The vagus nerve, also known as the tenth cranial nerve, is a crucial component of the human nervous system. The purpose of this article is to shed light on the effects of a pinched vagus nerve, including its anatomy, causes, symptoms, diagnostic procedures, treatment options, and prevention. However, it is important to note that all information presented here is for informational purposes only and should not be considered medical advice. If you suspect you have a pinched vagus nerve or any related conditions, please consult with a healthcare professional for proper diagnosis and guidance.
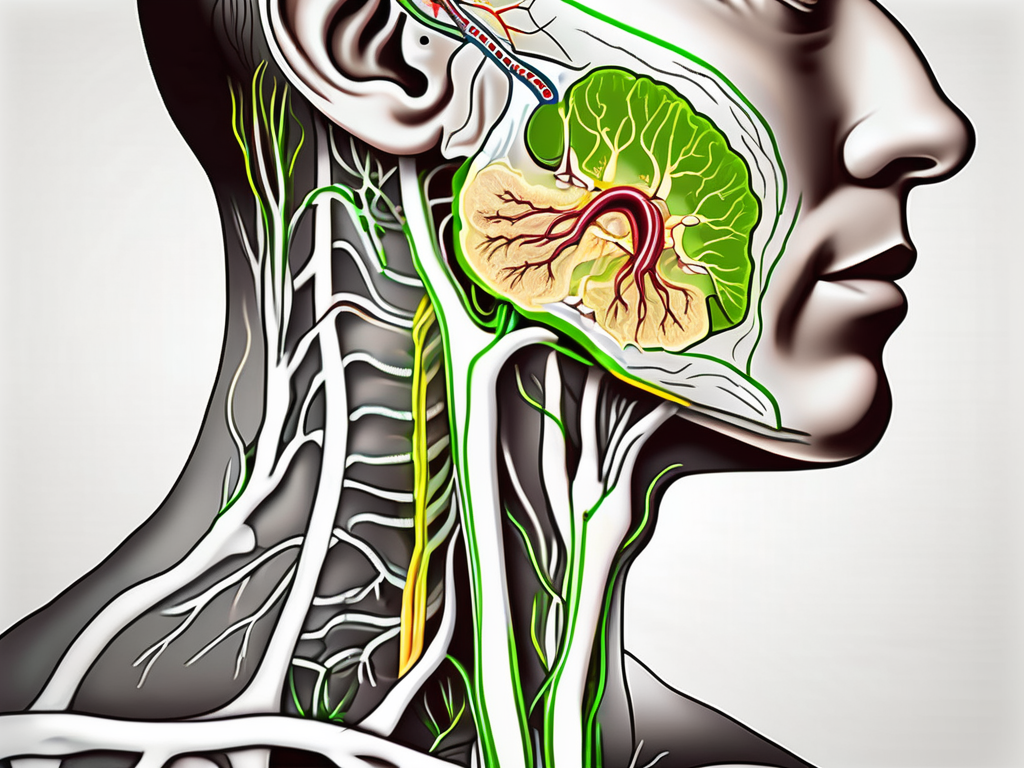
Anatomy of the Vagus Nerve
The vagus nerve, also known as the cranial nerve X, is an incredibly fascinating and important part of the human body. It holds the title for being the longest cranial nerve, stretching all the way from the brainstem to the abdomen. This complex network of nerve fibers connects the brain to various organs, including the heart, lungs, digestive system, and even the vocal cords.
When it comes to regulating essential bodily functions, the vagus nerve takes center stage. It plays a vital role in controlling heart rate, digestion, breathing, and even speech. Without the vagus nerve, these functions would be compromised, leading to significant health issues.
Role and Function of the Vagus Nerve
The vagus nerve is a true superhero when it comes to maintaining homeostasis and overall well-being. It acts as a communication highway, carrying sensory and motor information between the brain and different organs. This means that it not only relays important signals from the brain to the organs but also sends feedback from the organs back to the brain.
One of the most intriguing aspects of the vagus nerve is its influence on the autonomic nervous system. This system controls involuntary bodily functions, such as heart rate, blood pressure, and digestion. The vagus nerve, particularly its parasympathetic branch, plays a significant role in promoting rest, relaxation, and digestion. It counterbalances the sympathetic branch, which is responsible for the fight-or-flight response.
Through its intricate network of fibers, the vagus nerve helps regulate heart rate, ensuring that it beats at a steady pace. It also influences the muscles involved in breathing, allowing us to take in oxygen and expel carbon dioxide effortlessly. Additionally, the vagus nerve stimulates the digestive system, promoting the secretion of digestive juices and facilitating the movement of food through the intestines.
Location and Pathway of the Vagus Nerve
The vagus nerve originates from the brainstem, specifically the medulla oblongata. This region, located at the base of the brain, serves as the nerve’s command center. From there, the vagus nerve embarks on its incredible journey, traveling down through the neck and chest.
As it makes its way through the neck, the vagus nerve passes alongside vital structures such as the carotid artery and jugular vein. This close proximity to major blood vessels highlights the nerve’s importance in regulating heart rate and blood pressure.
Continuing its descent, the vagus nerve branches out to innervate various organs throughout the body. It forms connections with the heart, lungs, liver, intestines, and many other organs, ensuring that they receive the necessary signals for proper functioning.
The vagus nerve truly is a remarkable part of our anatomy. Its extensive reach and crucial role in maintaining bodily functions make it an essential component of our overall health and well-being.
Causes of a Pinched Vagus Nerve
A pinched vagus nerve, also known as vagus nerve compression or impingement, can occur due to several factors. Understanding the underlying causes is crucial in managing and preventing this condition.
The vagus nerve, also called the tenth cranial nerve, is one of the longest and most important nerves in the body. It plays a vital role in regulating various bodily functions, including heart rate, digestion, and breathing. When this nerve is compressed or irritated, it can lead to a range of symptoms and complications.
Physical Trauma and Injuries
One potential cause of a pinched vagus nerve is physical trauma or injuries to the neck, chest, or upper back. Examples include whiplash from car accidents, sports injuries, or falls. These traumatic events can cause sudden jolts or jerks to the body, leading to compression or irritation of the nerve.
Imagine a scenario where a person is involved in a car accident. The impact of the collision causes their head to snap forward and backward rapidly, resulting in whiplash. This sudden movement can put pressure on the vagus nerve, disrupting its normal function.
Medical Conditions Leading to Nerve Compression
Various medical conditions can contribute to the compression of the vagus nerve. These conditions include cervical spine disorders, such as herniated discs or bone spurs, tumors, infections, and inflammation. When these conditions affect the structures surrounding the vagus nerve, they can exert pressure on the nerve, leading to impingement.
Let’s consider an example of a person diagnosed with a herniated disc in their cervical spine. The herniated disc protrudes and presses against the vagus nerve, causing compression. This compression can disrupt the normal flow of nerve signals, resulting in symptoms such as difficulty swallowing, hoarseness, or changes in heart rate.
In addition to cervical spine disorders, certain autoimmune disorders or other systemic diseases may cause nerve impingement. Conditions like rheumatoid arthritis, lupus, or diabetes can lead to inflammation in the body, which can affect the vagus nerve and result in compression.
It is important to note that while these are common causes of a pinched vagus nerve, there may be other factors at play as well. Each individual’s case is unique, and a thorough evaluation by a healthcare professional is necessary to determine the exact cause and develop an appropriate treatment plan.
Symptoms Associated with a Pinched Vagus Nerve
The symptoms of a pinched vagus nerve can vary depending on the severity and location of the compression. It is important to note that these symptoms can also be indicative of other underlying health issues, so proper medical evaluation is crucial.
Physical Symptoms and Manifestations
Physical symptoms associated with a pinched vagus nerve may include difficulty swallowing, voice hoarseness, slowed heart rate, altered digestion, bloating, and constipation. Additionally, some individuals may experience chest pain, difficulty breathing, or changes in blood pressure.
When the vagus nerve is compressed, it can disrupt the normal function of the muscles responsible for swallowing. This can lead to difficulty in swallowing food and liquids, causing discomfort and potential choking hazards. Voice hoarseness may also occur due to the nerve’s involvement in controlling the vocal cords.
Furthermore, the vagus nerve plays a crucial role in regulating heart rate. When compressed, it can result in a slowed heart rate, leading to feelings of fatigue and dizziness. Altered digestion, bloating, and constipation can also be attributed to the vagus nerve’s influence on the gastrointestinal system.
While not as common, some individuals with a pinched vagus nerve may experience chest pain, which can be alarming. This occurs due to the nerve’s connection to the heart and the potential disruption of its normal functioning. Difficulty breathing and changes in blood pressure can also be associated with vagus nerve compression.
Psychological and Emotional Effects
In some cases, a pinched vagus nerve can have psychological and emotional effects. These may include anxiety, depression, mood swings, and problems with memory and concentration. It is important to note that these symptoms can also manifest due to other factors, so professional assessment is essential.
The vagus nerve is intricately linked to the brain and plays a significant role in regulating mood and emotions. When compressed, it can disrupt the normal flow of signals between the brain and the body, potentially leading to psychological and emotional imbalances.
Anxiety and depression are common psychological effects of a pinched vagus nerve. The constant discomfort and physical symptoms associated with the compression can contribute to feelings of unease and sadness. Mood swings may also occur, causing individuals to experience sudden shifts in emotions without apparent triggers.
Problems with memory and concentration can be attributed to the vagus nerve’s involvement in cognitive function. When compressed, it can impair the brain’s ability to process information efficiently, leading to difficulties in remembering and focusing on tasks.
It is important to remember that while these psychological and emotional effects can be associated with a pinched vagus nerve, they can also be caused by other factors. Therefore, seeking professional assessment and diagnosis is crucial to determine the underlying cause of these symptoms.
Diagnostic Procedures for a Pinched Vagus Nerve
Diagnosing a pinched vagus nerve involves a comprehensive assessment of the patient’s medical history, physical examination, and, in some cases, additional tests.
A pinched vagus nerve can cause a variety of symptoms, including difficulty swallowing, hoarseness, heart palpitations, and gastrointestinal issues. To accurately diagnose a pinched vagus nerve, healthcare providers employ a range of diagnostic procedures.
Medical History and Physical Examination
During the medical history interview, the healthcare provider will inquire about symptoms, medical conditions, and any recent trauma or injuries. This information helps establish a baseline understanding of the patient’s overall health and identify any potential risk factors for nerve compression.
Following the medical history interview, a thorough physical examination will be performed. The healthcare provider will carefully assess the patient’s neck, chest, and upper back for signs of nerve compression. They will look for muscle weakness, tenderness, and any abnormalities in the range of motion. Additionally, they may check for any visible swelling or deformities that could indicate nerve compression.
During the physical examination, the healthcare provider may also perform specific tests to evaluate the function of the vagus nerve. These tests can include assessing the patient’s ability to swallow, monitoring heart rate and rhythm, and evaluating the patient’s voice quality.
Imaging and Laboratory Tests
In some cases, imaging tests such as X-rays, magnetic resonance imaging (MRI), or computed tomography (CT) scans may be necessary to visualize the structures surrounding the vagus nerve. These imaging tests can provide detailed images of the neck, chest, and upper back, allowing healthcare providers to identify any potential sources of nerve compression, such as herniated discs, bone spurs, or tumors.
Additionally, blood tests and other laboratory investigations may be ordered to rule out underlying medical conditions that could be contributing to the symptoms. These tests can help identify any systemic issues, such as autoimmune disorders or infections, that may be affecting the vagus nerve.
Furthermore, nerve conduction studies and electromyography (EMG) may be utilized to assess the electrical activity and function of the nerves. These tests involve the placement of small electrodes on the skin to measure the nerve signals and muscle responses, providing valuable information about the health of the vagus nerve.
Overall, the diagnostic procedures for a pinched vagus nerve aim to gather comprehensive information about the patient’s medical history, perform a thorough physical examination, and utilize imaging and laboratory tests to identify the underlying cause of the nerve compression. By employing a multidimensional approach, healthcare providers can accurately diagnose a pinched vagus nerve and develop an appropriate treatment plan to alleviate symptoms and improve the patient’s quality of life.
Treatment Options for a Pinched Vagus Nerve
The treatment of a pinched vagus nerve may involve various approaches, depending on the underlying cause, severity of symptoms, and individual patient factors. It is essential to seek professional medical advice for proper management.
A pinched vagus nerve can cause a range of symptoms, including difficulty swallowing, hoarseness, heart palpitations, and gastrointestinal issues. Non-surgical interventions are often the first line of treatment and can provide significant relief for many individuals.
Non-Surgical Interventions
Non-surgical interventions may include physical therapy, stretching exercises, and posture correction. Physical therapy can help improve muscle strength and flexibility, reducing pressure on the vagus nerve. Stretching exercises can also help alleviate tension in the neck and throat area, providing relief from symptoms.
In addition to physical therapy, pain management techniques may be employed to alleviate discomfort. Medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, or nerve pain medications, may be prescribed to reduce inflammation and relieve pain associated with the pinched vagus nerve. Nerve blocks, which involve injecting a local anesthetic or steroid medication near the affected nerve, can also provide temporary relief.
Furthermore, lifestyle modifications can play a crucial role in managing a pinched vagus nerve. Stress reduction techniques, such as meditation, deep breathing exercises, or yoga, can help relax the body and alleviate tension in the neck and throat area. Dietary changes, such as avoiding foods that may trigger inflammation or irritation in the throat, can also be beneficial.
Surgical Procedures and Their Risks
In severe cases or when conservative measures fail, surgical intervention may be considered. The specific procedure would depend on the underlying cause of the pinched vagus nerve. One surgical option is vagus nerve decompression, which involves relieving pressure on the nerve by removing surrounding structures or tissues that may be compressing it.
Another surgical approach is neurolysis, where scar tissue or adhesions around the vagus nerve are removed to restore its normal function. In some cases, a surgical release of the surrounding muscles may be necessary to alleviate pressure on the nerve.
While surgical procedures can provide relief for individuals with a pinched vagus nerve, it is important to understand the potential risks and benefits. Risks associated with surgery may include infection, bleeding, nerve damage, or adverse reactions to anesthesia. A thorough evaluation of the individual’s condition and a consultation with a specialist are necessary to determine the most appropriate surgical approach and understand the potential outcomes.
In conclusion, the treatment options for a pinched vagus nerve range from non-surgical interventions, such as physical therapy and pain management techniques, to surgical procedures like vagus nerve decompression or neurolysis. The choice of treatment depends on the severity of symptoms, underlying cause, and individual patient factors. Seeking professional medical advice is crucial to ensure proper management and relief from the symptoms associated with a pinched vagus nerve.
Prevention and Management of a Pinched Vagus Nerve
While it may not always be possible to prevent a pinched vagus nerve, there are certain measures individuals can take to minimize the risk or manage the symptoms.
A pinched vagus nerve can be a debilitating condition that affects the functioning of the body’s vital organs. It occurs when the vagus nerve, which runs from the brainstem to the abdomen, becomes compressed or irritated. This compression can lead to a variety of symptoms, including difficulty swallowing, heart palpitations, and digestive issues.
Lifestyle Modifications and Home Remedies
Engaging in regular exercise is not only beneficial for overall health but can also help reduce the likelihood of nerve compression. Exercise helps to strengthen the muscles surrounding the vagus nerve, providing support and reducing the risk of compression. Additionally, maintaining good posture is crucial in preventing a pinched vagus nerve. Poor posture can put unnecessary pressure on the nerve, leading to compression and discomfort.
Practicing stress management techniques is another important aspect of preventing and managing a pinched vagus nerve. Stress can cause muscle tension and inflammation, which can exacerbate nerve compression. Techniques such as deep breathing exercises, meditation, and yoga can help reduce stress levels and promote relaxation, ultimately alleviating the symptoms associated with a pinched vagus nerve.
Using ergonomic pillows can also provide relief for individuals with a pinched vagus nerve. These pillows are designed to support the neck and promote proper alignment, reducing the risk of compression during sleep. Additionally, avoiding prolonged periods of neck or chest compression is crucial. This can be achieved by avoiding activities that put excessive pressure on these areas, such as wearing tight clothing or carrying heavy bags on one shoulder.
However, it is important to note that these lifestyle modifications should be discussed with a healthcare professional to ensure their appropriateness for individual circumstances. A healthcare provider can provide personalized advice and guidance based on the specific needs and condition of each individual.
Regular Check-ups and Monitoring
Regular check-ups with a healthcare provider are essential for monitoring the condition and evaluating the effectiveness of treatments. These check-ups allow healthcare professionals to assess the progress of the pinched vagus nerve and make any necessary adjustments to the management plan. Open communication with the healthcare team is crucial, as it allows for the timely adjustment of treatments and ensures the best possible outcome for each individual.
During these check-ups, healthcare providers may perform various tests and examinations to assess the functioning of the vagus nerve. These tests may include nerve conduction studies, which measure the electrical activity of the nerve, and imaging tests, such as magnetic resonance imaging (MRI), to visualize any compression or damage to the nerve.
In addition to regular check-ups, individuals with a pinched vagus nerve should also be proactive in monitoring their symptoms and seeking medical attention if they worsen or change. Keeping a symptom diary can be helpful in tracking any patterns or triggers that may exacerbate the condition.
In conclusion, while it may not always be possible to prevent a pinched vagus nerve, lifestyle modifications and regular check-ups can help minimize the risk and manage the symptoms. By taking proactive steps and working closely with healthcare professionals, individuals can find relief and improve their overall quality of life.
Conclusion
In conclusion, a pinched vagus nerve can have a significant impact on an individual’s well-being. Understanding its anatomy, causes, symptoms, diagnostic procedures, treatment options, and prevention strategies is vital for comprehensive care. If you suspect you have a pinched vagus nerve or experience related symptoms, it is crucial to consult with a trusted healthcare professional for proper evaluation and guidance. Remember, this article serves as informational content and not medical advice.
If you’re fascinated by the intricate workings of the vagus nerve and its profound impact on your health, “My Vagus Nerve & Me Book” is an essential read. Dive deeper into the world of this remarkable nerve system, from its regulatory functions to natural and artificial stimulation techniques. Discover how to harness the power of your vagus nerve for improved immunity, digestion, heart rate, and mental health, among other benefits. Ready to embark on a journey of understanding and wellness? Get My Vagus Nerve & Me eBook today and take the first step towards optimizing your body’s most complex system.