Ehlers Danlos Syndrome (EDS) is a complex and rare genetic disorder that affects the body’s connective tissue. This tissue, which is found throughout the body, provides support and structure to organs, blood vessels, and various other tissues. In individuals with EDS, the connective tissue is fragile, leading to a wide range of symptoms and complications.
An Overview of Ehlers Danlos Syndrome
EDS is a group of disorders that have different subtypes, each with its own set of symptoms and genetic causes. The most common subtypes include Classical EDS, Hypermobility EDS, and Vascular EDS. Classical EDS is characterized by hyperelastic skin, joint hypermobility, and easy bruising. Hypermobility EDS is primarily associated with joint hypermobility and chronic pain. Vascular EDS, on the other hand, can lead to life-threatening arterial and organ rupture.
Ehlers Danlos Syndrome (EDS) is a complex and multifaceted condition that affects the connective tissues in the body. It is named after two physicians, Edvard Ehlers and Henri-Alexandre Danlos, who first described the disorder in the early 20th century. EDS is a rare genetic disorder that affects approximately 1 in 5,000 people worldwide. It can manifest in a variety of ways, with each subtype presenting its own unique set of challenges and symptoms.
Defining Ehlers Danlos Syndrome
EDS is caused by mutations in genes responsible for producing collagen, a key component of the connective tissue. Collagen provides strength and elasticity to the tissues, allowing them to withstand stress. In EDS, the abnormal collagen production leads to weak and unstable connective tissue, which can affect various parts of the body.
Collagen is the most abundant protein in the human body and is found in many different tissues, including the skin, tendons, ligaments, blood vessels, and organs. It acts as a scaffold, providing support and structure to these tissues. In individuals with EDS, the collagen fibers are structurally abnormal, leading to a wide range of symptoms and complications.
Symptoms and Diagnosis of Ehlers Danlos Syndrome
The symptoms of EDS can vary widely depending on the subtype, but common features include joint hypermobility, skin abnormalities, chronic pain, and easy bruising. Other complications may include gastrointestinal issues, cardiovascular problems, and weakness of the blood vessels. Diagnosing EDS can be challenging due to the overlapping symptoms with other conditions, but a thorough medical evaluation, family history assessment, and genetic testing are typically used for diagnosis.
Individuals with EDS often experience joint hypermobility, which means that their joints have a greater range of motion than normal. This can lead to frequent joint dislocations and subluxations, causing pain and instability. The skin in EDS patients is often described as “stretchy” or “velvety,” and may be prone to tearing or bruising easily. Chronic pain is a common symptom, affecting both the joints and muscles. Fatigue and weakness are also frequently reported.
Common Treatments for Ehlers Danlos Syndrome
While there is currently no cure for EDS, the management of symptoms and complications plays a crucial role in improving the quality of life for individuals with the condition. Treatment options include physical therapy to strengthen muscles and stabilize joints, pain management strategies, medications for specific symptoms, and lifestyle modifications such as avoiding activities that may exacerbate joint instability.
Physical therapy is an essential component of EDS management, as it helps to improve muscle strength and joint stability. This can reduce the frequency of joint dislocations and subluxations, as well as alleviate pain. Pain management strategies may include the use of nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and other medications to help manage chronic pain. In severe cases, surgical interventions may be necessary to repair damaged joints or address complications such as organ rupture.
Living with Ehlers Danlos Syndrome can be challenging, both physically and emotionally. The unpredictable nature of the condition and the chronic pain it causes can significantly impact an individual’s daily life. Support from healthcare professionals, family, and friends is crucial in managing the condition and maintaining a positive outlook.
The Vagus Nerve Explained
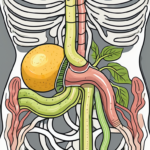
The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body and plays a vital role in the parasympathetic nervous system. It extends from the brainstem to the abdomen and innervates various organs, including the heart, lungs, and digestive system.
The vagus nerve is named after the Latin word “vagus,” meaning “wandering,” because of its extensive distribution throughout the body. It is composed of both motor and sensory fibers, allowing it to transmit signals in both directions.
One of the primary functions of the vagus nerve is to regulate the heart rate. It acts as a brake on the heart, slowing it down and promoting relaxation. This is why deep breathing exercises, which stimulate the vagus nerve, can help reduce heart rate and induce a state of calm.
In addition to its role in cardiovascular regulation, the vagus nerve also plays a crucial role in digestion. It stimulates the release of digestive enzymes and increases intestinal motility, aiding in the breakdown and absorption of nutrients. Dysfunction of the vagus nerve can lead to gastrointestinal disorders such as gastroparesis, a condition characterized by delayed stomach emptying.
Anatomy and Function of the Vagus Nerve
The vagus nerve consists of motor and sensory fibers and is responsible for regulating many essential bodily functions. It controls heart rate, digestion, breathing, and plays a role in the body’s stress response. Additionally, the vagus nerve is involved in the communication between the brain and various organs, helping to maintain overall homeostasis.
The vagus nerve originates in the medulla oblongata, a part of the brainstem, and extends downward, branching out into various regions of the body. It innervates the heart, where it helps regulate heart rate and blood pressure. It also sends branches to the lungs, where it influences breathing patterns and promotes relaxation.
Furthermore, the vagus nerve plays a crucial role in the digestive system. It sends signals to the stomach, liver, and pancreas, stimulating the release of digestive enzymes and promoting optimal digestion. Dysfunction of the vagus nerve can lead to gastrointestinal disorders such as irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD).
The Vagus Nerve and the Autonomic Nervous System
The vagus nerve is a crucial component of the autonomic nervous system, which controls involuntary functions in the body. It works in conjunction with the sympathetic nervous system, responsible for the “fight or flight” response, to maintain a balance between rest and activity, regulation of internal organs, and response to stress.
When the body is under stress, the sympathetic nervous system activates, preparing the body for action. The vagus nerve, on the other hand, acts as a counterbalance, promoting relaxation and restoration. It helps bring the body back to a state of equilibrium by slowing down the heart rate, reducing blood pressure, and promoting digestion.
In addition to its role in stress regulation, the vagus nerve also plays a role in emotional well-being. It is involved in the regulation of mood and has been linked to conditions such as anxiety and depression. Stimulating the vagus nerve through techniques like deep breathing or vagus nerve stimulation (VNS) therapy can have a positive impact on mental health.
Disorders Related to the Vagus Nerve
Disorders related to the vagus nerve can have significant impacts on overall well-being. Dysregulation of vagal nerve function has been associated with conditions such as anxiety, depression, gastrointestinal disorders, and certain cardiovascular conditions. Understanding the role of the vagus nerve in these disorders is an area of active research.
For example, individuals with vagus nerve dysfunction may experience symptoms such as heart palpitations, difficulty swallowing, gastrointestinal disturbances, and mood disorders. Treatment options for vagus nerve disorders include medication, lifestyle modifications, and therapies that target vagal nerve stimulation.
Research is ongoing to explore the potential of vagus nerve stimulation as a therapeutic approach for various conditions. Vagus nerve stimulation has shown promise in the treatment of epilepsy, depression, and even inflammatory conditions like rheumatoid arthritis.
In conclusion, the vagus nerve is a fascinating and essential part of the body’s nervous system. Its extensive distribution and involvement in various bodily functions make it a key player in maintaining overall health and well-being. Understanding the intricate workings of the vagus nerve can lead to new insights and potential treatments for a wide range of disorders.
The Connection Between the Vagus Nerve and Ehlers Danlos Syndrome
Recent studies have shed light on the potential link between Ehlers Danlos Syndrome (EDS) and vagal nerve dysfunction. EDS is a group of genetic disorders that affect the connective tissues in the body, leading to symptoms such as joint hypermobility, skin fragility, and abnormal wound healing. The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions, including heart rate, digestion, and stress response.
Researchers have hypothesized that the abnormal connective tissue seen in EDS may affect the vagus nerve’s structure and function, leading to various symptoms experienced by individuals with EDS. This connection between EDS and vagal nerve dysfunction has sparked interest in the scientific community, as it may provide insights into the underlying mechanisms of EDS and open up new avenues for treatment.
Research Findings on the Vagus Nerve and Ehlers Danlos Syndrome
Studies have shown that individuals with EDS may exhibit autonomic dysfunction, including vagal nerve abnormalities. Autonomic dysfunction refers to the impairment of the automatic processes in the body that are regulated by the autonomic nervous system, which includes the vagus nerve. Dysregulation of heart rate, gastrointestinal motility issues, and abnormal response to stress have been observed in some patients with EDS.
These findings suggest that there may be a direct link between EDS and vagal nerve dysfunction. However, further research is needed to establish a definitive connection and understand the underlying mechanisms.
How Ehlers Danlos Syndrome Affects the Vagus Nerve
The specific mechanisms by which EDS affects the vagus nerve are not yet fully understood. It is hypothesized that the weakened connective tissue in individuals with EDS may impede the proper signaling and communication between the nervous system and the various organs regulated by the vagus nerve.
The vagus nerve is responsible for transmitting signals between the brain and organs such as the heart, lungs, and digestive system. When the connective tissue is compromised in EDS, it may disrupt the normal flow of signals, leading to dysfunction in these organs. This disruption could contribute to the autonomic dysfunction seen in individuals with EDS.
Potential Implications for Treatment
Understanding the role of the vagus nerve in EDS opens up potential avenues for treatment and symptom management. Targeted therapies aimed at improving vagal nerve function and addressing autonomic dysfunction may provide relief for individuals with EDS.
For example, techniques such as vagus nerve stimulation have shown promise in treating various conditions by electrically stimulating the nerve to restore normal function. Additionally, lifestyle modifications, such as stress management techniques and dietary changes, may help alleviate symptoms associated with vagal nerve dysfunction in individuals with EDS.
However, it is crucial to consult with a healthcare professional familiar with EDS and its associated complications before considering any specific treatments. Each individual’s case is unique, and a personalized approach is necessary to ensure the most effective and safe treatment plan.
In conclusion, the connection between the vagus nerve and Ehlers Danlos Syndrome is an area of ongoing research. While studies have shown associations between EDS and vagal nerve abnormalities, further investigation is needed to fully understand the underlying mechanisms and establish a definitive link. The potential implications for treatment are promising, but it is essential to approach any interventions with caution and under the guidance of healthcare professionals.
Future Perspectives in Research and Treatment
As research continues to unravel the complexities of EDS and its connection to the vagus nerve, future perspectives hold promise for improved management and treatment options.
Ongoing Studies on the Vagus Nerve and Ehlers Danlos Syndrome
Researchers are actively investigating the relationship between EDS and vagal nerve dysfunction. Ongoing studies aim to identify specific mechanisms, potential biomarkers, and effective treatment strategies that target the vagus nerve. These studies hold the potential for significant advancements in the understanding and management of EDS.
One area of focus in these ongoing studies is the examination of the role of the vagus nerve in pain perception and modulation. It is believed that dysfunction of the vagus nerve may contribute to the heightened pain sensitivity experienced by individuals with EDS. By understanding the underlying mechanisms, researchers hope to develop targeted therapies that can alleviate pain and improve quality of life for EDS patients.
Another aspect being explored in these studies is the impact of vagal nerve dysfunction on autonomic regulation. The vagus nerve plays a crucial role in regulating various bodily functions, including heart rate, blood pressure, and digestion. Dysfunction of the vagus nerve in EDS patients may contribute to the dysregulation of these autonomic processes. By uncovering the specific mechanisms involved, researchers aim to develop interventions that can restore proper autonomic function in individuals with EDS.
Potential Therapies Targeting the Vagus Nerve
Therapies targeting the vagus nerve are being explored in various medical fields. Vagus nerve stimulation has shown promising results for conditions such as epilepsy and depression. While its potential application in EDS is not yet established, such therapies may offer future possibilities for symptom management.
In addition to vagus nerve stimulation, other emerging therapies are being investigated for their potential in EDS management. For example, bioelectronic medicine, which involves using electrical impulses to modulate neural activity, shows promise in regulating vagal nerve function. By fine-tuning the neural signals within the vagus nerve, bioelectronic medicine may offer a novel approach to managing the symptoms of EDS.
The Future of Ehlers Danlos Syndrome Management
In the future, personalized treatment approaches that take into account an individual’s genetic profile, specific EDS subtype, and associated vagal nerve dysfunction may become a reality. Advancements in genetic research, targeted therapies, and a multidisciplinary approach to EDS management offer hope for improved outcomes and quality of life for individuals living with the syndrome.
One area of research that holds promise for personalized treatment is the identification of genetic modifiers in EDS. While EDS is primarily caused by mutations in specific genes, recent studies have suggested that additional genetic factors may influence the severity and manifestation of the syndrome. By understanding these genetic modifiers, researchers hope to develop tailored treatment approaches that address the unique needs of each individual with EDS.
Furthermore, the integration of various medical specialties in EDS management is gaining recognition. Given the multisystem nature of EDS, a multidisciplinary approach that involves specialists from fields such as genetics, rheumatology, cardiology, and neurology is crucial. This collaborative approach allows for a comprehensive evaluation and management plan that addresses the diverse symptoms and complications associated with EDS.
In conclusion, understanding the role of the vagus nerve in Ehlers Danlos Syndrome opens up new avenues of exploration for improved diagnosis, treatment, and management of this complex disorder. While further research is needed to establish a definitive connection between EDS and vagal nerve dysfunction, the emerging knowledge offers hope for individuals with EDS and highlights the importance of ongoing research efforts in this field. If you suspect you may have Ehlers Danlos Syndrome or have concerns about your health, it is crucial to consult with a healthcare professional familiar with EDS and its associated complications for a proper evaluation and guidance on appropriate management strategies.
If you’re intrigued by the vital role the vagus nerve plays in conditions like Ehlers Danlos Syndrome and want to delve deeper into understanding this remarkable part of your anatomy, the “My Vagus Nerve & Me Book” is an invaluable resource. Discover the extensive influence of the vagus nerve on your body’s systems, learn natural and artificial ways to stimulate it, and explore its significant contributions to your overall health. Embark on a journey of knowledge that could enhance your well-being and provide insights into managing EDS symptoms. Get My Vagus Nerve & Me eBook today and take the first step towards harnessing the power of your body’s most intricate system.