Gastroparesis is a condition that affects the normal movement of food through the stomach. It can lead to various digestive symptoms and can have a significant impact on a person’s quality of life. One important factor in understanding gastroparesis is the role of the vagus nerve.
An Overview of the Vagus Nerve
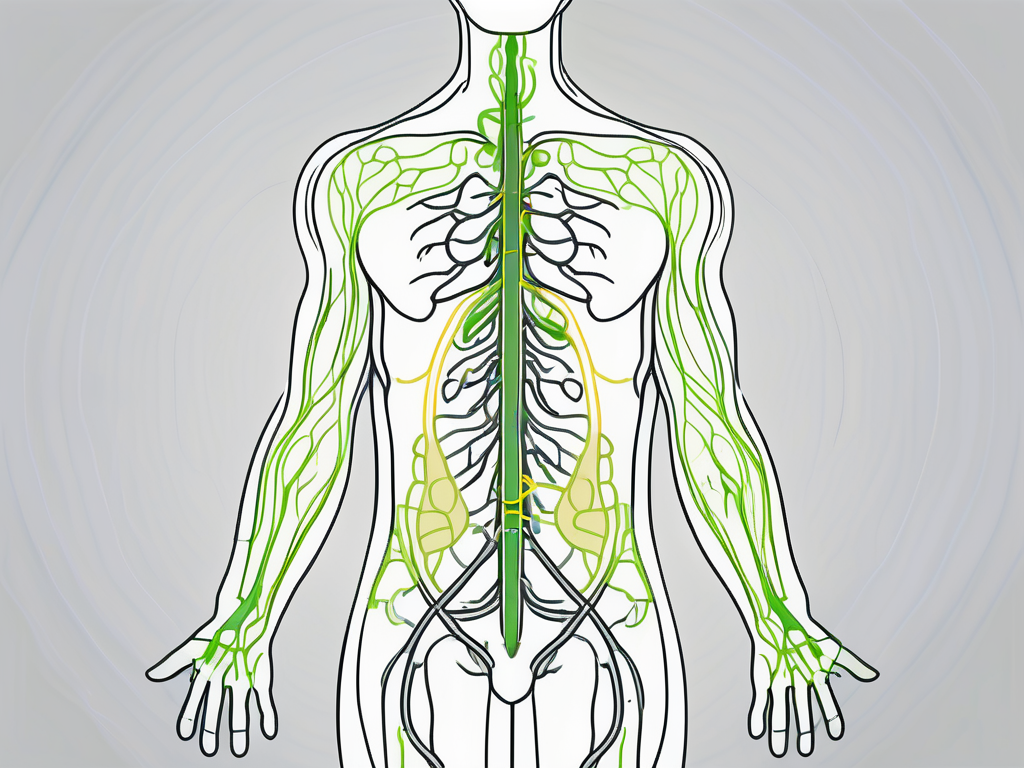
The vagus nerve, also known as the tenth cranial nerve, is one of the longest cranial nerves in our body. It begins in the brainstem and runs down through the neck, chest, and abdomen. This nerve plays a crucial role in regulating various bodily functions, including digestion.
The vagus nerve is a fascinating part of our anatomy, with a complex network of nerve fibers that innervate many organs, including the stomach. It carries signals between the brain and the stomach, controlling the release of digestive juices and regulating gastric motility. Without the vagus nerve, our digestive system would not function properly, leading to various gastrointestinal issues.
Anatomy and Function of the Vagus Nerve
The vagus nerve is like a highway that connects the brain to the stomach, ensuring smooth communication between the two. It is composed of both sensory and motor fibers, allowing it to transmit information from the stomach to the brain and vice versa. This bidirectional communication is crucial for maintaining digestive health.
When we eat, the vagus nerve is responsible for initiating the process of digestion. It helps stimulate the release of stomach acid and digestive enzymes, preparing the body to break down food and extract nutrients. Additionally, the vagus nerve coordinates the rhythmic contractions that move food through the stomach and intestines, ensuring efficient digestion and absorption.
The Vagus Nerve and the Autonomic Nervous System
The vagus nerve is not only involved in digestion but also plays a vital role in the autonomic nervous system. This system is responsible for controlling involuntary bodily functions, such as heart rate, blood pressure, and breathing. The vagus nerve belongs to the parasympathetic division of the autonomic nervous system, which is associated with the body’s “rest and digest” response.
When we eat, the parasympathetic division of the autonomic nervous system becomes active, thanks to the vagus nerve. This activation helps promote digestion by increasing blood flow to the digestive organs, stimulating the secretion of digestive juices, and enhancing nutrient absorption. It also helps relax the muscles of the gastrointestinal tract, allowing food to move smoothly through the digestive system.
Furthermore, the vagus nerve is involved in regulating heart rate and blood pressure. It helps slow down the heart rate and lower blood pressure, promoting a state of relaxation and calmness. This is why techniques such as deep breathing and meditation, which stimulate the vagus nerve, are effective in reducing stress and anxiety.
In addition to its role in digestion and the autonomic nervous system, the vagus nerve has been linked to various other functions and conditions. Research suggests that vagus nerve stimulation may have therapeutic benefits for conditions like epilepsy, depression, and inflammatory diseases. Scientists are still exploring the full extent of the vagus nerve’s capabilities and its potential for medical interventions.
In conclusion, the vagus nerve is a remarkable part of our anatomy, with its extensive reach and diverse functions. From regulating digestion to influencing our overall well-being, this nerve plays a vital role in maintaining our health. Understanding the intricate workings of the vagus nerve can help us appreciate the complexity of our body and its interconnected systems.
The Connection Between the Vagus Nerve and Gastroparesis
Gastroparesis occurs when the vagus nerve is damaged or not functioning correctly. This nerve damage can disrupt the normal signals between the brain and the stomach, leading to delayed gastric emptying and impaired digestion. There are several factors that can contribute to vagus nerve damage and, subsequently, the development of gastroparesis.
One possible cause of vagus nerve damage is diabetes. High blood sugar levels can injure the vagus nerve over time, affecting its ability to transmit signals effectively. This can result in gastroparesis, as the damaged nerve struggles to regulate the stomach’s contractions and emptying process.
Another factor that can lead to vagus nerve damage is surgery. Certain surgical procedures, such as those involving the stomach or esophagus, can inadvertently damage the vagus nerve. This damage can disrupt the communication between the brain and stomach, causing gastroparesis to develop post-surgery.
How Gastroparesis Affects Digestion
When the vagus nerve is damaged, the stomach is unable to contract and empty its contents efficiently. This leads to delayed gastric emptying, causing food to remain in the stomach for a more extended period than usual. As a result, individuals with gastroparesis may experience symptoms such as nausea, vomiting, bloating, and a feeling of fullness even after eating small amounts of food.
In addition to these symptoms, gastroparesis can also lead to nutritional deficiencies. Since food is not being properly digested and absorbed, essential nutrients may not be adequately absorbed by the body. This can result in malnutrition and other related health issues if left untreated.
The Vagus Nerve’s Role in Gastric Motility
Gastric motility refers to the coordinated movements of the stomach muscles that help break down and move food through the digestive system. The vagus nerve plays a vital role in regulating these contractions. When the vagus nerve is damaged, the smooth muscle in the stomach may not contract properly, resulting in impaired gastric motility.
This dysfunction can further contribute to the delayed emptying of the stomach and the development of gastroparesis symptoms. It is important to note that gastroparesis can have various underlying causes, and vagus nerve damage is just one factor that may contribute to its development.
Other potential causes of gastroparesis include viral infections, autoimmune disorders, and certain medications. In some cases, the exact cause of gastroparesis may remain unknown, making treatment and management more challenging.
Overall, understanding the connection between the vagus nerve and gastroparesis is crucial in diagnosing and managing this condition. By addressing the underlying nerve damage and implementing appropriate treatment strategies, individuals with gastroparesis can improve their quality of life and alleviate symptoms.
Symptoms and Diagnosis of Gastroparesis
Gastroparesis, a condition characterized by delayed emptying of the stomach, presents with a range of symptoms that can significantly impact a person’s wellbeing. It is crucial to recognize these symptoms and seek proper medical evaluation for an accurate diagnosis and appropriate management. However, it is essential to remember that only a healthcare professional can diagnose gastroparesis.
Common Symptoms Linked to Vagus Nerve Damage
The symptoms of gastroparesis can vary from person to person but often include nausea, vomiting, early satiety, bloating, and abdominal pain. These symptoms can be intermittent or chronic and may worsen after eating certain foods or during times of stress. The underlying cause of gastroparesis is damage to the vagus nerve, which controls the movement of food through the digestive system. When this nerve is damaged, the muscles in the stomach do not function properly, leading to delayed emptying.
Individuals with gastroparesis may also experience a feeling of fullness even after consuming small amounts of food. This early satiety can be frustrating and may lead to weight loss or malnutrition if not properly managed. Additionally, the persistent nausea and vomiting associated with gastroparesis can significantly impact a person’s quality of life, making it difficult to enjoy meals or engage in social activities.
If you experience these symptoms, it is essential to consult with a healthcare provider to determine their cause and discuss appropriate treatment options. A thorough medical evaluation will help identify the underlying cause of gastroparesis and guide the development of an individualized treatment plan.
Diagnostic Tests for Gastroparesis
To diagnose gastroparesis, a healthcare provider may perform various tests. One commonly used test is a gastric emptying study. In this test, the patient consumes a meal containing a small amount of radioactive material. The healthcare provider will then monitor the movement of the radioactive material through the digestive system to assess gastric emptying time. This test provides valuable information about the rate at which the stomach empties and helps confirm a diagnosis of gastroparesis.
In addition to the gastric emptying study, other diagnostic tests may be used to evaluate the function of the digestive tract and identify any underlying causes contributing to symptoms. Endoscopy, a procedure that uses a flexible tube with a camera to examine the esophagus, stomach, and small intestine, can help identify any structural abnormalities or inflammation. Manometry, a test that measures the pressure and movement of the esophagus and stomach, can provide valuable information about the function of the digestive tract. Electrogastrography, a non-invasive test that measures the electrical activity of the stomach, can also help assess gastric motility and identify any abnormalities.
If you are experiencing symptoms suggestive of gastroparesis, it is crucial to speak with a healthcare provider who can guide you through the appropriate diagnostic process and provide personalized treatment recommendations. Early diagnosis and intervention can help alleviate symptoms and improve overall quality of life for individuals with gastroparesis.
Treatment Options for Gastroparesis
Gastroparesis is a chronic condition that may require long-term management. Treatment options for gastroparesis aim to alleviate symptoms, improve gastric emptying, and enhance overall quality of life. However, it is important to note that treatment plans may vary depending on the individual’s specific needs.
Gastroparesis can significantly impact a person’s daily life, causing discomfort and affecting their ability to eat and digest food properly. Therefore, a multidisciplinary approach is often taken to manage this condition. Treatment options may include a combination of medications, therapies, dietary modifications, and in some cases, surgical interventions.
Medications and Therapies for Gastroparesis
Several medications and therapies can be used to manage gastroparesis symptoms. These may include prokinetic agents, which help improve gastric motility and facilitate stomach emptying. Prokinetic agents work by stimulating the muscles in the stomach to contract more effectively, allowing food to move through the digestive system at a more normal pace.
In addition to prokinetic agents, antiemetics may be prescribed to alleviate nausea and vomiting, which are common symptoms of gastroparesis. These medications work by blocking certain receptors in the brain that trigger the sensation of nausea and the urge to vomit.
Pain medications can also provide relief from abdominal pain associated with gastroparesis. Chronic pain can significantly impact a person’s quality of life, and managing it effectively is an essential aspect of treatment.
In some cases, a healthcare provider may recommend dietary modifications as part of the treatment plan. These modifications may include consuming smaller, more frequent meals to reduce the burden on the stomach and facilitate digestion. Modifying the consistency of the diet, such as consuming softer foods or pureeing meals, can also help ease digestion for individuals with gastroparesis.
Surgical Interventions and the Vagus Nerve
In severe cases of gastroparesis that do not respond to conservative treatments, surgical interventions may be considered. These interventions aim to improve gastric motility and enhance stomach emptying.
One surgical option is gastric electrical stimulation, where small electrical currents are delivered to the stomach to enhance gastric motility. This procedure involves the placement of a device, similar to a pacemaker, that delivers electrical impulses to the stomach muscles, helping them contract more effectively.
Another surgical intervention is pyloroplasty, a procedure that widens the opening between the stomach and small intestine. By enlarging this opening, stomach emptying is improved, allowing food to pass through more easily.
Both gastric electrical stimulation and pyloroplasty may involve manipulation or stimulation of the vagus nerve. The vagus nerve plays a crucial role in regulating digestive function, and by targeting this nerve during surgery, the hope is to improve the overall function of the digestive system.
It is important to remember that surgical interventions are typically considered after comprehensive evaluation and discussion with a healthcare provider. They are not suitable or necessary for all individuals with gastroparesis and should be approached on a case-by-case basis.
In conclusion, treatment options for gastroparesis are diverse and tailored to the individual’s specific needs. Medications, therapies, dietary modifications, and surgical interventions may all play a role in managing symptoms and improving quality of life for individuals with this chronic condition.
The Future of Gastroparesis Research
Ongoing research is shedding light on new treatment options and potential breakthroughs in the management of gastroparesis. Understanding the role of the vagus nerve in gastroparesis is a key area of focus in this research.
Gastroparesis, a condition characterized by delayed gastric emptying, affects millions of people worldwide. It can cause a range of symptoms, including nausea, vomiting, bloating, and early satiety. While current treatment options provide some relief, there is a need for more effective therapies to improve the quality of life for individuals living with gastroparesis.
Emerging Treatments and Their Potential Impact
Researchers are exploring various approaches to improve the symptoms and outcomes of individuals with gastroparesis. This includes investigating new medications that target the vagus nerve to enhance gastric motility or reduce nerve damage. The vagus nerve, also known as the “wandering nerve,” plays a crucial role in regulating various bodily functions, including digestion. By targeting this nerve, researchers hope to restore normal gastric emptying and alleviate the distressing symptoms associated with gastroparesis.
In addition to medication-based treatments, advancements in neuromodulation technologies show promise in improving digestive function and alleviating symptoms in some cases. Vagus nerve stimulation, a technique that involves delivering electrical impulses to the vagus nerve, has shown encouraging results in clinical trials. This non-invasive procedure has the potential to modulate nerve activity and restore normal gastric motility, providing much-needed relief for individuals with gastroparesis.
The Role of the Vagus Nerve in Future Research
Further research on the role of the vagus nerve in gastroparesis will deepen our understanding of the condition and potentially lead to more effective treatment strategies. Scientists are examining the molecular and cellular mechanisms underlying vagus nerve dysfunction in gastroparesis, aiming to develop targeted therapies that restore normal nerve function and improve digestive health.
One area of interest is the exploration of novel drug delivery systems that directly target the vagus nerve. By delivering medications or therapeutic agents specifically to the affected nerve, researchers hope to enhance treatment efficacy and minimize side effects. This targeted approach holds promise for individuals with gastroparesis, as it may provide more precise and personalized treatment options.
Furthermore, advancements in neuroimaging techniques, such as functional magnetic resonance imaging (fMRI), are enabling researchers to visualize and map the activity of the vagus nerve in real-time. This allows for a better understanding of how the nerve functions in individuals with gastroparesis and may uncover new avenues for intervention.
While these advancements in gastroparesis research hold promise, it is essential to consult with a healthcare provider for the most up-to-date information on available treatment options and potential future breakthroughs. Each individual’s condition is unique, and treatment plans should be tailored to their specific needs and circumstances.
In summary, the vagus nerve plays a crucial role in the development and management of gastroparesis. Damage or dysfunction of this nerve can lead to delayed gastric emptying and various digestive symptoms. Proper diagnosis and treatment are essential in managing gastroparesis and improving overall quality of life. If you suspect you may have gastroparesis, it is important to consult with a healthcare professional who can evaluate your symptoms, perform necessary tests, and guide you towards appropriate treatment options.
If you’re fascinated by the critical role the vagus nerve plays in conditions like gastroparesis and want to delve deeper into the wonders of this complex system, “My Vagus Nerve & Me Book” is your essential guide. Discover the intricacies of the vagus nerve, from its impact on your immune system and digestion to its influence on your heart rate and mental health. Learn practical ways to stimulate your vagus nerve, both naturally and artificially, and gain insights into its myriad functions, including liver detoxification and blood sugar regulation. Embark on a journey to better health and understanding. Get My Vagus Nerve & Me eBook today and take the first step towards harnessing the power of your body’s most astonishing system.