The vagus nerve is a crucial component of our nervous system, playing a significant role in various bodily functions. When this vital nerve is severed, it can have far-reaching implications for our health and well-being. In this article, we will explore the anatomy and function of the vagus nerve, delve into the causes and symptoms of vagus nerve damage, examine the diagnostic and testing methods available, and discuss the treatment options and strategies for living with a severed vagus nerve.
Anatomy of the Vagus Nerve
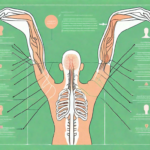
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex nerve in the body. It originates from the medulla oblongata in the brainstem and runs through the neck, chest, and abdomen. Composed of both sensory and motor fibers, the vagus nerve serves as a communication pathway between the brain and various organs, including the heart, lungs, stomach, and intestines. Its intricate network of branches allows for the transmission of vital information, regulating a wide range of bodily functions.
The vagus nerve, with its extensive reach throughout the body, is truly a remarkable structure. Let’s delve deeper into the fascinating role it plays in maintaining our overall health and well-being.
The Role of the Vagus Nerve in the Body
The vagus nerve plays a pivotal role in controlling key bodily functions, such as heart rate, blood pressure, digestion, and breathing. It is responsible for the parasympathetic nervous system, often referred to as the “rest and digest” response, which helps maintain internal homeostasis.
When we are in a state of relaxation, the vagus nerve is hard at work, ensuring that our heart beats at a steady pace, our blood pressure remains within a healthy range, and our digestive system functions optimally. It promotes the release of digestive enzymes, allowing us to break down food efficiently and absorb essential nutrients.
Furthermore, the vagus nerve influences our breathing patterns, ensuring that we inhale and exhale in a rhythmic manner. This helps oxygenate our cells and remove waste products, contributing to our overall well-being.
But the vagus nerve’s influence extends beyond these vital functions. It also plays a role in regulating inflammation and immune responses. When our body encounters an infection or injury, the vagus nerve helps modulate the immune system’s response, preventing excessive inflammation and promoting healing.
Moreover, the vagus nerve has been linked to emotional well-being. It is involved in the regulation of mood and has been associated with reducing anxiety and depression. This connection between the vagus nerve and our emotional state highlights its significance in maintaining not just our physical health, but also our mental well-being.
The Pathway of the Vagus Nerve
The vagus nerve extends from the base of the brain, passing through the neck, thorax, and into the abdomen, where it branches out. Its extensive network of fibers innervates various organs, including the heart, lungs, esophagus, stomach, liver, pancreas, and intestines.
As the vagus nerve travels through the body, it forms intricate connections with these organs, allowing for precise control and regulation. For example, it sends signals to the heart, instructing it to beat at the appropriate rate to meet the body’s demands. It also influences the muscles in the digestive tract, coordinating their contractions to facilitate the movement of food through the system.
Furthermore, the vagus nerve is involved in the release of digestive enzymes and the stimulation of gastric acid production, ensuring efficient digestion and absorption of nutrients. It also communicates with the liver, playing a role in regulating glucose metabolism and maintaining stable blood sugar levels.
The vagus nerve’s pathway encompasses both afferent fibers (carrying sensory information from the organs to the brain) and efferent fibers (sending signals from the brain to the organs). This bidirectional communication enables the regulation of numerous bodily functions.
In conclusion, the vagus nerve is a remarkable structure that connects the brain to various organs, allowing for the precise regulation of vital bodily functions. Its role in maintaining homeostasis, controlling inflammation, and influencing emotional well-being highlights its significance in overall health. Understanding the anatomy and function of the vagus nerve provides us with a deeper appreciation for the intricate mechanisms that govern our bodies.
Causes of Vagus Nerve Damage
Vagus nerve damage can occur due to various reasons, including accidental injury and surgical complications. Understanding these causes is vital in appreciating the potential risks and taking necessary precautions.
Accidental Injury and the Vagus Nerve
Vagus nerve damage resulting from accidental trauma is a serious concern. The vagus nerve, also known as the tenth cranial nerve, is a crucial component of the autonomic nervous system. It plays a significant role in regulating various bodily functions, including heart rate, digestion, and breathing.
Accidental trauma, such as a severe blow to the neck or chest, can lead to vagus nerve damage. This can happen in situations like motor vehicle accidents, sports-related injuries, or even physical altercations. The forceful impact can cause compression or stretching of the nerve, disrupting its normal functioning.
Recognizing the signs and symptoms of vagus nerve damage is essential for prompt diagnosis and appropriate management. Common symptoms may include hoarseness or loss of voice, difficulty swallowing, changes in heart rate or blood pressure, and gastrointestinal issues. It is essential to be cautious and seek medical attention immediately following such incidents to promptly diagnose and manage any potential vagus nerve damage.
Surgical Complications Leading to Vagus Nerve Damage
While accidental injuries are a significant cause of vagus nerve damage, surgical complications can also pose a risk. Certain surgical procedures, particularly those involving the neck, chest, or abdomen, carry a potential for vagus nerve injury. Although the incidence is relatively rare, it is crucial for patients and healthcare providers to be aware of this possibility.
During surgical interventions, the vagus nerve may be at risk of damage due to its proximity to the surgical site. Procedures such as thyroidectomy, heart surgery, or gastrointestinal surgeries can inadvertently affect the vagus nerve. Surgeons take precautions to minimize the risk, but it is important for patients to understand the potential complications.
Patients undergoing surgical interventions should discuss the potential risks with their healthcare provider in advance to make informed decisions. By understanding the potential for vagus nerve damage, patients can weigh the benefits and risks of the procedure and take necessary precautions. Surgeons, on the other hand, must exercise caution and employ meticulous surgical techniques to minimize the risk of vagus nerve injury.
In conclusion, vagus nerve damage can occur due to accidental injury or surgical complications. Accidental trauma, such as severe blows to the neck or chest, can compress or stretch the nerve, disrupting its normal functioning. Surgical procedures involving the neck, chest, or abdomen also carry a potential risk of vagus nerve damage. It is crucial for individuals to be aware of these causes and take necessary precautions to protect the vagus nerve and maintain overall well-being.
Symptoms of a Severed Vagus Nerve
The symptoms of a severed vagus nerve can vary depending on the location and severity of the damage. It is important to recognize these symptoms as they may indicate the need for medical attention.
A severed vagus nerve can have a profound impact on a person’s physical and psychological well-being. The nerve, which is responsible for regulating various bodily functions, plays a crucial role in maintaining overall health. When the vagus nerve is severed, it can result in a range of symptoms that can significantly affect a person’s quality of life.
Physical Manifestations of Vagus Nerve Damage
Damage to the vagus nerve can result in a range of physical symptoms, including difficulty swallowing, hoarseness or voice changes, heart rhythm abnormalities, gastrointestinal disturbances (such as nausea, vomiting, or bloating), and breathing difficulties.
Difficulty swallowing, known as dysphagia, can make it challenging to eat and drink. This can lead to weight loss, malnutrition, and dehydration if not properly managed. Hoarseness or voice changes can affect a person’s ability to communicate effectively, impacting their personal and professional relationships.
Heart rhythm abnormalities, also known as arrhythmias, can be life-threatening if left untreated. These irregular heartbeats can cause dizziness, fainting, and chest pain. Gastrointestinal disturbances, such as nausea, vomiting, or bloating, can significantly impact a person’s digestive system, leading to discomfort and disruption of daily activities.
In addition, breathing difficulties can make it challenging to get enough oxygen into the body, resulting in fatigue, shortness of breath, and decreased physical endurance. These physical symptoms can be distressing and may require medical intervention to manage effectively.
If you experience any of these physical symptoms, it is crucial to consult a healthcare professional to rule out vagus nerve damage or seek appropriate management strategies.
Psychological Impact of a Severed Vagus Nerve
In addition to physical symptoms, vagus nerve damage can also have psychological effects. The vagus nerve plays a crucial role in regulating mood and emotions, and when severed, it can disrupt these processes.
Individuals with a severed vagus nerve may experience mood changes, such as irritability, sadness, or sudden shifts in emotions. These mood swings can be challenging to manage and may impact a person’s relationships and overall well-being.
Anxiety and depression are also common psychological symptoms associated with vagus nerve damage. The nerve’s role in regulating the body’s stress response system can be compromised, leading to heightened anxiety and a persistent feeling of sadness or hopelessness.
In addition to mood changes and psychological distress, individuals with a severed vagus nerve may also experience difficulties with memory and concentration. These cognitive impairments can affect a person’s ability to focus, remember important information, and perform daily tasks effectively.
It is essential to seek emotional support and consult with a mental health professional to address these challenges and develop coping mechanisms. Therapy, medication, and lifestyle changes can all play a role in managing the psychological impact of a severed vagus nerve.
In conclusion, a severed vagus nerve can have a significant impact on a person’s physical and psychological well-being. Recognizing the symptoms and seeking appropriate medical and emotional support is crucial in managing the effects of vagus nerve damage.
Diagnosis and Testing for Vagus Nerve Damage
Accurate diagnosis and testing are fundamental in assessing the extent of vagus nerve damage and developing an appropriate treatment plan. Healthcare professionals employ various techniques to evaluate the condition.
When it comes to diagnosing vagus nerve damage, a thorough medical history and physical examination are crucial steps. Physicians will take the time to inquire about the patient’s symptoms, medical conditions, and any potential exposure to trauma or surgical procedures. This information is essential in understanding the context of the nerve damage and its possible causes.
Furthermore, during the physical examination, healthcare professionals will perform a comprehensive assessment, focusing on areas innervated by the vagus nerve. By carefully examining these areas, they can identify any physical signs that may indicate nerve damage. This may include testing the patient’s ability to swallow, assessing their vocal cord function, and evaluating their gag reflex.
Advanced Diagnostic Techniques
In addition to the medical history and physical examination, advanced diagnostic techniques are often employed to further evaluate the integrity and functionality of the vagus nerve. These tests provide objective data and valuable insights into the extent of nerve damage, guiding treatment decisions and strategies for management.
One such technique is imaging studies, which can include magnetic resonance imaging (MRI) or computed tomography (CT) scans. These imaging techniques allow healthcare professionals to visualize the vagus nerve and surrounding structures, helping to identify any abnormalities or damage.
Nerve conduction tests are another valuable tool in diagnosing vagus nerve damage. This test involves the placement of electrodes on the skin to measure the electrical impulses transmitted along the nerve. By assessing the speed and strength of these impulses, healthcare professionals can determine if there is any disruption or damage to the vagus nerve.
Electrical stimulation is yet another technique used to evaluate the functionality of the vagus nerve. During this test, a small electrical current is applied to the nerve, and the response is measured. This can help determine if the nerve is able to transmit signals effectively, or if there is any impairment.
Overall, the combination of a thorough medical history, physical examination, and advanced diagnostic techniques allows healthcare professionals to accurately diagnose and assess the extent of vagus nerve damage. This comprehensive approach ensures that an appropriate treatment plan can be developed to address the specific needs of each patient.
Treatment Options for a Severed Vagus Nerve
The treatment of a severed vagus nerve depends on the severity of the damage and its impact on bodily functions. It is essential to collaborate with healthcare professionals to determine the best course of action.
A severed vagus nerve can have significant implications for an individual’s overall health and well-being. The vagus nerve plays a crucial role in regulating various bodily functions, including digestion, heart rate, and even mood. When the nerve is severed, it can lead to a range of symptoms, such as difficulty swallowing, voice changes, gastrointestinal issues, and even emotional disturbances.
Surgical Interventions for Vagus Nerve Repair
In severe cases of vagus nerve damage, surgical interventions may be necessary to repair or reconstruct the damaged nerve. Surgeons employ various techniques, such as nerve grafts or nerve transfers, to restore nerve function and alleviate symptoms. These surgical procedures require a high level of expertise and precision to ensure successful outcomes.
During a nerve graft procedure, a healthy nerve from another part of the body is harvested and used to bridge the gap created by the severed vagus nerve. This allows for the regrowth of nerve fibers and the restoration of normal function. Nerve transfers, on the other hand, involve taking a nearby functioning nerve and rerouting it to the damaged area, providing a new pathway for nerve signals.
However, it is important to note that surgical treatments are not appropriate or feasible for every patient. Factors such as the location and extent of the nerve damage, as well as the overall health of the individual, need to be carefully considered before opting for surgery. The decision should always be made in consultation with a healthcare professional who can assess the risks and benefits and provide personalized recommendations.
Non-Surgical Management Strategies
For individuals with less severe vagus nerve damage, non-surgical management strategies can be employed to alleviate symptoms and improve quality of life. These strategies focus on maximizing the remaining nerve function and compensating for any deficits.
Lifestyle modifications play a crucial role in managing vagus nerve damage. Dietary changes, such as consuming foods that are easy to swallow and digest, can help prevent complications like aspiration pneumonia and malnutrition. Stress management techniques, such as deep breathing exercises, meditation, and yoga, can also be beneficial in reducing the impact of stress on the body and promoting overall well-being.
Physical therapy is another non-surgical approach that can be used to address specific symptoms associated with vagus nerve damage. Therapists can design customized exercise programs to improve swallowing function, enhance vocal quality, and strengthen the muscles affected by the nerve injury.
In some cases, medications may be prescribed to manage specific symptoms caused by the severed vagus nerve. For example, medications that promote gastric motility can help alleviate digestive issues, while medications targeting anxiety or depression can address emotional disturbances. It is important to work closely with a healthcare professional to determine the most appropriate medications and dosages for individual needs.
Consulting with a healthcare professional who specializes in nerve injuries can help tailor these non-surgical strategies to individual needs and circumstances. They can provide guidance and support throughout the treatment process, ensuring the best possible outcomes for patients with a severed vagus nerve.
Living with a Severed Vagus Nerve
Living with a severed vagus nerve can be a life-altering experience. The vagus nerve, also known as the “wandering nerve,” plays a crucial role in regulating various bodily functions, including digestion, heart rate, and breathing. When this nerve is severed, it can have profound impacts on daily life, affecting not only physical health but also emotional well-being.
While the challenges of living with a severed vagus nerve may seem overwhelming, there are strategies and resources available to help individuals adapt and cope with the changes they may face. Making lifestyle adjustments can be beneficial in managing the symptoms associated with vagus nerve damage. Adopting a healthy diet, rich in nutrients and fiber, can support digestive health and alleviate gastrointestinal issues that may arise. Engaging in regular exercise, such as walking or yoga, can help improve overall well-being and promote a sense of balance.
Practicing stress reduction techniques, such as deep breathing exercises or meditation, can be particularly helpful in managing the emotional toll of living with a severed vagus nerve. Chronic pain, anxiety, and depression are common challenges faced by individuals with vagus nerve damage. Prioritizing self-care, whether through engaging in hobbies, spending time in nature, or seeking professional therapy, can provide much-needed relief and support.
Support Systems and Resources for Patients
Living with a severed vagus nerve can be challenging, both physically and emotionally. It is essential to build a strong support system to navigate these difficulties. Healthcare professionals, including neurologists, gastroenterologists, and therapists, can provide valuable guidance and expertise in managing the symptoms and addressing any underlying conditions.
Additionally, patient advocacy organizations and online communities can offer a sense of understanding and connection. These platforms provide a space for individuals with vagus nerve damage to share their experiences, exchange information, and find support. Connecting with others who have similar journeys can be empowering and reassuring, reminding individuals that they are not alone in their struggles.
It is important to remember that each person’s experience with a severed vagus nerve is unique. While it is valuable to learn from others and gain support, it is equally important to respect individual differences and tailor approaches to personal circumstances. What works for one person may not work for another, and finding the right combination of strategies and resources may require time and experimentation.
In conclusion, understanding the implications of a severed vagus nerve is essential in comprehending the potential effects on bodily functions and overall well-being. By familiarizing ourselves with the anatomy, causes, symptoms, diagnosis, and treatment options associated with vagus nerve damage, we can better navigate this complex condition. It is crucial to consult with healthcare professionals, who can provide expert advice and guidance tailored to individual circumstances.
If you’re fascinated by the remarkable capabilities of the vagus nerve and its profound impact on your health, “My Vagus Nerve & Me Book” is an invaluable resource waiting to be explored. Delve into the complexities of this extraordinary system, from understanding its functions to learning how to stimulate it for optimal well-being. Discover the secrets of liver detoxification, bile production, blood sugar regulation, and much more. Take the first step towards harnessing the power of your vagus nerve for a healthier, more balanced life. Get My Vagus Nerve & Me eBook today and embark on a journey of self-discovery and improved health.