk of developing vagus nerve compression. These activities can strain the neck structures, potentially leading to nerve compression over time.
Understanding the risk factors associated with vagus nerve compression can help individuals take preventive measures and seek early medical intervention if necessary.
Identifying Symptoms of Vagus Nerve Compression
Vagus nerve compression can manifest in a variety of ways, affecting both physical and psychological well-being. The vagus nerve, also known as the “wandering nerve,” is a crucial component of the autonomic nervous system, responsible for regulating various bodily functions.
When the vagus nerve becomes compressed, it can disrupt the normal flow of signals between the brain and the body, leading to a range of symptoms. These symptoms can vary from person to person, depending on the severity and location of the compression.
Physical Symptoms
The physical symptoms of vagus nerve compression can vary from person to person. Common physical symptoms may include difficulty swallowing, hoarseness or voice changes, digestive issues such as nausea or vomiting, and irregular heart rate or palpitations.
Difficulty swallowing, known as dysphagia, can occur when the compression affects the muscles responsible for moving food from the throat to the stomach. This can lead to discomfort and a feeling of food getting stuck in the throat.
Hoarseness or voice changes may result from the compression affecting the vocal cords, which can interfere with the normal vibration required for producing clear speech.
Digestive issues, such as nausea or vomiting, can arise when the vagus nerve compression disrupts the normal functioning of the gastrointestinal tract. The nerve plays a crucial role in regulating digestion, and any disruption can lead to discomfort and digestive disturbances.
Irregular heart rate or palpitations may occur due to the compression affecting the nerve’s control over the heart’s electrical signals. This can result in an abnormal heart rhythm, causing palpitations or a sensation of a racing heart.
Psychological Symptoms
The compression of the vagus nerve can also have psychological effects. Some individuals may experience anxiety, depression, mood swings, or trouble sleeping. These psychological symptoms may be a result of the nerve’s impact on the body’s stress response and emotional regulation mechanisms.
The vagus nerve plays a crucial role in regulating the body’s stress response, known as the fight-or-flight response. When the nerve is compressed, it can disrupt this response, leading to heightened anxiety or an inability to cope with stress effectively.
Furthermore, the vagus nerve is involved in regulating emotional responses and mood. When compressed, it can interfere with the normal regulation of neurotransmitters responsible for mood stability, potentially leading to depressive symptoms or mood swings.
Trouble sleeping, or insomnia, can also be a consequence of vagus nerve compression. The nerve is involved in the regulation of the sleep-wake cycle, and any disruption can result in difficulties falling asleep or staying asleep throughout the night.
In conclusion, vagus nerve compression can have a significant impact on both physical and psychological well-being. It is essential to recognize the symptoms associated with this condition and seek appropriate medical attention for diagnosis and treatment.
The Impact of Vagus Nerve Compression on Daily Life
Vagus nerve compression can significantly impact daily life, affecting both physical health and mental well-being.
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions. It is responsible for controlling the parasympathetic nervous system, which helps maintain balance in the body. When the vagus nerve becomes compressed, it can lead to a range of symptoms that can have a profound impact on a person’s day-to-day activities.
Effects on Physical Health
Physical symptoms associated with vagus nerve compression can limit a person’s ability to eat, speak, or engage in physical activities. Digestive issues, such as difficulty swallowing or a sensation of food getting stuck in the throat, can make mealtimes a challenging and uncomfortable experience. Furthermore, individuals may experience heart rhythm abnormalities, leading to palpitations or a racing heart. These physical symptoms can be distressing and may require medical attention to manage effectively.
In addition to the difficulties with eating and heart rhythm, vagus nerve compression can also affect other bodily functions. It can lead to a decrease in lung function, causing shortness of breath and difficulty breathing. This can significantly impact a person’s ability to engage in physical activities, leading to a sedentary lifestyle and a decline in overall fitness.
Effects on Mental Health
The psychological symptoms resulting from vagus nerve compression can take a toll on an individual’s mental well-being. Anxiety and depression are common among those experiencing vagus nerve compression. The constant physical discomfort and limitations can lead to feelings of frustration, helplessness, and a sense of being trapped within one’s own body.
Furthermore, disrupted sleep patterns are another consequence of vagus nerve compression. The discomfort and pain associated with the condition can make it difficult for individuals to fall asleep or stay asleep throughout the night. This lack of quality sleep can have a significant impact on overall mood, cognitive function, and emotional well-being.
It is essential for individuals experiencing the effects of vagus nerve compression to seek appropriate support from healthcare professionals. Medical interventions, such as physical therapy, medication, or surgical procedures, may be necessary to alleviate the compression and improve symptoms. Additionally, mental health support, such as therapy or counseling, can help individuals cope with the emotional and psychological impact of living with vagus nerve compression.
Diagnostic Procedures for Vagus Nerve Compression
Diagnosing vagus nerve compression typically involves a comprehensive evaluation of medical history and physical examination.
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions, including digestion, heart rate, and breathing. When this nerve is compressed or irritated, it can lead to a range of symptoms such as difficulty swallowing, voice changes, and gastrointestinal issues.
Medical History and Physical Examination
A healthcare professional will take a detailed medical history and ask about the specific symptoms experienced. This information helps in identifying any potential underlying causes of vagus nerve compression, such as previous neck injuries, tumors, or inflammatory conditions.
During the physical examination, the healthcare provider will perform a thorough assessment, focusing on the neck area to assess for any signs of compression or abnormalities. They may gently palpate the neck, checking for tenderness or swelling that could be indicative of nerve compression. Additionally, they may evaluate the patient’s voice quality, swallowing ability, and heart rate variability to gather further clues.
Imaging Tests and Other Diagnostic Tools
In some cases, imaging tests such as an MRI (Magnetic Resonance Imaging) or CT (Computed Tomography) scan may be ordered to further assess the neck, spine, and surrounding structures. These tests can provide more detailed information about the location and extent of nerve compression.
An MRI uses powerful magnets and radio waves to create detailed images of the body’s soft tissues. This non-invasive procedure allows healthcare professionals to visualize the vagus nerve and identify any potential compression or abnormalities. On the other hand, a CT scan utilizes X-rays and computer technology to produce cross-sectional images of the body, providing valuable insights into the bony structures and potential causes of nerve compression.
In addition to imaging tests, other diagnostic tools may be employed to evaluate the function of the vagus nerve. These may include nerve conduction studies, which measure the speed and strength of electrical signals traveling along the nerve, and electromyography, which assesses the electrical activity of muscles innervated by the vagus nerve.
Furthermore, specialized tests such as esophageal manometry, which measures the pressure and movement of the esophagus during swallowing, and laryngoscopy, which examines the structures of the throat and vocal cords, may be utilized to gather more specific information about the impact of vagus nerve compression on swallowing and voice function.
By combining the information obtained from the medical history, physical examination, and diagnostic tests, healthcare professionals can accurately diagnose vagus nerve compression and develop an appropriate treatment plan tailored to the individual patient’s needs.
Treatment Options for Vagus Nerve Compression
The treatment options for vagus nerve compression aim to relieve pressure on the nerve and alleviate associated symptoms. The appropriate treatment will depend on the underlying cause and severity of compression.
Vagus nerve compression can cause a range of symptoms, including difficulty swallowing, hoarseness, heart palpitations, and gastrointestinal issues. These symptoms can significantly impact a person’s quality of life and may require medical intervention to manage effectively.
Non-Surgical Treatments
In many cases, non-surgical treatment options may be recommended initially. These can include physical therapy, pain management techniques, and medications to control symptoms such as pain or inflammation. Physical therapy exercises can help strengthen the muscles surrounding the vagus nerve, reducing pressure and improving nerve function.
Additionally, pain management techniques such as heat therapy, massage, and acupuncture may provide relief from discomfort associated with vagus nerve compression. Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids may be prescribed to reduce inflammation and alleviate pain.
Lifestyle modifications can also play a crucial role in managing vagus nerve compression. Stress reduction techniques, such as meditation, deep breathing exercises, and yoga, can help relax the body and reduce nerve compression symptoms. Dietary changes, such as avoiding trigger foods that may exacerbate symptoms, can also be beneficial.
Surgical Treatments
If non-surgical treatments do not provide significant relief or if the compression is severe, surgical intervention may be necessary. Surgical options may involve decompressing the nerve, removing any tumors or growths, or addressing structural abnormalities in the neck that are causing the compression.
One surgical procedure commonly used to relieve vagus nerve compression is microvascular decompression (MVD). During MVD, a small incision is made behind the ear, and a small pad is placed between the compressed nerve and the blood vessel causing the compression. This procedure aims to relieve pressure on the nerve and restore its normal function.
In cases where tumors or growths are causing the compression, surgical removal may be necessary. The specific approach will depend on the size and location of the growth. Surgeons may opt for minimally invasive techniques, such as endoscopic surgery, whenever possible to minimize scarring and recovery time.
Addressing structural abnormalities in the neck that are causing the compression may involve surgical procedures such as cervical spine fusion or laminectomy. These procedures aim to stabilize the neck and relieve pressure on the vagus nerve.
It is important to note that the choice of surgical treatment will depend on the individual case and the expertise of the medical team. A thorough evaluation of the patient’s condition, including diagnostic imaging and consultations with specialists, will help determine the most appropriate surgical approach.
Prevention and Management of Vagus Nerve Compression
While it may not be possible to prevent all cases of vagus nerve compression, there are steps individuals can take to reduce their risk and manage the condition effectively.
Vagus nerve compression occurs when the vagus nerve, which is responsible for controlling various bodily functions, is compressed or irritated. This can lead to a range of symptoms, including difficulty swallowing, hoarseness, and changes in heart rate.
Adopting a healthy lifestyle can promote overall nerve health. Regular exercise, for example, can improve blood flow and reduce the risk of nerve compression. It is important to engage in activities that strengthen the neck and upper back muscles, as this can help maintain good posture and reduce strain on the vagus nerve.
In addition to exercise, practicing stress-reduction techniques can also be beneficial. Chronic stress can contribute to muscle tension and inflammation, which may increase the risk of nerve compression. Activities such as yoga or meditation can help relax the body and mind, reducing the likelihood of nerve compression.
Furthermore, individuals with known risk factors should take precautions to prevent neck injuries. Wearing seat belts correctly and avoiding excessive strain on the neck during physical activities or heavy lifting can help protect the vagus nerve from compression.
Lifestyle Changes and Home Remedies
Adopting a healthy lifestyle can promote overall nerve health. This can include regular exercise, maintaining good posture, and practicing stress-reduction techniques, such as yoga or meditation. Additionally, individuals with known risk factors should take precautions to prevent neck injuries, such as wearing seat belts correctly and avoiding excessive strain on the neck.
When it comes to managing vagus nerve compression, home remedies can also be helpful. Applying heat or cold packs to the affected area can help reduce inflammation and alleviate symptoms. Gentle neck stretches and exercises recommended by a healthcare professional can also provide relief and prevent further compression of the vagus nerve.
Furthermore, maintaining a healthy diet can support nerve health. Consuming foods rich in vitamins and minerals, such as fruits, vegetables, and whole grains, can provide the necessary nutrients to keep the nerves functioning optimally. Additionally, staying hydrated is essential for overall nerve health.
Regular Check-ups and Monitoring
Regular check-ups with a healthcare professional can help monitor the condition, especially if there are underlying factors that predispose an individual to vagus nerve compression. During these check-ups, the healthcare professional may perform physical examinations, order diagnostic tests, and assess the effectiveness of any ongoing treatment.
Regular monitoring can help detect any changes or complications early on, allowing for timely intervention and management. It is important to communicate any new or worsening symptoms to the healthcare professional, as this can guide the treatment plan and prevent further complications.
In conclusion, understanding the symptoms of vagus nerve compression in the neck is crucial for timely diagnosis and management. If you suspect you may have vagus nerve compression based on the symptoms described, it is important to consult with a healthcare professional who can provide a proper evaluation and recommend appropriate treatment. Remember to always seek medical advice from a trained professional for personalized care and guidance.
If you’re intrigued by the vital role the vagus nerve plays in your health and are seeking to deepen your understanding, “My Vagus Nerve & Me Book” is an essential resource. Discover the complexities of this remarkable system, from regulating your heart rate and digestion to its influence on your mental health. Learn how to nurture your vagus nerve through natural and artificial stimulation, and unlock the secrets to enhancing your overall well-being. Don’t miss out on this opportunity to become an expert on one of the most fascinating aspects of human anatomy. Get My Vagus Nerve & Me eBook today and embark on a journey to optimal health.