The connection between the vagus nerve and autoimmune disease has been the subject of much research and speculation. In this article, we will explore the intricacies of this link and examine the current scientific understanding of the role the vagus nerve plays in autoimmune diseases. While this article provides valuable information, it is important to consult with a qualified healthcare provider for individual medical advice.
Exploring the Vagus Nerve: An Overview
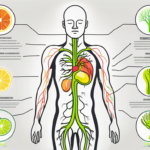
The vagus nerve is one of the longest nerves in the body, stretching from the brainstem to the abdomen. It is a key component of the parasympathetic nervous system, which controls many of the body’s essential functions, including heart rate, digestion, and immune response.
The vagus nerve is responsible for transmitting signals between the brain and various organs, helping to regulate their activity. Its name, “vagus,” comes from the Latin word for “wandering,” reflecting its extensive distribution throughout the body.
As we delve deeper into the fascinating world of the vagus nerve, we uncover its intricate role in maintaining our overall well-being.
The Role and Function of the Vagus Nerve
The primary function of the vagus nerve is to regulate the body’s rest-and-digest response, promoting relaxation and recovery. It slows heart rate, increases digestive activity, and facilitates the release of neurotransmitters that promote calmness and well-being.
But the wonders of the vagus nerve do not end there. Recent studies have revealed that this remarkable nerve also plays a critical role in modulating the immune response. It communicates with immune cells, releasing anti-inflammatory signals that help regulate the body’s immune system.
Imagine the vagus nerve as a conductor, orchestrating a symphony of bodily functions, ensuring harmony and balance within our internal systems.
Anatomy of the Vagus Nerve
The vagus nerve consists of both sensory and motor fibers. The sensory fibers transmit information from various organs, such as the heart and lungs, to the brain. These signals provide the brain with vital feedback about the state of our internal environment.
On the other hand, the motor fibers send signals from the brain to the organs, influencing their function. This bidirectional communication allows the vagus nerve to fine-tune the activity of our organs, ensuring optimal performance.
Furthermore, the vagus nerve consists of multiple branches, each responsible for different functions. These branches include the auricular branch (ear), pharyngeal branch (throat), superior and inferior cardiac branches (heart), pulmonary branches (lungs), and abdominal branches (digestive system).
Each branch of the vagus nerve plays a unique role in maintaining the delicate balance of our bodily functions. It is truly remarkable how this single nerve can have such a widespread impact on our overall health and well-being.
As we continue our exploration of the vagus nerve, we uncover even more fascinating details about its intricate connections and the profound influence it has on our daily lives.
The Intricacies of Autoimmune Diseases
Autoimmune diseases are a complex group of disorders in which the immune system mistakenly attacks the body’s own cells and tissues. It can affect various organs and systems, leading to a wide range of symptoms.
Defining Autoimmune Diseases
In autoimmune diseases, the immune system fails to recognize certain cells or tissues as “self” and instead perceives them as foreign invaders. This triggers an immune response, resulting in inflammation and tissue damage. Examples of autoimmune diseases include rheumatoid arthritis, lupus, multiple sclerosis, and type 1 diabetes.
Research into the causes of autoimmune diseases is ongoing, but genetic factors, environmental triggers, and dysregulation of the immune system are thought to play a role.
Common Types of Autoimmune Diseases
Autoimmune diseases can affect a wide range of organs and tissues, each with its own set of symptoms and complications. Rheumatoid arthritis, for example, primarily affects the joints, leading to pain, swelling, and stiffness. Lupus, on the other hand, can affect multiple organs, including the skin, joints, kidneys, and heart.
Other common autoimmune diseases include psoriasis, celiac disease, inflammatory bowel disease (IBD), Hashimoto’s thyroiditis, and Grave’s disease.
Psoriasis is a chronic autoimmune condition that primarily affects the skin. It is characterized by red, scaly patches that can be itchy and painful. These patches can appear anywhere on the body, but are most commonly found on the elbows, knees, scalp, and lower back. In severe cases, psoriasis can also affect the nails, causing them to become thick, pitted, and discolored.
Celiac disease is an autoimmune disorder that affects the small intestine. It is triggered by the consumption of gluten, a protein found in wheat, barley, and rye. When individuals with celiac disease consume gluten, their immune system reacts by attacking the lining of the small intestine. This can lead to a range of symptoms, including abdominal pain, diarrhea, bloating, and weight loss.
Inflammatory bowel disease (IBD) is a term used to describe a group of chronic inflammatory conditions that affect the digestive tract. The two main types of IBD are Crohn’s disease and ulcerative colitis. Crohn’s disease can affect any part of the digestive tract, from the mouth to the anus, and can cause a variety of symptoms, including abdominal pain, diarrhea, fatigue, and weight loss. Ulcerative colitis, on the other hand, primarily affects the colon and rectum, leading to symptoms such as bloody diarrhea, abdominal pain, and a frequent urge to have a bowel movement.
Hashimoto’s thyroiditis is an autoimmune disorder that affects the thyroid gland. It is characterized by inflammation of the thyroid, which can lead to an underactive thyroid (hypothyroidism). Symptoms of Hashimoto’s thyroiditis can vary, but may include fatigue, weight gain, depression, constipation, and dry skin.
Grave’s disease is an autoimmune disorder that affects the thyroid gland as well, but in this case, it leads to an overactive thyroid (hyperthyroidism). Symptoms of Grave’s disease can include weight loss, rapid heartbeat, anxiety, irritability, tremors, and an enlarged thyroid gland (goiter).
The Connection Between the Vagus Nerve and Autoimmune Diseases
Emerging research suggests that the vagus nerve is intimately involved in the modulation of the immune response, making it a potential key player in autoimmune diseases.
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It originates in the brainstem and extends down to various organs in the body, including the heart, lungs, liver, and gastrointestinal tract. While traditionally known for its role in regulating heart rate and digestion, recent studies have shed light on its influence on the immune system.
The Vagus Nerve’s Influence on Immune Response
The vagus nerve communicates with immune cells through neurotransmitters, such as acetylcholine, to regulate inflammation and immune activity. This bidirectional communication between the nervous system and immune system is known as the neuroimmune axis.
When the immune system detects a threat, it triggers an inflammatory response to eliminate the invading pathogens or damaged cells. However, an excessive or prolonged inflammatory response can lead to tissue damage and contribute to the development of autoimmune diseases.
By releasing anti-inflammatory signals, the vagus nerve helps prevent excessive immune responses that can lead to tissue damage. It acts as a “brake” on the immune system, keeping inflammation in check and promoting immune homeostasis.
Furthermore, studies have shown that stimulating the vagus nerve can suppress the production of pro-inflammatory molecules and activate immune cells responsible for reducing inflammation, such as regulatory T cells. This suggests that the vagus nerve plays a crucial role in maintaining immune balance and preventing the onset of autoimmune diseases.
How Autoimmune Diseases Affect the Vagus Nerve
In some autoimmune diseases, the immune system may mistakenly target the vagus nerve itself, leading to dysfunction and impaired communication between the nerve and immune cells. This can disrupt the regulation of inflammation and immune responses, potentially exacerbating the autoimmune process.
For example, in Guillain-Barré syndrome, an autoimmune disorder characterized by the immune system attacking the peripheral nerves, the vagus nerve can be affected, resulting in symptoms such as weakness, numbness, and paralysis.
Additionally, the chronic inflammation associated with autoimmune diseases can impact the function of the vagus nerve and compromise its ability to modulate the immune response effectively. This creates a vicious cycle where the dysregulated immune response further damages the vagus nerve, leading to a worsening of autoimmune symptoms.
Understanding the intricate relationship between the vagus nerve and autoimmune diseases is crucial for developing targeted therapies that can modulate the neuroimmune axis and restore immune balance. Researchers are exploring various approaches, including vagus nerve stimulation and pharmacological interventions, to harness the therapeutic potential of this connection.
Overall, the vagus nerve’s involvement in the immune response highlights its significance in autoimmune diseases. Further research in this field holds promise for the development of innovative treatments that can improve the lives of individuals living with these complex and often debilitating conditions.
Scientific Research on the Vagus Nerve and Autoimmune Diseases
Researchers around the world are actively investigating the relationship between the vagus nerve and autoimmune diseases. Autoimmune diseases occur when the immune system mistakenly attacks healthy cells in the body, leading to chronic inflammation and tissue damage. Understanding the role of the vagus nerve in these diseases could potentially revolutionize treatment options and improve the lives of millions of people.
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It originates in the brainstem and extends down to various organs in the body, including the heart, lungs, and digestive system. The vagus nerve plays a crucial role in regulating many bodily functions, such as heart rate, digestion, and inflammation.
Recent Findings and Developments
One recent study found that electrical stimulation of the vagus nerve can reduce inflammation and improve symptoms in animal models of rheumatoid arthritis and other autoimmune diseases. This exciting discovery suggests that vagus nerve stimulation could be a promising therapeutic approach for managing autoimmune diseases in the future. By modulating the activity of the vagus nerve, it may be possible to dampen the immune response and prevent the destructive inflammation that characterizes these diseases.
Another area of research focuses on the gut-brain axis, which highlights the connection between the gut microbiome, the vagus nerve, and autoimmune diseases. The gut microbiome refers to the trillions of bacteria and other microorganisms that reside in the gastrointestinal tract. Studies suggest that an imbalance in the gut microbiome may contribute to the development and progression of autoimmune diseases by impacting the communication between the vagus nerve and immune cells. This intricate relationship between the gut microbiome and the vagus nerve opens up new possibilities for targeted interventions.
Moreover, researchers have also found evidence suggesting that the vagus nerve may play a role in regulating the production of cytokines, which are small proteins involved in the immune response. Dysregulation of cytokines is a hallmark of autoimmune diseases, and understanding how the vagus nerve influences their production could lead to novel treatment strategies.
The Future of Vagus Nerve and Autoimmune Disease Research
As our understanding of the vagus nerve and autoimmune diseases continues to evolve, researchers are exploring new avenues for targeted therapies. These may include developing selective drugs that can modulate the activity of the vagus nerve, optimizing vagus nerve stimulation techniques, and investigating the potential role of the gut microbiome in autoimmune diseases.
Furthermore, advancements in technology have allowed for the development of non-invasive methods to stimulate the vagus nerve, such as transcutaneous vagus nerve stimulation. This technique involves applying electrical impulses to specific areas of the skin, activating the vagus nerve without the need for invasive procedures. Non-invasive vagus nerve stimulation holds great promise for the future, as it could provide a safer and more accessible alternative to traditional methods.
However, it is important to note that while research is promising, much more work needs to be done before these approaches become mainstream treatments. Clinical trials involving human participants are necessary to validate the findings from animal studies and determine the safety and efficacy of vagus nerve interventions. As always, consulting with a healthcare provider is crucial for personalized medical advice and treatment plans.
Potential Therapies and Treatments
Various therapies and treatments are being explored in the context of the vagus nerve and autoimmune diseases. However, it is essential to stress that individual treatment plans should be developed in consultation with healthcare providers, taking into account each person’s unique medical history and needs.
Vagus Nerve Stimulation Therapy
Vagus nerve stimulation therapy involves the implantation of a device that delivers electrical impulses to the vagus nerve, stimulating its activity. This therapy has been approved for certain conditions, such as epilepsy and treatment-resistant depression.
Research has shown that the vagus nerve plays a crucial role in regulating inflammation and immune responses in the body. By stimulating the vagus nerve, it is believed that the activity of the immune system can be modulated, potentially offering a new approach to managing autoimmune diseases.
Animal studies have demonstrated promising results, showing a reduction in disease severity and inflammation in models of autoimmune diseases such as rheumatoid arthritis and multiple sclerosis. However, more research is needed to determine the safety and efficacy of vagus nerve stimulation therapy for managing autoimmune diseases in humans.
Other Emerging Treatments for Autoimmune Diseases
In addition to vagus nerve stimulation therapy, other emerging treatments for autoimmune diseases are also being investigated. These include biologic medications that target specific components of the immune system, immunomodulatory drugs, and regenerative medicine approaches.
Biologic medications, such as monoclonal antibodies, work by blocking specific molecules or cells involved in the immune response. By targeting these specific components, these medications can help reduce inflammation and prevent damage to tissues and organs affected by autoimmune diseases.
Immunomodulatory drugs, on the other hand, aim to regulate the activity of the immune system as a whole. These drugs can either suppress an overactive immune response or boost a weakened immune system, depending on the specific needs of the patient.
Regenerative medicine approaches, including stem cell therapy, hold great promise for the treatment of autoimmune diseases. By using stem cells to regenerate damaged tissues or modulate the immune system, these therapies offer a potential long-term solution for managing these chronic conditions.
It is important to note that these treatments are not appropriate for all individuals and should be discussed with a healthcare provider to determine the most suitable option for each patient. Factors such as the type and severity of the autoimmune disease, the patient’s overall health, and potential side effects need to be carefully considered when developing a treatment plan.
The Impact on Patients and Healthcare
Living with an autoimmune disease can present numerous challenges, both physical and emotional, for individuals and their families. It is essential to understand the impact that these conditions can have on daily life and the role of healthcare providers in managing them.
Autoimmune diseases are a group of disorders in which the immune system mistakenly attacks healthy cells in the body. This can lead to a wide range of symptoms and complications, depending on the specific disease. For some individuals, the impact may be relatively mild, with occasional flare-ups and manageable symptoms. However, for others, the effects can be debilitating, severely impacting their ability to carry out daily activities and maintain a good quality of life.
Living with an autoimmune disease means constantly navigating a complex web of symptoms and treatments. Fatigue is a common symptom experienced by many patients, often making it difficult to engage in regular activities and maintain a consistent level of energy throughout the day. Pain and joint stiffness can also be significant challenges, limiting mobility and causing discomfort. Cognitive difficulties, such as brain fog and memory problems, can further complicate daily life, affecting concentration, decision-making, and overall cognitive function.
Emotional distress is another aspect of living with an autoimmune disease that should not be overlooked. The constant uncertainty, unpredictability, and potential for long-term complications can take a toll on a person’s mental well-being. Anxiety, depression, and feelings of isolation are not uncommon among individuals with autoimmune diseases, highlighting the need for comprehensive support and care.
Living with an Autoimmune Disease
Autoimmune diseases can significantly affect an individual’s quality of life. Symptoms may vary in severity and can include fatigue, pain, joint stiffness, cognitive difficulties, and emotional distress. Adapting to these challenges and managing symptoms require a multidisciplinary approach involving healthcare providers, self-care strategies, and support from loved ones.
Self-care strategies are essential for individuals living with autoimmune diseases. This may include making dietary changes, engaging in regular exercise, practicing stress management techniques, and getting enough rest. These self-care practices can help reduce symptoms, improve overall well-being, and enhance the effectiveness of medical treatments.
Support from loved ones is also crucial in managing the impact of autoimmune diseases. Understanding, empathy, and practical assistance can make a significant difference in a person’s ability to cope with the challenges they face. Family members and friends can provide emotional support, help with daily tasks, accompany individuals to medical appointments, and advocate for their needs within the healthcare system.
The Role of Healthcare Providers in Managing Autoimmune Diseases
Healthcare providers, including primary care physicians, specialists, and allied healthcare professionals, play a crucial role in managing autoimmune diseases. They provide accurate diagnoses, develop personalized treatment plans, and monitor the progression of the disease.
Diagnosing an autoimmune disease can be complex, as symptoms can overlap with other conditions. Healthcare providers use a combination of medical history, physical examinations, laboratory tests, and imaging studies to reach an accurate diagnosis. This is essential for determining the most appropriate treatment approach and managing the disease effectively.
Once a diagnosis is made, healthcare providers work closely with patients to develop personalized treatment plans. This may involve a combination of medications, physical therapy, occupational therapy, and other interventions aimed at reducing symptoms, preventing complications, and improving overall well-being. Regular follow-up appointments allow healthcare providers to assess the effectiveness of treatment and make any necessary adjustments.
Furthermore, healthcare providers offer support and education on managing symptoms, making lifestyle modifications, and navigating the complex healthcare system. They can provide information on available resources, support groups, and community services that can enhance a patient’s ability to cope with their condition. Patients are encouraged to maintain open and honest communication with their healthcare team to receive the best possible care.
In conclusion, living with an autoimmune disease can have a significant impact on patients and their families. The challenges faced by individuals with these conditions are diverse and can affect various aspects of daily life. Healthcare providers play a crucial role in managing autoimmune diseases, providing accurate diagnoses, developing personalized treatment plans, and offering support and education. With a comprehensive approach that includes self-care strategies, support from loved ones, and the expertise of healthcare providers, individuals with autoimmune diseases can better navigate the complexities of their condition and improve their overall well-being.
Conclusion
Understanding the link between the vagus nerve and autoimmune diseases provides valuable insights into the complex nature of these conditions. While research is ongoing, it is important to consult with healthcare providers for individualized medical advice and treatment plans. The intricacies of the vagus nerve and its impact on autoimmune diseases offer hope for future therapeutic interventions, but more research is needed to validate their effectiveness and safety.
By fostering collaboration between patients, healthcare providers, and researchers, we can advance our understanding of autoimmune diseases and develop more effective strategies for their prevention, diagnosis, and management.
If you’re captivated by the vital role the vagus nerve plays in your health and are eager to delve deeper into its functions and the ways you can nurture it, “My Vagus Nerve & Me Book” is the perfect resource for you. Embark on a journey to understand this remarkable system that orchestrates so many aspects of your well-being, from immune regulation to heart rate and beyond. Discover the secrets of stimulating your vagus nerve, both naturally and artificially, and unlock the potential to enhance your overall health. Ready to explore the wonders of the vagus nerve and its impact on your life? Get My Vagus Nerve & Me eBook today and take the first step towards harnessing the power of your body’s most fascinating nerve.