Constipation is a common gastrointestinal problem that affects millions of people worldwide. While there are various factors that can contribute to constipation, one emerging area of research is the link between vagus nerve damage and constipation. The vagus nerve, also known as the “wandering nerve,” plays a vital role in the body’s digestive system, and any damage to this nerve can have a profound impact on bowel movements and overall gastrointestinal function.
The Anatomy of the Vagus Nerve
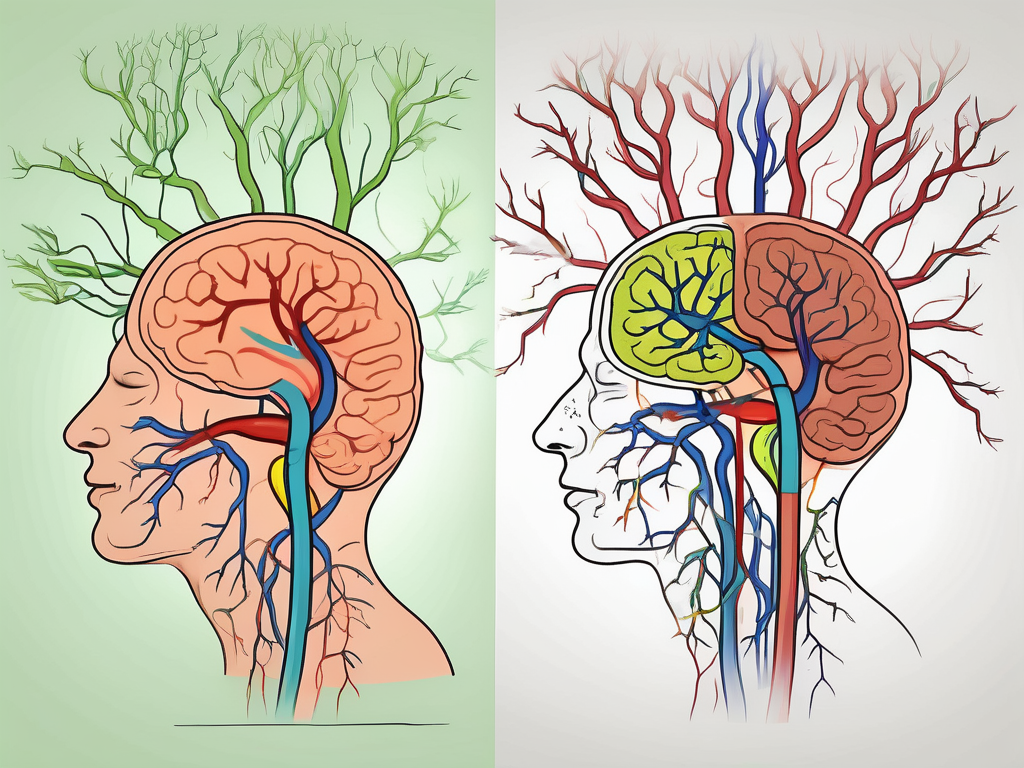
The vagus nerve is the longest cranial nerve in the body and is responsible for numerous important functions. It originates in the brainstem and extends to various organs in the body, including the heart, lungs, stomach, and intestines. This nerve consists of both sensory and motor fibers, making it crucial for both sending signals from the brain to the organs and transmitting information from the organs back to the brain.
The Role of the Vagus Nerve in the Body
The vagus nerve plays a vital role in the parasympathetic nervous system, which promotes rest, relaxation, and digestion. It controls many essential bodily functions, including heart rate, breathing, and digestion. When the vagus nerve is stimulated, it increases gastrointestinal motility, helping the food move through the digestive tract and promoting regular bowel movements.
But the influence of the vagus nerve extends beyond digestion. It also plays a significant role in regulating heart rate. When the body is at rest, the vagus nerve slows down the heart rate, promoting a state of calm and relaxation. On the other hand, when the body is under stress or in a fight-or-flight response, the vagus nerve reduces its activity, allowing the heart rate to increase and preparing the body for action.
In addition to its role in digestion and heart rate regulation, the vagus nerve is involved in controlling the muscles responsible for breathing. It helps regulate the depth and frequency of breaths, ensuring a steady supply of oxygen to the body. This is especially important during moments of physical exertion or when the body needs to increase its oxygen intake.
The Vagus Nerve and the Digestive System
In the digestive system, the vagus nerve controls the movement and contraction of muscles in the esophagus, stomach, and intestines. It also regulates the secretion of digestive enzymes and hormones necessary for proper digestion and nutrient absorption. When the vagus nerve is functioning correctly, it ensures the coordination and smooth operation of the entire digestive process.
But the vagus nerve’s role in the digestive system goes beyond the mechanical aspects of digestion. It also plays a crucial role in the gut-brain axis, which is the bidirectional communication between the gut and the brain. The vagus nerve acts as a messenger, transmitting signals between the gut and the brain, influencing mood, appetite, and even cognitive function.
Furthermore, the vagus nerve is involved in the release of various neurotransmitters and neuropeptides in the gut, such as serotonin and oxytocin. These chemicals not only affect digestion but also play a role in regulating emotions and social behavior. This connection between the vagus nerve, the gut, and the brain highlights the importance of a healthy vagus nerve for overall well-being.
In conclusion, the vagus nerve is a remarkable and multifaceted nerve that plays a crucial role in the body. From regulating heart rate and breathing to controlling digestion and influencing mood, this nerve is involved in numerous essential functions. Understanding the anatomy and functions of the vagus nerve can help us appreciate its significance in maintaining our overall health and well-being.
The Impact of Vagus Nerve Damage
Damage to the vagus nerve can disrupt the communication between the brain and the digestive system, leading to a range of symptoms and complications. Some common causes of vagus nerve damage include surgery, injury, diabetes, and certain medical conditions.
The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body. It extends from the brainstem to the abdomen, innervating various organs along the way, including the heart, lungs, stomach, and intestines. This extensive network allows the vagus nerve to play a crucial role in regulating many bodily functions, including digestion.
Symptoms of Vagus Nerve Damage
Vagus nerve damage can manifest in various ways, depending on the extent and location of the injury. Some common symptoms include difficulty swallowing, heartburn, nausea, bloating, abdominal pain, and changes in bowel movements. Constipation, in particular, is a prevalent symptom associated with vagus nerve damage, as it affects the smooth muscle contractions needed for efficient digestion and elimination.
Aside from gastrointestinal symptoms, vagus nerve damage can also cause issues in other parts of the body. For example, damage to the vagus nerve can lead to a condition called vocal cord paralysis, resulting in hoarseness or difficulty speaking. It can also affect the heart, causing irregular heart rhythms or a decrease in heart rate.
How Vagus Nerve Damage Affects Digestion
When the vagus nerve is damaged, it can disrupt the normal digestive process. The impairment of signals from the brain to the digestive organs can result in slowed gastrointestinal motility, causing food to move more slowly through the intestines. This delayed transit time, combined with reduced muscle contractions, can lead to constipation and difficulty passing stools.
In addition to constipation, vagus nerve damage can also affect the stomach’s ability to produce stomach acid and digestive enzymes. This can result in poor digestion and nutrient absorption, leading to deficiencies in essential vitamins and minerals. Over time, these deficiencies can have a significant impact on overall health and well-being.
Furthermore, vagus nerve damage can disrupt the intricate balance of the gut microbiome, the community of microorganisms that reside in the digestive tract. The vagus nerve plays a crucial role in maintaining the gut-brain axis, a bidirectional communication system between the gut and the brain. When this communication is disrupted, it can lead to dysbiosis, an imbalance in the gut microbiome, which has been linked to various health conditions, including inflammatory bowel disease, obesity, and mental health disorders.
It is important to note that the severity of vagus nerve damage can vary from person to person. Some individuals may experience mild symptoms that resolve over time, while others may require ongoing medical intervention and management. Treatment options for vagus nerve damage may include medication, physical therapy, dietary modifications, and in some cases, surgical interventions.
In conclusion, vagus nerve damage can have a profound impact on digestion and overall health. It is a complex condition that requires careful evaluation and management. If you suspect you may have vagus nerve damage, it is essential to seek medical attention to receive an accurate diagnosis and develop an appropriate treatment plan.
The Connection Between Vagus Nerve Damage and Constipation
The vagus nerve plays a crucial role in regulating bowel movements. It coordinates the rhythmic contractions of the muscles in the intestines, called peristalsis, which helps to propel food through the digestive tract. Damage to the vagus nerve can disrupt this coordination, leading to slowed or irregular peristalsis and ultimately resulting in constipation.
The Role of the Vagus Nerve in Bowel Movements
In normal circumstances, the vagus nerve sends signals to initiate the sequential contractions of the intestinal muscles needed for effective bowel movements. These contractions create a coordinated wave-like movement that facilitates the movement of digested food and waste through the intestines. However, when the vagus nerve is damaged, these contractions become less efficient, leading to decreased motility and constipation.
Imagine the vagus nerve as a conductor, orchestrating the symphony of muscle contractions in the intestines. It ensures that each section of the digestive tract knows when it’s time to contract and when it’s time to relax. This synchronized dance allows for the smooth passage of food and waste, preventing any disruptions in the digestive process.
When the vagus nerve is functioning properly, it sends signals from the brain to the intestines, instructing them to contract in a coordinated manner. This signaling ensures that the muscles contract in a wave-like motion, pushing the food forward and aiding in the efficient absorption of nutrients. It’s like a well-choreographed ballet, where every step is perfectly timed and executed.
How Vagus Nerve Damage Can Lead to Constipation
When the vagus nerve is damaged, the disrupted communication between the brain and the digestive system can result in inadequate muscle contractions in the intestines. This can cause food to move more slowly through the digestive tract, allowing excessive water absorption from the stool. The lack of sufficient muscle contractions and increased water absorption can result in hard, dry stools that are difficult to pass, leading to constipation.
Think of the vagus nerve as a telephone line connecting the brain and the intestines. When this line is damaged, the messages from the brain to the intestines become distorted or lost. It’s like trying to have a conversation with someone over a faulty phone line – the information gets garbled, and the intended message doesn’t reach its destination accurately.
As a result of this communication breakdown, the muscles in the intestines may not receive the proper instructions to contract and relax in a coordinated manner. This leads to a disruption in the natural flow of digestion, causing food to linger in the intestines for longer periods. The longer the food stays in the intestines, the more water gets absorbed, making the stool dry and hard.
Furthermore, the lack of proper muscle contractions can also affect the movement of waste through the colon. The colon relies on rhythmic contractions to propel the stool towards the rectum. When these contractions are weakened due to vagus nerve damage, the stool may become stagnant, leading to further constipation.
In conclusion, the vagus nerve plays a vital role in maintaining regular bowel movements. Damage to this nerve can disrupt the coordination of muscle contractions in the intestines, leading to constipation. Understanding the connection between vagus nerve damage and constipation can help in developing effective treatment strategies to alleviate this common digestive issue.
Diagnosing Vagus Nerve Damage
If you are experiencing symptoms of vagus nerve damage, it is important to seek medical evaluation. A healthcare professional will conduct a thorough assessment to determine the underlying cause and make an accurate diagnosis. The diagnostic process typically involves:
Medical History and Physical Examination
Your healthcare provider will review your medical history and ask about your symptoms, including when they started and any contributing factors. This detailed information helps the healthcare professional understand the context of your symptoms and identify potential triggers or risk factors. Additionally, they will perform a physical examination to check for any signs of nerve damage or other related conditions, such as diabetes or gastrointestinal disorders. During the examination, they may assess your reflexes, muscle strength, and sensation to gather further insights into the functioning of your nervous system.
Diagnostic Tests for Vagus Nerve Damage
In some cases, diagnostic tests may be necessary to confirm vagus nerve damage. These tests aim to provide objective evidence of nerve dysfunction and help guide treatment decisions. One commonly used imaging study is magnetic resonance imaging (MRI), which uses powerful magnets and radio waves to create detailed images of the body’s structures. An MRI can visualize the vagus nerve and identify any abnormalities, such as compression or inflammation. Similarly, a computed tomography (CT) scan may be employed to obtain cross-sectional images of the nerve and surrounding tissues.
Furthermore, nerve conduction studies and electromyography (EMG) tests may be conducted to assess the functionality of the nerves and muscles. Nerve conduction studies involve the placement of small electrodes on the skin to measure the speed and strength of electrical signals as they travel along the vagus nerve. This test can help identify any disruptions or delays in nerve conduction, indicating potential damage. EMG tests, on the other hand, involve the insertion of fine needles into specific muscles to evaluate their electrical activity. By analyzing the muscle response, healthcare professionals can gain insights into the integrity of the nerve-muscle connection.
Additionally, your healthcare provider may recommend other specialized tests based on your specific symptoms and medical history. These could include autonomic function tests to assess the functioning of the autonomic nervous system, which the vagus nerve is a part of. These tests may involve monitoring heart rate variability, blood pressure changes, and sweating responses to various stimuli.
It is important to note that the diagnostic process for vagus nerve damage may vary depending on individual circumstances. Your healthcare provider will determine the most appropriate tests and evaluations based on your unique situation. By conducting a comprehensive assessment, they can accurately diagnose vagus nerve damage and develop an effective treatment plan tailored to your needs.
Treatment Options for Vagus Nerve Damage
The vagus nerve is a crucial component of the nervous system, responsible for regulating various bodily functions. When this nerve is damaged, it can lead to a range of symptoms and complications. The treatment approach for vagus nerve damage depends on the underlying cause and severity of the condition. It is crucial to consult with a healthcare professional to determine the most appropriate treatment plan for your specific case.
There are several treatment options available for vagus nerve damage, each tailored to address the unique needs of the individual. These options may include medications, surgical interventions, or a combination of both.
Medications for Vagus Nerve Damage
In some instances, medications may be prescribed to manage symptoms associated with vagus nerve damage. These medications aim to alleviate pain, reduce nausea, and promote gastrointestinal motility. Pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), may be recommended to help manage any discomfort or pain caused by the nerve damage.
Anti-nausea drugs, such as ondansetron or metoclopramide, may be prescribed to alleviate the sensation of nausea that can occur as a result of vagus nerve damage. These medications work by blocking certain receptors in the brain that trigger the feeling of nausea.
In cases where the damage to the vagus nerve affects gastrointestinal motility, medications that promote movement within the digestive tract may be prescribed. These medications, such as prokinetics, help stimulate the muscles in the digestive system, facilitating the movement of food and waste through the body.
Surgical Treatments for Vagus Nerve Damage
In severe cases of vagus nerve damage that do not respond to conservative treatments, surgical interventions may be considered. These surgical options aim to repair or restore the functionality of the vagus nerve, providing relief from symptoms and improving overall quality of life.
Nerve repair or grafting is a surgical procedure that involves reconnecting or replacing damaged sections of the vagus nerve. This procedure aims to restore the nerve’s functionality and promote proper nerve signaling.
In some cases, the implantation of electrical devices may be recommended to stimulate the vagus nerve and restore its functionality. These devices, known as vagus nerve stimulators, deliver electrical impulses to the nerve, helping to regulate various bodily functions. Vagus nerve stimulation has been shown to be effective in managing conditions such as epilepsy and depression, which are associated with vagus nerve dysfunction.
It is important to note that the decision to undergo surgical treatment for vagus nerve damage should be made in consultation with a healthcare professional. They will assess the individual’s overall health, the severity of the nerve damage, and the potential benefits and risks of the procedure.
In conclusion, treatment options for vagus nerve damage vary depending on the underlying cause and severity of the condition. Medications can help manage symptoms, while surgical interventions aim to repair or restore the functionality of the vagus nerve. Consulting with a healthcare professional is essential to determine the most appropriate treatment plan for each individual case.
Managing Constipation Caused by Vagus Nerve Damage
If you are experiencing constipation due to vagus nerve damage, there are several strategies you can try to alleviate your symptoms. However, it is essential to discuss these strategies with your healthcare provider first to ensure their suitability for your specific situation.
Constipation caused by vagus nerve damage can be a frustrating and uncomfortable condition. It occurs when the vagus nerve, which plays a crucial role in regulating bowel movements, is damaged or impaired. This can lead to a variety of symptoms, including infrequent bowel movements, difficulty passing stools, and abdominal discomfort.
Dietary Changes to Improve Constipation
Adjusting your diet can play a significant role in managing constipation caused by vagus nerve damage. Increasing your fiber intake, drinking plenty of water, and consuming foods rich in probiotics can help promote healthy bowel movements. Fiber acts as a natural bulking agent, adding bulk to the stool and making it easier to pass. Water helps soften the stool, making it easier to move through the digestive system. Probiotics, found in foods like yogurt and sauerkraut, can help regulate gut health and improve digestion.
In addition to these dietary changes, incorporating regular exercise and maintaining a consistent meal schedule can also aid in regulating digestion. Exercise helps stimulate bowel movements by increasing muscle activity in the intestines. A consistent meal schedule can help train your body to expect regular bowel movements, making it easier to establish a routine.
Physical Therapy for Constipation Relief
Physical therapy techniques can be beneficial in managing constipation caused by vagus nerve damage. Abdominal massage, performed by a trained therapist, can help stimulate bowel movements by promoting muscle relaxation and improving blood flow to the intestines. This technique can also help relieve any abdominal discomfort associated with constipation.
Pelvic floor exercises, also known as Kegel exercises, can strengthen the muscles in the pelvic area, including those involved in bowel movements. These exercises can improve muscle coordination and function, making it easier to pass stools. A physical therapist can guide you through the proper technique and provide personalized recommendations based on your specific needs.
It is important to note that while these strategies can be helpful in managing constipation caused by vagus nerve damage, they may not be suitable for everyone. It is always best to consult with your healthcare provider before making any significant changes to your diet or starting a new exercise or physical therapy regimen.
The Future of Vagus Nerve Damage Research
With ongoing advancements in medical research, there is increasing interest in understanding vagus nerve damage and its implications fully. Scientists and healthcare professionals are exploring various treatment modalities and potential interventions that may help alleviate the symptoms associated with vagus nerve damage. Some areas of current research include:
Advances in Vagus Nerve Damage Treatment
Researchers are investigating novel treatment approaches for vagus nerve damage, including techniques to enhance nerve regeneration and promote functional recovery. These advancements aim to develop more effective therapies to restore vagus nerve function and improve overall gastrointestinal health.
The Potential of Vagus Nerve Stimulation
Vagus nerve stimulation (VNS) is a promising area of research for various medical conditions, including vagus nerve damage. This technique involves the use of small electrical impulses to stimulate the vagus nerve and restore its normal function. Ongoing studies aim to explore the potential benefits of VNS as a therapeutic option for individuals with vagus nerve damage and related constipation.
Conclusion
Understanding the link between vagus nerve damage and constipation is crucial for individuals experiencing gastrointestinal symptoms. If you suspect vagus nerve damage may be contributing to your constipation, it is essential to consult with a healthcare professional. They can conduct a comprehensive evaluation, provide an accurate diagnosis, and develop an appropriate treatment plan tailored to your specific needs. By working closely with your healthcare team, you can manage and alleviate the symptoms associated with vagus nerve damage, ultimately improving your quality of life.
If you’re intrigued by the vital role the vagus nerve plays in your health and are seeking to deepen your understanding, “My Vagus Nerve & Me Book” is the perfect resource. Discover the astonishing complexities of this nerve and learn how it influences everything from your digestion to your heart rate. Gain insight into natural and artificial ways to stimulate your vagus nerve for better well-being. Embrace the opportunity to explore its myriad functions, including its contribution to immune system support and mental health. Don’t miss out on this chance to unlock the secrets of one of the most sophisticated systems in your body. Get My Vagus Nerve & Me eBook today and take the first step towards enhancing your vagus nerve health!