The human body is a complex network of interconnected systems, each playing a crucial role in maintaining our health and well-being. One such system that has garnered increasing attention in recent years is the vagus nerve. This article aims to delve into the intricacies of dorsal vagus nerve shutdown, shedding light on its mechanisms and potential implications for our health.
An Overview of the Vagus Nerve
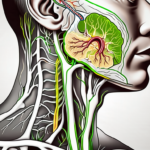
Before diving into the specifics of dorsal vagus nerve shutdown, it is essential to understand the basics of the vagus nerve itself. The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex nerve in our body. It consists of thousands of fibers that originate from the brainstem and innervate various organs in our body, including the heart, lungs, stomach, and intestines.
The Role and Function of the Vagus Nerve
The vagus nerve plays a pivotal role in regulating several bodily functions, earning it the nickname “the wandering nerve.” It is responsible for controlling our heart rate, digestion, respiration, and even plays a role in modulating our mood and emotions. Essentially, the vagus nerve forms a vital connection between our brain and major organs, ensuring their coordinated functioning.
When it comes to heart rate regulation, the vagus nerve acts as a natural pacemaker. It sends signals to the sinoatrial node, a group of specialized cells in the heart, instructing it to slow down or speed up the heart rate as needed. This ability to modulate heart rate is crucial for maintaining cardiovascular health and adapting to various physiological demands.
In terms of digestion, the vagus nerve controls the movement of food through the digestive tract. It stimulates the release of digestive enzymes and promotes the contraction of smooth muscles in the stomach and intestines, facilitating the breakdown and absorption of nutrients. Additionally, the vagus nerve communicates with the brain to regulate feelings of hunger and satiety, helping to maintain a healthy balance in our eating habits.
Respiration is another vital function regulated by the vagus nerve. It influences the rate and depth of our breaths, ensuring an optimal exchange of oxygen and carbon dioxide in the lungs. The vagus nerve also plays a role in controlling the diameter of our airways, helping to prevent airway constriction and maintaining proper lung function.
Interestingly, the vagus nerve extends its influence beyond physiological processes and into the realm of emotions. It is involved in the regulation of mood and emotional responses, with studies suggesting that stimulating the vagus nerve can have antidepressant effects. This connection between the vagus nerve and our emotional well-being highlights the intricate interplay between our mind and body.
The Dorsal and Ventral Vagus: A Comparison
The vagus nerve consists of two main branches: the dorsal and ventral vagus. While both branches share common functions, they differ in their anatomical locations and physiological roles. The dorsal vagus, primarily responsible for shutdown and immobility responses, is located deep within the brainstem, while the ventral vagus exerts more control over social engagement and relaxation responses.
The dorsal vagus, also known as the “old vagus,” is evolutionarily older and more primitive compared to the ventral vagus. It is involved in the freeze response, which is a survival mechanism that allows animals to conserve energy and protect themselves from threats. When activated, the dorsal vagus slows down heart rate, decreases blood pressure, and reduces overall metabolic activity, preparing the body for a state of immobility.
On the other hand, the ventral vagus, also known as the “new vagus,” is responsible for promoting social engagement and relaxation. It is involved in the rest-and-digest response, which occurs when the body feels safe and secure. When the ventral vagus is activated, it promotes feelings of calmness, enhances digestion, and fosters social bonding.
While the dorsal and ventral vagus have distinct roles, they work in harmony to maintain a balance between mobilization and immobilization responses. This delicate interplay ensures that our body can adapt to different situations, whether it’s responding to a threat or engaging in social interactions.
The Concept of Vagus Nerve Shutdown
Now that we have established the foundations of the vagus nerve, let us turn our attention to dorsal vagus nerve shutdown. Vagus nerve shutdown refers to a physiological state in which the dorsal vagus branch becomes less active or completely inactive, leading to a shutdown response in various bodily systems.
Defining Vagus Nerve Shutdown
Vagus nerve shutdown is a natural defense mechanism triggered in response to perceived threats or high-stress situations. When activated, it manifests as a cascade of physiological changes designed to preserve energy and promote survival. This shutdown response can range from mild inhibition to a more pronounced reduction in bodily functions.
During vagus nerve shutdown, the body undergoes a series of intricate processes to ensure its survival. One of the key mechanisms involved is the release of stress hormones, such as cortisol, which plays a crucial role in initiating the shutdown response. These hormones act as messengers, signaling the body to prepare for potential danger.
As the dorsal vagus branch is activated, a series of coordinated events take place within the body. The first noticeable change is a decrease in heart rate, allowing the body to conserve energy and divert resources to more essential functions. Blood pressure also decreases, reducing the strain on the cardiovascular system.
In addition to cardiovascular changes, metabolic activity is significantly reduced during vagus nerve shutdown. This metabolic slowdown helps to conserve energy and prevent unnecessary expenditure. The body redirects its resources to vital survival functions, ensuring that it can endure the perceived threat or stressful situation.
The Biological Process Behind Shutdown
In response to stress or danger, the body releases stress hormones, such as cortisol, which initiates the shutdown response. Activation of the dorsal vagus branch leads to a decrease in heart rate, blood pressure, and metabolic activity while redirecting resources to essential survival functions. This response can also involve reduced social engagement, increased vigilance, and a heightened focus on self-preservation.
During vagus nerve shutdown, the body enters a state of heightened vigilance and self-preservation. It becomes more attuned to potential threats in the environment, scanning for any signs of danger. This increased vigilance allows the individual to react quickly and effectively if the situation escalates.
Furthermore, vagus nerve shutdown can also result in a temporary reduction in social engagement. The body prioritizes self-preservation over social interactions, as it perceives the threat as a higher priority. This withdrawal from social engagement allows the individual to focus solely on their own survival, ensuring that they can navigate the challenging situation effectively.
It is important to note that vagus nerve shutdown is a natural and adaptive response. It is not inherently negative or harmful; rather, it is a mechanism that has evolved over time to ensure the survival of the individual. By conserving energy and redirecting resources to essential functions, the body increases its chances of overcoming the perceived threat or high-stress situation.
In conclusion, vagus nerve shutdown is a complex physiological response that occurs in response to perceived threats or high-stress situations. It involves a cascade of changes in heart rate, blood pressure, metabolic activity, and social engagement. By understanding the biological processes behind vagus nerve shutdown, we can gain insights into the body’s remarkable ability to adapt and survive in challenging circumstances.
The Mechanisms of Dorsal Vagus Nerve Shutdown
To gain deeper insights into dorsal vagus nerve shutdown, it is crucial to examine its mechanisms. From a neurological perspective, the shutdown response involves activation of specific brain regions, such as the amygdala and the periaqueductal gray, which modulate our physiological and emotional responses.
The amygdala, a key player in the shutdown response, is responsible for processing emotions and initiating appropriate behavioral and physiological responses. When a threat is perceived, the amygdala sends signals to the periaqueductal gray, a region involved in pain modulation and defensive behaviors. This activation triggers a cascade of events that ultimately lead to the shutdown of the dorsal vagus nerve.
Neurotransmitters, such as GABA and opioids, play a significant role in regulating the dorsal vagus branch’s activity and the subsequent shutdown response. GABA, an inhibitory neurotransmitter, reduces neuronal excitability and promotes relaxation. Opioids, on the other hand, are known for their pain-relieving properties and can induce a state of calmness and sedation.
When the amygdala and periaqueductal gray are activated, they release GABA and opioids into the dorsal vagus nerve pathway. The activation of these neurotransmitters inhibits neuronal firing and dampens the overall activity of the dorsal vagus, leading to a reduction in bodily functions.
The Neurological Perspective
Understanding the neurological perspective of dorsal vagus nerve shutdown provides valuable insights into the intricate mechanisms underlying this physiological response. The amygdala’s involvement highlights the importance of emotional processing in triggering the shutdown response, as it allows for the appropriate allocation of resources to deal with potential threats.
Furthermore, the role of GABA and opioids in regulating the dorsal vagus activity emphasizes the intricate interplay between neurotransmitters and the nervous system. This delicate balance ensures that the shutdown response is appropriately activated in response to stressors while also preventing excessive or prolonged inactivity of the dorsal vagus.
The Physiological Implications
While dorsal vagus nerve shutdown serves as a protective response in acute stress situations, prolonged or chronic shutdown can have adverse effects on our health. Research suggests that excessive or prolonged inactivity of the dorsal vagus is associated with a heightened risk of cardiovascular disease, gastrointestinal disorders, and compromised immune function.
Cardiovascular disease, in particular, has been linked to reduced vagal tone, which is indicative of decreased activity of the dorsal vagus nerve. The vagus nerve plays a crucial role in regulating heart rate, blood pressure, and overall cardiovascular function. When the dorsal vagus is consistently inactive, these regulatory mechanisms can become dysregulated, increasing the risk of cardiovascular complications.
Gastrointestinal disorders, such as irritable bowel syndrome and functional dyspepsia, have also been associated with impaired dorsal vagus activity. The dorsal vagus nerve is responsible for coordinating various digestive processes, including the secretion of digestive enzymes and the regulation of gut motility. When its activity is compromised, these processes can become disrupted, leading to gastrointestinal symptoms and discomfort.
Furthermore, the dorsal vagus nerve plays a crucial role in modulating immune function. Studies have shown that reduced vagal activity is associated with impaired immune responses, making individuals more susceptible to infections and inflammatory conditions. The immune system relies on the intricate communication between the nervous and immune systems, and when the dorsal vagus is shut down, this communication can be disrupted, compromising immune function.
The Impact of Dorsal Vagus Nerve Shutdown on Health
Understanding the implications of dorsal vagus nerve shutdown on our health is crucial for comprehending its significance. The shutdown response, although designed to protect us, can have both physical and mental health consequences.
The dorsal vagus nerve, also known as the parasympathetic nervous system, plays a vital role in regulating various bodily functions. When faced with a perceived threat or danger, the dorsal vagus nerve initiates a shutdown response, redirecting the body’s energy towards survival mechanisms. While this response is essential for our survival, prolonged shutdown can lead to several physical health consequences.
Physical Health Consequences
Prolonged dorsal vagus nerve shutdown can contribute to a variety of physical health issues. Reduced metabolic activity and altered immune function can increase susceptibility to infections and impair the body’s ability to heal. The body’s natural defense mechanisms, such as the production of immune cells and antibodies, may become compromised, leaving us more vulnerable to illnesses.
Furthermore, decreased cardiovascular function is another consequence of dorsal vagus nerve shutdown. As the body conserves energy during the shutdown response, heart rate and blood pressure decrease. While this response is beneficial in the short term, prolonged shutdown can raise the risk of heart disease and exacerbate existing conditions. The reduced blood flow to vital organs and tissues can compromise their function and lead to long-term health complications.
In addition to the physical health consequences, the implications of dorsal vagus nerve shutdown extend beyond the body’s physiological responses. Mental health is also significantly affected by chronic shutdown.
Mental Health Consequences
Chronic dorsal vagus nerve shutdown can contribute to the development or worsening of mental health disorders, such as anxiety and depression. The constant activation of the shutdown response can disrupt the balance of neurotransmitters in the brain, leading to imbalances that contribute to these disorders. The persistent feeling of fear and hypervigilance associated with shutdown can also contribute to the development of anxiety disorders.
Moreover, reduced social engagement is another consequence of dorsal vagus nerve shutdown. When the shutdown response is activated, our bodies prioritize survival over social interactions. This can lead to decreased motivation and interest in socializing, resulting in feelings of isolation and loneliness. The lack of meaningful social connections can have a detrimental effect on our emotional well-being and overall quality of life.
In conclusion, the impact of dorsal vagus nerve shutdown on health goes beyond the immediate physiological responses. Prolonged shutdown can lead to a range of physical health consequences, including compromised immune function and cardiovascular issues. Additionally, the mental health implications of chronic shutdown can contribute to the development or worsening of anxiety and depression, as well as hinder social interactions. Understanding these consequences is crucial for developing strategies to mitigate the negative effects of dorsal vagus nerve shutdown and promote overall well-being.
Potential Treatments and Interventions
While further research is needed to fully comprehend dorsal vagus nerve shutdown, several potential treatments and interventions have shown promise in modulating vagus nerve activity.
Dorsal vagus nerve shutdown, also known as vagal inhibition, is a condition that occurs when the vagus nerve, a major component of the autonomic nervous system, becomes less active. This can lead to a range of symptoms, including digestive issues, heart rate irregularities, and mood disturbances.
Understanding the underlying mechanisms of dorsal vagus nerve shutdown is crucial for developing effective treatments. Researchers have been exploring various approaches, including medical interventions and lifestyle changes, to modulate vagus nerve activity and restore balance to the autonomic nervous system.
Medical Approaches to Vagus Nerve Stimulation
Vagus nerve stimulation (VNS) is a medical procedure that involves the electrical stimulation of the vagus nerve. It has been approved as a treatment for certain conditions, such as epilepsy and depression. By modulating vagus nerve activity, VNS aims to restore balance and alleviate symptoms associated with dorsal vagus nerve shutdown.
The procedure involves implanting a device, similar to a pacemaker, that delivers electrical impulses to the vagus nerve. These impulses can help regulate the nerve’s activity and promote a more balanced autonomic response. While VNS has shown promising results in certain conditions, its efficacy in treating dorsal vagus nerve shutdown specifically is still being investigated.
Researchers are also exploring non-invasive forms of vagus nerve stimulation, such as transcutaneous vagus nerve stimulation (tVNS). This technique involves applying electrical stimulation to the skin overlying the vagus nerve, stimulating its activity without the need for invasive procedures. tVNS has shown potential in modulating vagus nerve function and may offer a less invasive alternative for those seeking treatment.
Lifestyle Changes and Their Effects on Vagus Nerve Function
In addition to medical interventions, certain lifestyle changes may also help regulate vagus nerve activity. Practices such as regular exercise, stress management techniques, and fostering social connections have been linked to improved vagal tone, promoting a more balanced autonomic nervous system response.
Regular physical activity has been shown to increase vagal tone, leading to enhanced vagus nerve function. Engaging in activities such as aerobic exercise, yoga, and tai chi can help stimulate the vagus nerve and improve its regulation of bodily functions. Additionally, stress management techniques, such as deep breathing exercises and meditation, can activate the relaxation response and promote vagal activity.
Social connections and positive social interactions have also been associated with improved vagus nerve function. Engaging in meaningful relationships, participating in community activities, and practicing empathy and compassion can all contribute to a healthier autonomic nervous system response. These lifestyle changes not only benefit vagus nerve function but also promote overall well-being and mental health.
While lifestyle changes can be beneficial, it is important to note that they may not be sufficient as standalone treatments for dorsal vagus nerve shutdown. Consulting with healthcare professionals and exploring a comprehensive treatment plan that combines medical interventions and lifestyle modifications is recommended for individuals seeking relief from symptoms associated with dorsal vagus nerve shutdown.
Future Research Directions in Vagus Nerve Shutdown
While our understanding of dorsal vagus nerve shutdown has grown significantly, there are still many unanswered questions and areas that warrant further exploration.
The dorsal vagus nerve, also known as the vagus nerve, plays a crucial role in regulating various bodily functions, including heart rate, digestion, and immune response. It is a complex network of nerve fibers that extends from the brainstem to various organs in the body.
Researchers have made significant progress in unraveling the mechanisms underlying dorsal vagus nerve shutdown. However, there are still many unanswered questions that require further investigation.
Unanswered Questions and Potential Studies
Researchers continue to investigate the intricate mechanisms underlying dorsal vagus nerve shutdown. Future studies could explore the interplay between the dorsal and ventral vagus branches, shedding light on how their coordination affects the overall shutdown response.
Understanding the specific triggers and factors that lead to dorsal vagus nerve shutdown is another important area of research. By identifying these triggers, researchers can develop targeted interventions to prevent or mitigate the shutdown response.
Additionally, exploring the long-term effects of shutdown and potential interventions to mitigate its consequences remains an important area of investigation. Understanding how prolonged or repeated shutdown episodes impact overall health and well-being is crucial for developing effective treatment strategies.
Furthermore, investigating the role of genetics and individual differences in the susceptibility to dorsal vagus nerve shutdown could provide valuable insights into personalized approaches for managing this condition.
The Future of Vagus Nerve Research
The field of vagus nerve research is rapidly evolving, opening up new possibilities for understanding and managing dorsal vagus nerve shutdown. Advances in neuroscience and biotechnology hold promising potential for targeted interventions and personalized approaches to mitigate the adverse effects of dorsal vagus nerve shutdown on health.
Emerging technologies, such as optogenetics and bioelectronic devices, offer exciting avenues for modulating vagus nerve activity and restoring normal functioning in individuals experiencing shutdown episodes.
Furthermore, the integration of artificial intelligence and machine learning algorithms can enhance our understanding of the complex interactions between the vagus nerve and various physiological processes. This interdisciplinary approach can help identify novel biomarkers and therapeutic targets for dorsal vagus nerve shutdown.
Moreover, collaborative efforts between researchers, clinicians, and industry partners are essential for translating scientific discoveries into practical applications. By fostering interdisciplinary collaborations, we can accelerate the development of innovative treatments and interventions for individuals affected by dorsal vagus nerve shutdown.
In conclusion, understanding the mechanisms of dorsal vagus nerve shutdown provides valuable insights into the intricate workings of our autonomic nervous system and its impact on our health. While further research is needed, this knowledge can help pave the way for innovative treatments and interventions, offering hope for individuals experiencing the consequences of dorsal vagus nerve shutdown. As always, it is essential to consult with a healthcare professional for personalized advice and guidance.
If you’re fascinated by the vital role the vagus nerve plays in your health and are eager to delve deeper into its functions and the power it holds within your body, “My Vagus Nerve & Me Book” is the perfect resource for you. Discover the secrets of this remarkable system, from regulating your heart rate and digestion to its impact on your immune system and mental health. Learn not only about its extensive functions but also how you can stimulate your vagus nerve both naturally and artificially to enhance your well-being. Take the first step towards harnessing the full potential of your vagus nerve by getting your copy of the My Vagus Nerve & Me eBook today.