Gastroparesis is a condition that affects the normal movement of food through the stomach. It is often characterized by symptoms such as nausea, vomiting, bloating, and feeling full after eating only small amounts of food. While the exact cause of gastroparesis is not yet fully understood, researchers have identified a potential connection between the vagus nerve and this condition.
An Overview of the Vagus Nerve
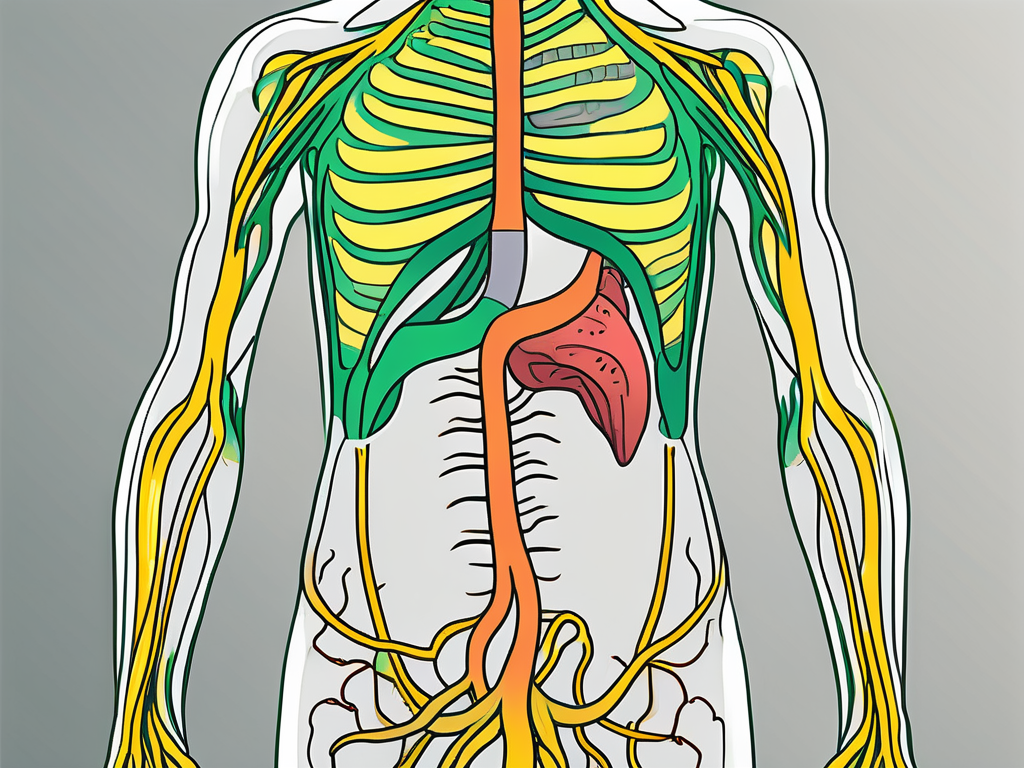
The vagus nerve, also known as the tenth cranial nerve, is one of the longest nerves in the human body. It originates in the brain stem and extends down the neck and into the abdomen, branching to various organs along the way. This nerve plays a crucial role in the regulation of many bodily functions, including heart rate, digestion, and breathing.
Anatomy and Function of the Vagus Nerve
The vagus nerve consists of both sensory and motor fibers. The sensory fibers transmit information from the internal organs back to the brain, allowing us to perceive sensations such as pain or fullness. On the other hand, the motor fibers carry signals from the brain to the organs, controlling their function.
In terms of digestion, the vagus nerve is responsible for transmitting signals that regulate the release of enzymes and acids required for proper food breakdown. It also plays a role in stimulating the contraction of the muscles in the stomach and small intestine, helping propel food through the digestive system.
But the vagus nerve’s involvement in digestion goes beyond these basic functions. It has been found to have a profound impact on our overall digestive health. Research has shown that the vagus nerve is closely linked to the gut microbiome, the complex community of microorganisms that reside in our digestive tract.
The vagus nerve communicates with the gut microbiome through a bidirectional pathway. It sends signals to the gut, influencing the composition and activity of the microbiome. In turn, the gut microbiome produces metabolites and other compounds that can affect the function of the vagus nerve.
The Vagus Nerve’s Role in the Digestive System
When it comes to the digestive system’s functioning, the vagus nerve acts as a critical mediator between the brain and the gastrointestinal tract. It sends signals from the brain to the stomach and intestines, regulating the speed at which food is moved along the digestive tract.
Moreover, the vagus nerve is involved in the complex process of satiety, or feeling full after a meal. It relays information to the brain about the state of the stomach, including its distension and the release of hormones that signal fullness. This feedback loop helps us regulate our food intake and prevent overeating.
Furthermore, the vagus nerve plays a role in the gut-brain axis, a bidirectional communication system between the gut and the brain. This axis allows the gut to send signals to the brain, influencing our mood, emotions, and cognitive function. In fact, the vagus nerve has been implicated in the regulation of anxiety and depression, as well as in the modulation of stress responses.
This communication between the brain and the digestive system is essential for maintaining a healthy and efficient digestive process. However, disruptions in the vagus nerve’s function can lead to various digestive issues, including gastroparesis. Gastroparesis is a condition characterized by delayed stomach emptying, which can cause symptoms such as nausea, vomiting, and bloating.
In conclusion, the vagus nerve is a fascinating and multifaceted component of our body’s intricate systems. Its role in digestion extends beyond basic functions, influencing the gut microbiome, satiety, and the gut-brain axis. Understanding the complexities of the vagus nerve can provide valuable insights into digestive health and pave the way for potential therapeutic interventions.
Exploring Gastroparesis
Gastroparesis is a condition that affects the movement of food through the stomach. In individuals with gastroparesis, the muscles in the stomach do not contract properly, causing food to remain in the stomach for a longer period than usual. This delayed emptying can result in uncomfortable symptoms and complications.
Defining Gastroparesis
Gastroparesis is often characterized by symptoms such as chronic nausea, vomiting, bloating, and a feeling of fullness even after consuming small amounts of food. These symptoms can vary in severity from person to person and may significantly impact an individual’s quality of life.
Gastroparesis can occur as a primary condition, known as idiopathic gastroparesis, or secondary to other underlying medical conditions such as diabetes, autoimmune disorders, or nerve damage.
Common Symptoms and Complications of Gastroparesis
In addition to the symptoms mentioned earlier, individuals with gastroparesis may also experience abdominal pain, acid reflux, weight loss, and malnutrition. The delayed emptying of the stomach can lead to bacterial overgrowth, as food that remains in the stomach for an extended period provides an ideal environment for bacterial growth.
Furthermore, gastroparesis can make it difficult for individuals to manage their blood glucose levels, especially for those with diabetes. The unpredictable digestion of carbohydrates can cause blood sugar fluctuations and make it challenging to plan insulin or medication dosages.
Living with gastroparesis can be challenging, as individuals often have to make significant adjustments to their diet and lifestyle. For example, they may need to eat smaller, more frequent meals to prevent overloading the stomach. It’s also crucial for individuals with gastroparesis to avoid foods that are high in fat and fiber, as these can be difficult to digest and further delay stomach emptying.
Managing gastroparesis often involves a multidisciplinary approach, with healthcare professionals such as gastroenterologists, dietitians, and endocrinologists working together to develop an individualized treatment plan. Medications may be prescribed to help stimulate stomach contractions or control symptoms such as nausea and vomiting.
In severe cases, when conservative treatments fail to provide relief, surgical interventions such as gastric electrical stimulation or feeding tubes may be considered. These interventions aim to improve stomach motility and ensure adequate nutrition.
It’s important for individuals with gastroparesis to work closely with their healthcare team to monitor their symptoms, manage any complications, and make necessary lifestyle modifications. Support groups and online communities can also provide valuable emotional support and practical tips for living with gastroparesis.
Research is ongoing to better understand the underlying causes of gastroparesis and develop more effective treatments. By raising awareness about this condition, we can improve diagnosis rates and enhance the quality of life for individuals living with gastroparesis.
The Vagus Nerve and Gastroparesis Connection
Research suggests that the vagus nerve plays a crucial role in gastroparesis development and progression. In individuals with gastroparesis, the vagus nerve may be damaged or not functioning correctly, leading to the disruption of normal stomach contractions.
How Gastroparesis Affects the Vagus Nerve
It is hypothesized that prolonged high blood sugar levels, such as those experienced by individuals with diabetes, can damage the vagus nerve over time. This damage can impede the nerve’s ability to transmit signals between the brain and the stomach effectively.
Furthermore, the vagus nerve can also be affected by autoimmune disorders. In these cases, the immune system mistakenly attacks the nerve, leading to dysfunction and potential gastroparesis development. Additionally, certain medications, such as opioids, can have a detrimental effect on the vagus nerve, further increasing the risk of gastroparesis.
The Impact of Vagus Nerve Damage on Gastroparesis
Vagus nerve damage can disrupt the coordination of stomach contractions, causing food to move through the digestive system at an abnormal pace. This disrupted motility can result in the characteristic symptoms of gastroparesis, such as nausea, vomiting, and bloating.
Moreover, vagus nerve damage can also affect the release of digestive enzymes and acids essential for breaking down food. The vagus nerve plays a crucial role in stimulating the production and release of these digestive substances. When the nerve is damaged, the production and release of enzymes and acids can be impaired, further hampering the digestive process.
In addition to impaired digestion, vagus nerve damage can also affect the communication between the stomach and the brain. The vagus nerve is responsible for transmitting signals of fullness and satiety from the stomach to the brain. When the nerve is damaged, these signals may not be effectively communicated, leading to a delay in recognizing fullness and potentially contributing to overeating and weight gain.
Furthermore, the vagus nerve is involved in the regulation of inflammation in the digestive system. When the nerve is damaged, the body’s ability to control inflammation in the stomach may be compromised, leading to increased inflammation and further aggravation of gastroparesis symptoms.
In conclusion, the vagus nerve plays a critical role in the development and progression of gastroparesis. Damage or dysfunction of the nerve can disrupt stomach contractions, impair digestion, hinder the communication between the stomach and the brain, and affect the regulation of inflammation. Understanding the connection between the vagus nerve and gastroparesis can provide valuable insights for the development of targeted treatments and interventions for individuals with this condition.
Diagnosis and Treatment
Diagnosing gastroparesis typically involves a combination of medical history evaluations, physical examinations, and specialized tests. A gastric emptying study, where a patient consumes a meal containing a small amount of radioactive material, can provide valuable information about the rate at which food leaves the stomach.
During a gastric emptying study, the patient will be asked to consume the meal, which typically consists of scrambled eggs or oatmeal mixed with a small amount of radioactive material. The radioactive material allows healthcare professionals to track the movement of food through the digestive system using a special camera. This test can help determine if there is delayed emptying of the stomach, which is a common characteristic of gastroparesis.
In addition to the gastric emptying study, healthcare professionals may also perform other tests to further evaluate the underlying cause of gastroparesis. Blood tests may be conducted to check for conditions such as diabetes or thyroid disorders, which can contribute to the development of gastroparesis. Imaging tests, such as an upper gastrointestinal series or an endoscopy, may also be ordered to visualize the stomach and rule out any structural abnormalities.
Identifying Vagus Nerve Damage
Assessing the function of the vagus nerve requires specialized testing. Nerve conduction studies and electrogastrography are among the diagnostic tools that healthcare professionals may use to evaluate vagus nerve integrity and function.
Nerve conduction studies involve the placement of small electrodes on the skin overlying the vagus nerve. These electrodes deliver small electrical impulses to the nerve, and the response is recorded. This test can help determine if there is any damage or dysfunction in the vagus nerve, which plays a crucial role in regulating stomach emptying.
Electrogastrography is another test that can be used to assess the electrical activity of the stomach. During this test, electrodes are placed on the skin of the abdomen to measure the electrical signals generated by the stomach muscles. This can provide valuable information about the coordination and strength of stomach contractions, which are essential for proper digestion.
If vagus nerve damage is suspected, further investigation may be necessary to determine the underlying cause and develop an appropriate treatment plan.
Treatment Options for Gastroparesis Related to Vagus Nerve Damage
Unfortunately, there is no cure for gastroparesis. However, various treatment options can help manage the symptoms and improve overall quality of life.
Dietary modifications, such as consuming smaller, more frequent meals and avoiding high-fat and high-fiber foods, can aid in symptom management. These dietary changes can help reduce the workload on the stomach and make digestion easier. In some cases, a liquid or pureed diet may be recommended to facilitate digestion and ensure adequate nutrition.
Medications can also be prescribed to promote stomach contractions, control nausea and vomiting, and manage other associated symptoms. Prokinetic agents, such as metoclopramide or domperidone, are commonly used to improve the movement of food through the stomach. These medications work by increasing the strength and coordination of stomach contractions, helping to alleviate symptoms of gastroparesis.
In severe cases, where conservative measures and medications fail to provide relief, more invasive interventions may be considered. Gastric electrical stimulation is a surgical procedure that involves implanting a device in the abdomen to deliver electrical impulses to the stomach. This can help regulate stomach contractions and improve gastric emptying. Feeding tube placement may also be considered in cases where oral intake is severely compromised, allowing for the delivery of nutrition directly into the small intestine.
It is important for individuals with gastroparesis to work closely with their healthcare team to develop a comprehensive treatment plan that addresses their specific needs and goals. Regular follow-up appointments and ongoing monitoring are essential to ensure the effectiveness of the chosen treatment approach and make any necessary adjustments.
Prevention and Management
While gastroparesis cannot always be prevented, certain measures can support vagus nerve health and potentially reduce the risk of developing this condition.
Gastroparesis is a condition characterized by delayed emptying of the stomach, which can lead to symptoms such as nausea, vomiting, and bloating. It is often caused by damage to the vagus nerve, which controls the movement of food through the digestive tract.
Lifestyle Changes to Support Vagus Nerve Health
Avoiding prolonged high blood sugar levels is particularly important in preventing gastroparesis. High blood sugar can damage the vagus nerve over time, leading to impaired stomach emptying. Individuals with diabetes should work closely with their healthcare team to manage their blood sugar levels effectively.
In addition to blood sugar control, maintaining a balanced diet is crucial for vagus nerve health. Eating a variety of nutrient-rich foods, including fruits, vegetables, whole grains, and lean proteins, provides the necessary vitamins and minerals for nerve function.
Regular physical activity is also beneficial for vagus nerve health. Exercise helps improve blood flow and oxygenation to the nerves, promoting their overall health and function.
Moreover, managing stress levels through techniques such as meditation, deep breathing exercises, and mindfulness practices can have a positive impact on vagus nerve function. Stress can contribute to inflammation and nerve damage, so finding healthy ways to cope with stress is essential.
Managing Gastroparesis Symptoms in Daily Life
Living with gastroparesis can be challenging, but there are strategies to help manage the symptoms and improve quality of life.
Keeping a food diary can be a helpful tool in identifying trigger foods or behaviors that worsen gastroparesis symptoms. By tracking what you eat and how it affects your symptoms, you can make informed decisions about your diet.
Practicing good chewing habits is another beneficial approach. Chewing food thoroughly and taking smaller bites can make it easier for the stomach to process and empty the food.
Staying adequately hydrated is important for individuals with gastroparesis. Drinking enough fluids can help prevent dehydration and facilitate digestion.
It is important to note that everyone’s experience with gastroparesis is unique, and what works for one individual may not work for another. Consulting with a healthcare professional is crucial for developing an individualized management plan. They can provide guidance on dietary modifications, medications, and other interventions that may be beneficial.
By implementing these lifestyle changes and working closely with healthcare professionals, individuals can support vagus nerve health and effectively manage gastroparesis symptoms, improving their overall well-being and quality of life.
Conclusion
Understanding the role of the vagus nerve in gastroparesis provides insights into the complex relationship between the nervous system and the digestive system. While vagus nerve dysfunction can contribute to gastroparesis, the exact underlying causes of this condition require further research.
Diagnosis and treatment options for gastroparesis continue to evolve, aiming to alleviate symptoms and improve the overall well-being of individuals affected by this condition. Consulting with a healthcare professional is crucial for a comprehensive evaluation and developing an appropriate management plan.
By increasing awareness and understanding of the vagus nerve’s role in gastroparesis, researchers and healthcare professionals can continue to explore new avenues for diagnosis, treatment, and prevention, ultimately improving the lives of those living with this condition.
If you’re fascinated by the vital role the vagus nerve plays in conditions like gastroparesis and want to delve deeper into its functions and impact on your health, “My Vagus Nerve & Me Book” is the perfect resource. Discover the intricacies of this remarkable nerve system, learn about its extensive influence on your body’s operations, and explore ways to stimulate it for better health. Whether you’re dealing with digestive issues, seeking to enhance your mental well-being, or simply curious about the body’s inner workings, this book offers valuable insights. Take the first step towards understanding and optimizing your vagus nerve function. Get My Vagus Nerve & Me eBook today and embark on a journey to better health.