Chest pain can be a distressing symptom and is often associated with serious medical conditions. While heart-related causes are commonly considered, it’s important to recognize that chest pain can also stem from other sources, including the vagus nerve. The vagus nerve plays a vital role in the body, and understanding its connection to chest pain can help individuals identify and manage their symptoms effectively.
The Anatomy of the Vagus Nerve
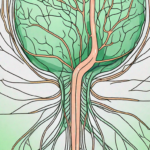
The vagus nerve, formally known as the tenth cranial nerve, is one of the longest nerves in the body. It originates in the brainstem and extends down the neck, passing through the chest and abdomen. This cranial nerve is responsible for controlling various bodily functions, including heart rate, digestion, and even speech.
But let’s dive deeper into the intricate anatomy of the vagus nerve. It is composed of both sensory and motor fibers, allowing it to transmit information from the body to the brain and vice versa. The sensory fibers carry signals from the organs and tissues back to the brain, providing crucial feedback about their functioning. On the other hand, the motor fibers carry signals from the brain to the organs, allowing for the regulation of various bodily functions.
Interestingly, the vagus nerve is not a single structure but rather a complex network of fibers. It consists of both a left and right vagus nerve, which travel alongside each other, branching off into numerous smaller nerve fibers as they traverse the body. These branches innervate different organs and tissues, enabling the vagus nerve to exert its control over a wide range of bodily functions.
The Role of the Vagus Nerve in the Body
The vagus nerve serves as a crucial communication channel between the brain and different organs in the body. It plays a significant role in regulating parasympathetic functions, which help maintain a state of rest and relaxation. This nerve is responsible for controlling heart rate, stimulating digestion, and fostering overall wellbeing.
When it comes to heart rate regulation, the vagus nerve acts as a natural pacemaker. It sends signals to the heart that slow down the heart rate, promoting a sense of calm and relaxation. This is why techniques such as deep breathing and meditation, which stimulate the vagus nerve, can help reduce stress and anxiety.
In terms of digestion, the vagus nerve plays a vital role in stimulating the release of digestive enzymes and promoting the movement of food through the gastrointestinal tract. It helps ensure efficient digestion and absorption of nutrients, contributing to overall digestive health.
Furthermore, the vagus nerve is involved in various other bodily functions, including controlling the muscles responsible for speech and vocalization. It allows us to articulate words and express ourselves verbally, making it an essential component of our communication abilities.
The Connection Between the Vagus Nerve and the Chest
The vagus nerve has branches that innervate the chest region, making it a potential source of chest pain. When the vagus nerve becomes irritated or compressed, it can trigger sensations of discomfort or pain in the chest. Understanding this connection is especially crucial for individuals experiencing unexplained episodes of chest pain.
In addition to chest pain, the vagus nerve’s involvement in the chest region can also lead to other symptoms such as heart palpitations, shortness of breath, and even coughing. These symptoms may arise when there is an imbalance or dysfunction in the vagus nerve signaling, highlighting the intricate relationship between this nerve and the chest.
It is important to note that chest pain can have various causes, and not all cases are related to the vagus nerve. However, understanding the potential role of the vagus nerve in chest pain can help healthcare professionals in their diagnostic process and guide appropriate treatment strategies.
In conclusion, the vagus nerve is a remarkable structure with a wide range of functions in the body. From regulating heart rate and digestion to facilitating speech, this cranial nerve plays a crucial role in maintaining overall health and wellbeing. Its connection to the chest region further emphasizes its significance and highlights the need for further research and understanding in this area.
Identifying Vagus Nerve-Related Chest Pain
Recognizing vagus nerve-related chest pain can be challenging, as it can mimic symptoms of other conditions, such as heart-related problems. However, understanding the specific symptoms associated with vagus nerve-related chest pain can help differentiate it from other causes.
The vagus nerve, also known as the tenth cranial nerve, is a crucial component of the autonomic nervous system. It plays a significant role in regulating various bodily functions, including heart rate, digestion, and breathing. When the vagus nerve becomes irritated or compressed, it can lead to chest pain that may be mistaken for other conditions.
Common Symptoms of Vagus Nerve Chest Pain
In general, vagus nerve-related chest pain often presents as a sharp or aching sensation. It may be accompanied by other symptoms such as shortness of breath, a feeling of heaviness or pressure in the chest, and an increased heart rate. These symptoms may or may not be triggered by certain activities or emotional states.
Furthermore, vagus nerve-related chest pain can sometimes be associated with gastrointestinal symptoms, such as nausea, vomiting, or abdominal discomfort. This connection is due to the close relationship between the vagus nerve and the digestive system. Irritation of the vagus nerve can disrupt the normal functioning of the gastrointestinal tract, leading to additional discomfort.
Differentiating Vagus Nerve Pain from Other Types of Chest Pain
Distinguishing vagus nerve-related chest pain from other types of chest pain can be challenging, as the symptoms can overlap. However, certain factors can help in the differential diagnosis. For example, vagus nerve pain is often not related to physical exertion or exercise, whereas heart-related chest pain may worsen with activity.
Another distinguishing factor is the response to certain triggers. Vagus nerve-related chest pain may be more likely to occur during periods of heightened emotional stress or anxiety. It can also be triggered by certain activities that stimulate the vagus nerve, such as coughing, sneezing, or straining during bowel movements.
Additionally, vagus nerve-related chest pain tends to be more episodic in nature, with intermittent flare-ups rather than a constant, persistent pain. This fluctuating pattern can help differentiate it from other causes of chest pain that may be more consistent in their presentation.
It is important to note that while vagus nerve-related chest pain is generally not life-threatening, it is still essential to seek medical evaluation to rule out other serious conditions. A healthcare professional can conduct a thorough examination, review medical history, and perform diagnostic tests to determine the underlying cause of the chest pain and develop an appropriate treatment plan.
Causes of Vagus Nerve Chest Pain
Several factors can contribute to vagus nerve chest pain. Understanding these causes can assist in managing the symptoms effectively and addressing any underlying issues.
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions, including heart rate, digestion, and breathing. When this nerve becomes irritated or compressed, it can lead to chest pain, which can range from mild discomfort to intense and debilitating sensations.
Medical Conditions Linked to Vagus Nerve Pain
Various medical conditions can irritate or compress the vagus nerve, leading to chest pain. One such condition is gastroesophageal reflux disease (GERD), a chronic digestive disorder characterized by the backflow of stomach acid into the esophagus. The persistent exposure of the esophagus to stomach acid can cause inflammation and irritation, affecting the vagus nerve and resulting in chest pain.
Another medical condition associated with vagus nerve chest pain is hiatal hernia. This occurs when a portion of the stomach pushes through the diaphragm, causing the upper part of the stomach to protrude into the chest cavity. The pressure exerted by the herniated stomach can irritate the vagus nerve, leading to chest pain.
Inflammation of the surrounding structures, such as the esophagus or the tissues around the heart, can also contribute to vagus nerve-related chest pain. Conditions like esophagitis or pericarditis can cause swelling and irritation, affecting the vagus nerve and causing discomfort in the chest area.
Additionally, anxiety and panic disorders can exacerbate vagus nerve-related symptoms. The vagus nerve is closely connected to the parasympathetic nervous system, which is responsible for the body’s rest and digest response. During periods of heightened anxiety or panic, the vagus nerve can become overstimulated, leading to chest pain and other symptoms.
Lifestyle Factors Contributing to Vagus Nerve Chest Pain
Certain lifestyle factors can contribute to vagus nerve-related chest pain. Poor posture, for example, can put unnecessary pressure on the nerves and muscles in the chest area, including the vagus nerve. Slouching or hunching over for extended periods can lead to muscle imbalances and nerve compression, resulting in chest pain.
Excessive stress and inadequate sleep can also contribute to vagus nerve chest pain. Chronic stress can disrupt the body’s natural balance and increase muscle tension, potentially affecting the vagus nerve. Similarly, lack of sleep can impair the body’s ability to recover and repair, leading to heightened sensitivity and increased risk of experiencing chest pain.
A sedentary lifestyle, characterized by prolonged periods of sitting or inactivity, can also contribute to vagus nerve-related symptoms. Regular physical activity helps improve blood circulation, reduce muscle tension, and promote overall well-being. Without sufficient movement, the body may experience increased muscle stiffness and nerve compression, potentially leading to chest pain.
Being aware of these factors and making appropriate changes can potentially alleviate symptoms associated with vagus nerve chest pain. It is important to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan.
Diagnosing Vagus Nerve Chest Pain
Proper diagnosis is crucial for effectively managing vagus nerve-related chest pain and ruling out any serious underlying conditions. Medical professionals employ various methods to identify the cause of the symptoms.
When diagnosing vagus nerve chest pain, medical history and physical examination play a vital role. The healthcare provider will take a detailed medical history, asking about the patient’s symptoms, their duration, and any potential triggers. They will also inquire about the patient’s overall health, including any pre-existing conditions or medications that could contribute to the chest pain.
After gathering the necessary information, the healthcare provider will proceed with a thorough physical examination. This examination may involve palpating the chest area, listening to the patient’s heart and lungs with a stethoscope, and checking for any signs of inflammation or tenderness.
Medical History and Physical Examination
During the diagnostic process, the healthcare provider will evaluate medical history and perform a physical examination. This allows them to gather important information and identify any potential triggers or underlying factors that may contribute to the chest pain.
Additionally, the healthcare provider may ask the patient to describe the chest pain in detail. They may inquire about the pain’s intensity, location, and any accompanying symptoms such as shortness of breath or dizziness. This comprehensive approach helps the healthcare provider gain a better understanding of the patient’s condition and aids in making an accurate diagnosis.
Diagnostic Tests for Vagus Nerve Disorders
In some cases, additional diagnostic tests may be required to confirm the diagnosis of vagus nerve-related chest pain. These tests can include electrocardiograms (ECG), upper endoscopy, esophageal manometry, and imaging studies.
An electrocardiogram (ECG) is a non-invasive test that measures the electrical activity of the heart. It can help determine if the chest pain is cardiac in nature or if it is related to the vagus nerve. This test is particularly useful in ruling out any underlying heart conditions that may be causing the chest pain.
Upper endoscopy is another diagnostic test that may be performed. It involves inserting a thin, flexible tube with a camera into the esophagus to examine the lining of the esophagus, stomach, and upper small intestine. This test can help identify any abnormalities or inflammation that may be contributing to the chest pain.
Esophageal manometry is a test that measures the pressure and movement of the esophagus. It can help determine if there are any abnormalities in the functioning of the esophagus, such as spasms or motility disorders, which may be causing the chest pain.
Imaging studies, such as chest X-rays or CT scans, may also be ordered to get a visual representation of the chest area. These tests can help identify any structural abnormalities or abnormalities in the surrounding organs that may be causing the chest pain.
By conducting these diagnostic tests, healthcare providers can eliminate other potential causes of chest pain and provide a clearer picture of the condition’s origin. This information is crucial for developing an appropriate treatment plan and managing vagus nerve-related chest pain effectively.
Treatment Options for Vagus Nerve Chest Pain
Managing vagus nerve-related chest pain involves addressing the underlying causes and providing relief from discomfort. It’s essential to consult with a healthcare professional to determine the most suitable treatment approach for individual cases.
Vagus nerve chest pain, also known as vagal chest pain, can be a distressing experience. The vagus nerve is a crucial component of the autonomic nervous system, responsible for regulating various bodily functions, including heart rate, digestion, and breathing. When the vagus nerve becomes irritated or inflamed, it can lead to chest pain that may mimic symptoms of a heart attack.
Medications are often prescribed to relieve vagus nerve-related chest pain. These medications can include antacids, acid reducers, and pain relievers. Antacids work by neutralizing stomach acid, which can help reduce the irritation of the vagus nerve. Acid reducers, such as proton pump inhibitors, can also be effective in reducing stomach acid production and alleviating symptoms. Pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help manage any discomfort associated with the chest pain.
However, the specific medication and dosage will depend on the individual’s symptoms and overall health. It is crucial to work closely with a healthcare professional to determine the most appropriate medication regimen.
Non-Pharmacological Interventions for Vagus Nerve Chest Pain
Alongside medications, non-pharmacological interventions can provide additional support in managing vagus nerve-related chest pain. These interventions may include stress management techniques, lifestyle modifications, physical therapy, and relaxation exercises.
Stress management techniques, such as deep breathing exercises, meditation, and mindfulness practices, can help calm the nervous system and reduce vagus nerve irritation. These techniques promote relaxation and can alleviate the intensity and frequency of chest pain episodes.
Lifestyle modifications can also play a significant role in managing vagus nerve chest pain. Avoiding triggers, such as certain foods or activities that exacerbate symptoms, can help prevent episodes of chest pain. Maintaining a healthy diet, regular exercise routine, and adequate sleep can also contribute to overall well-being and reduce the likelihood of experiencing chest pain.
Physical therapy may be recommended to address any musculoskeletal issues that could contribute to vagus nerve chest pain. A physical therapist can provide exercises and stretches to improve posture, strengthen the muscles around the chest and upper back, and alleviate any tension or strain that may be affecting the vagus nerve.
Relaxation exercises, such as progressive muscle relaxation and guided imagery, can help promote a sense of calm and relaxation, reducing the likelihood of vagus nerve irritation. These exercises can be practiced regularly to manage stress and prevent chest pain episodes.
Integrating these non-pharmacological interventions into daily life can help alleviate symptoms and improve overall well-being. It is important to work with a healthcare professional to develop an individualized treatment plan that addresses the specific needs and circumstances of each person experiencing vagus nerve chest pain.
Living with Vagus Nerve Chest Pain
Coping with vagus nerve-related chest pain can be challenging, but there are strategies individuals can employ to improve their quality of life while managing their symptoms effectively.
Living with vagus nerve-related chest pain can be a daily struggle. The pain can range from mild discomfort to intense, sharp sensations that make it difficult to breathe. It’s important for individuals experiencing these symptoms to understand that they are not alone and that there are ways to cope with and manage the pain.
Coping Strategies for Vagus Nerve Pain
Developing effective coping strategies is crucial when living with vagus nerve-related chest pain. These strategies may include practicing relaxation techniques, such as deep breathing exercises or meditation, to help calm the body and reduce stress levels. Engaging in regular physical activity, such as walking or yoga, can also help improve overall well-being and alleviate symptoms.
In addition to physical strategies, maintaining a healthy diet is essential for managing vagus nerve-related chest pain. Avoiding trigger foods, such as spicy foods or caffeine, can help prevent symptom flare-ups. Incorporating foods that are known to have anti-inflammatory properties, such as fruits, vegetables, and omega-3 fatty acids, can also be beneficial.
Seeking emotional support from loved ones is another important coping strategy. Talking to someone who understands and empathizes with the challenges of living with vagus nerve-related chest pain can provide comfort and reassurance. Support groups or therapy sessions can also be helpful in navigating the emotional toll that chronic pain can have on an individual’s mental well-being.
Implementing these coping strategies can help individuals maintain a positive outlook and enhance their overall well-being. It’s important to remember that finding the right combination of strategies may take time and experimentation. What works for one person may not work for another, so it’s essential to be patient and open to trying different approaches.
Preventive Measures to Avoid Vagus Nerve Chest Pain
Taking proactive steps to prevent vagus nerve-related chest pain can significantly reduce the frequency and severity of symptoms. Encouraging healthy lifestyle habits, such as maintaining good posture, can help alleviate pressure on the vagus nerve and minimize discomfort. Practicing good posture not only benefits the vagus nerve but also contributes to overall spinal health.
Reducing stress levels is another important preventive measure. Stress can exacerbate chest pain symptoms, so finding healthy ways to manage stress, such as through exercise, relaxation techniques, or engaging in hobbies, is crucial. Creating a calm and peaceful environment at home can also contribute to stress reduction.
Avoiding trigger foods is another preventive measure that individuals can take. Spicy foods, caffeine, and alcohol are known to stimulate the vagus nerve and can lead to chest pain flare-ups. Being mindful of these triggers and making conscious choices to avoid them can help prevent unnecessary discomfort.
In conclusion, understanding the symptoms of chest pain linked to the vagus nerve is crucial for identifying and managing such discomfort. Although it’s essential to be aware of the potential connection between the vagus nerve and chest pain, consulting with a healthcare professional is paramount for an accurate diagnosis and appropriate treatment. Combining medical guidance with self-care strategies can provide relief and improve the overall quality of life for individuals experiencing vagus nerve-related symptoms.
If you’re intrigued by the vital role the vagus nerve plays in your health and want to delve deeper into its functions and how to care for it, “My Vagus Nerve & Me Book” is the perfect resource. Discover the secrets of one of the most sophisticated systems in the human body and learn practical ways to stimulate your vagus nerve for better health and well-being. From regulating your heart rate to supporting liver detoxification, this book covers it all. Don’t miss the chance to unlock the full potential of your vagus nerve. Get My Vagus Nerve & Me eBook today and take the first step towards a healthier you.