The vagus nerve and hiatal hernia may seem like unrelated topics, but they are actually connected in several ways. To fully understand this connection, it is important to explore both the role and function of the vagus nerve and the comprehensive nature of a hiatal hernia. By delving into these topics, we can gain insight into how the vagus nerve influences hiatal hernia and how hiatal hernia affects the vagus nerve. This understanding can help inform diagnosis, treatment options, and prevention strategies for individuals affected by these conditions.
An Overview of the Vagus Nerve
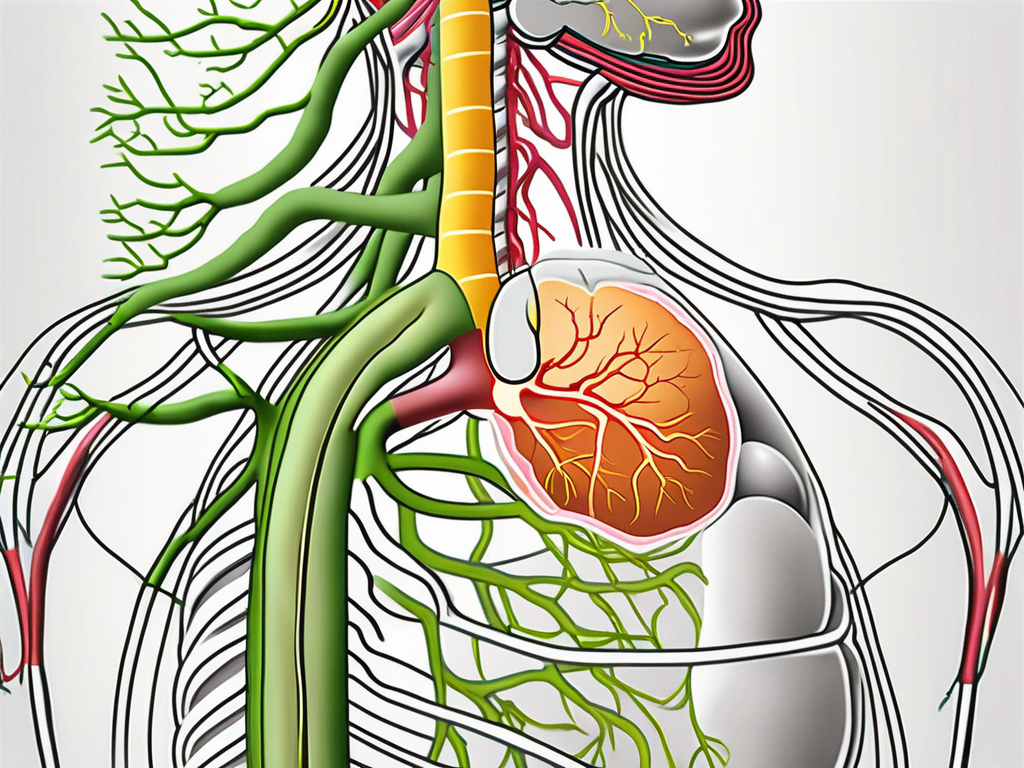
The vagus nerve, also known as the tenth cranial nerve, plays a critical role in the autonomic nervous system. It is the longest and most complex of the cranial nerves, extending from the brainstem down into the abdomen. The vagus nerve is responsible for transmitting signals between the brain and various organs, including the heart, lungs, digestive system, and other vital organs.
The vagus nerve, named after the Latin word for “wandering,” gets its name due to its extensive reach throughout the body. It is like a highway, connecting the brain to different regions and ensuring smooth communication between them. This nerve is composed of both sensory and motor fibers, allowing it to transmit information from the body to the brain and vice versa.
While the vagus nerve is often associated with its role in the autonomic nervous system, it also has connections to the somatic nervous system. This means that it can influence both involuntary processes, such as heart rate and digestion, as well as voluntary actions, like speaking and swallowing.
The Role and Function of the Vagus Nerve
The vagus nerve is involved in numerous physiological processes, such as regulating heart rate, controlling digestion, and managing inflammation. It helps maintain the balance between the sympathetic and parasympathetic nervous systems, ensuring the body operates efficiently and adapts to different situations.
One of the key functions of the vagus nerve is its role in heart rate variability. It acts as a regulator, adjusting the heart rate to match the body’s needs. When we engage in physical activity, the vagus nerve decreases heart rate to conserve energy. On the other hand, during moments of stress or excitement, the vagus nerve increases heart rate to prepare the body for action.
In addition to its impact on the cardiovascular system, the vagus nerve plays a crucial role in digestion. It stimulates the release of digestive enzymes and increases blood flow to the digestive organs, promoting efficient nutrient absorption and waste elimination. This nerve also helps regulate gastrointestinal motility, ensuring the smooth movement of food through the digestive tract.
Furthermore, the vagus nerve is known for its anti-inflammatory properties. It helps control the body’s immune response by reducing the production of pro-inflammatory molecules. This modulation of inflammation is crucial for maintaining overall health and preventing chronic inflammatory conditions.
Another fascinating function of the vagus nerve is its involvement in the body’s stress response. When activated, it promotes relaxation and reduces anxiety. This is why techniques like deep breathing and meditation, which stimulate the vagus nerve, are effective in reducing stress levels.
The Vagus Nerve’s Impact on Body Systems
Due to its extensive reach, the vagus nerve has a profound impact on various body systems. For example, it influences heart rate variability, breathing patterns, and gastrointestinal motility. It also communicates with the brain’s reward and pleasure centers, which can affect mood, emotional well-being, and even cravings for certain foods.
When the vagus nerve is functioning optimally, it helps regulate heart rate variability, ensuring a healthy balance between sympathetic and parasympathetic activity. This balance is essential for maintaining cardiovascular health and preventing conditions such as arrhythmias and hypertension.
In terms of breathing, the vagus nerve plays a crucial role in controlling respiratory rate and depth. It helps coordinate the smooth rhythm of inhalation and exhalation, allowing for efficient gas exchange in the lungs. Dysfunction of the vagus nerve can lead to irregular breathing patterns, such as rapid or shallow breathing.
Moreover, the vagus nerve’s connection to the brain’s reward and pleasure centers can influence our mood and emotional well-being. Activation of the vagus nerve triggers the release of neurotransmitters like serotonin and dopamine, which are associated with feelings of happiness and contentment. This is why activities that stimulate the vagus nerve, such as socializing, laughter, and engaging in hobbies, can have a positive impact on our mental health.
Additionally, the vagus nerve interacts with the immune system, assisting in the regulation of inflammation and immune responses. It helps maintain a delicate balance between pro-inflammatory and anti-inflammatory processes, preventing excessive immune activation or suppression. Dysfunction of the vagus nerve can contribute to chronic inflammation, which is implicated in various diseases, including autoimmune disorders and metabolic conditions.
In conclusion, the vagus nerve is a remarkable component of the nervous system, with far-reaching effects on the body. Its role in regulating heart rate, digestion, inflammation, and stress response highlights its importance in maintaining overall health and well-being. Understanding the intricacies of the vagus nerve can provide valuable insights into various physiological processes and open doors for potential therapeutic interventions.
Comprehensive Understanding of Hiatal Hernia
A hiatal hernia occurs when a part of the stomach protrudes through the diaphragm into the chest cavity. This condition occurs when the opening known as the hiatus, which allows the esophagus to pass through the diaphragm, becomes enlarged or weakened. Hiatal hernias can either be sliding or paraesophageal, with sliding hernias being the most common. While some individuals with a hiatal hernia might not experience any symptoms, others may experience discomfort, heartburn, regurgitation, and other complications.
What is a Hiatal Hernia?
A hiatal hernia is a condition characterized by the displacement of the stomach into the chest cavity through the diaphragm. Sliding hiatal hernias are more prevalent and occur when the gastroesophageal junction moves up into the chest when swallowing. Paraesophageal hiatal hernias, on the other hand, are less common but pose a higher risk of complications as they involve the stomach moving up into the chest alongside the esophagus.
When a hiatal hernia occurs, it can disrupt the normal anatomy and function of the digestive system. The diaphragm, a dome-shaped muscle that separates the chest cavity from the abdominal cavity, plays a crucial role in breathing. It also has an opening called the hiatus, which allows the esophagus to pass through and connect to the stomach. However, when the hiatus becomes enlarged or weakened, it can lead to the development of a hiatal hernia.
Sliding hiatal hernias, as the name suggests, involve the stomach and the gastroesophageal junction sliding up into the chest. This movement occurs during swallowing when the muscles in the esophagus contract to push food down into the stomach. In some cases, the stomach may slide back down into the abdominal cavity after swallowing, but in others, it remains in the chest cavity.
Paraesophageal hiatal hernias, on the other hand, are characterized by the stomach moving up into the chest alongside the esophagus. Unlike sliding hernias, the gastroesophageal junction remains in its normal position. This type of hiatal hernia is less common but can be more concerning as it carries a higher risk of complications.
Common Symptoms and Complications of Hiatal Hernia
Individuals with a hiatal hernia may experience a range of symptoms, including heartburn, chest pain, difficulty swallowing, regurgitation of stomach acid, and feeling full quickly after eating. These symptoms can be uncomfortable and impact one’s quality of life. In some cases, complications can arise, such as gastroesophageal reflux disease (GERD), esophagitis, and Barrett’s esophagus.
Gastroesophageal reflux disease (GERD) is a condition that occurs when stomach acid flows back into the esophagus, causing irritation and inflammation. This can lead to symptoms such as heartburn, chest pain, and difficulty swallowing. If left untreated, GERD can cause long-term damage to the esophagus and increase the risk of developing esophageal cancer.
Esophagitis is another potential complication of hiatal hernia. It refers to the inflammation of the esophagus, often caused by the irritation of stomach acid. Symptoms of esophagitis include difficulty swallowing, chest pain, and a burning sensation in the throat. If left untreated, esophagitis can lead to complications such as ulcers, strictures, and bleeding.
Barrett’s esophagus is a condition that occurs when the lining of the esophagus undergoes changes, becoming similar to the lining of the intestine. This change in the lining is believed to be a response to chronic exposure to stomach acid. Barrett’s esophagus is a significant concern as it increases the risk of developing esophageal cancer.
It is crucial to consult with a healthcare professional if any of these symptoms or complications occur, as they can offer appropriate guidance and treatment options. Treatment for hiatal hernias may include lifestyle changes, medication to manage symptoms, and in severe cases, surgical intervention to repair the hernia and restore the normal anatomy of the diaphragm and stomach.
The Vagus Nerve-Hiatal Hernia Connection
Now that we have explored the vagus nerve and hiatal hernia individually, it is important to understand how they interact with each other. The vagus nerve innervates various structures around the esophagus, including the diaphragm and lower esophageal sphincter (LES). The LES is responsible for preventing stomach acid from flowing back into the esophagus. Dysfunction of the vagus nerve can impact the function of the LES, potentially leading to an increased risk of hiatal hernia formation or worsening of symptoms in individuals already diagnosed with a hiatal hernia.
How the Vagus Nerve Influences Hiatal Hernia
Research suggests that the vagus nerve plays a crucial role in maintaining the integrity of the diaphragm and the LES. The vagus nerve sends signals to the LES, instructing it to contract and tighten, which helps to keep the stomach acid where it belongs – in the stomach. Disruptions in vagal function can weaken the LES, making it less effective in preventing stomach acid reflux. This reduced barrier function can contribute to the development or exacerbation of a hiatal hernia.
In addition to its influence on the LES, the vagus nerve also affects digestive motility. It regulates the movement of food and acid through the gastrointestinal tract, ensuring that the process is smooth and efficient. When the vagus nerve is not functioning optimally, digestive motility can be affected, potentially leading to symptoms associated with hiatal hernia, such as bloating, heartburn, and difficulty swallowing.
The Effect of Hiatal Hernia on the Vagus Nerve
While the vagus nerve’s impact on hiatal hernia is well-documented, the reverse relationship is less clear. However, hiatal hernias can cause functional disturbances that may indirectly affect vagal function. For example, increased pressure from a paraesophageal hernia, where a portion of the stomach protrudes through the diaphragm, can compress adjacent structures, potentially leading to vagal nerve compression or irritation. This compression can disrupt the normal function of the vagus nerve, potentially contributing to symptoms associated with vagal dysfunction.
Furthermore, the presence of a hiatal hernia can lead to chronic inflammation in the surrounding tissues. Inflammation can have a negative impact on nerve function, including the vagus nerve. The inflamed tissues can put pressure on the vagus nerve, impeding its ability to transmit signals effectively. This can result in a variety of symptoms, such as nausea, dizziness, and even changes in heart rate.
It is important to note that the relationship between hiatal hernia and vagus nerve dysfunction is complex and multifaceted. Further research is needed to fully understand the mechanisms at play and to develop targeted treatment approaches.
Diagnosis and Treatment Options
Diagnosing both vagus nerve disorders and hiatal hernia requires a comprehensive evaluation, typically involving a combination of medical history, physical examination, and diagnostic tests. Meticulous attention is given to identifying symptoms, assessing the function of the vagus nerve, and determining the presence and severity of a hiatal hernia. A variety of treatment approaches are available, tailored to the individual’s specific condition and symptoms.
When it comes to diagnosing hiatal hernia, various imaging techniques may be used to provide a clearer picture of the condition. X-rays can be helpful in visualizing the position of the stomach and identifying the size and type of the hernia. Another diagnostic tool is the barium swallow test, where the patient swallows a liquid containing barium, which helps highlight any abnormalities in the esophagus and stomach. Additionally, endoscopy may be performed, allowing the doctor to directly visualize the hernia and assess its severity.
On the other hand, diagnosing vagus nerve disorders requires specialized tests to evaluate the function of this important nerve. Autonomic function tests are commonly used to assess the autonomic nervous system, which is regulated by the vagus nerve. These tests measure various physiological responses, such as heart rate, blood pressure, and sweating, to determine if there are any abnormalities. Heart rate variability assessments can also provide valuable information about the vagus nerve’s function, as it plays a crucial role in regulating heart rate. Furthermore, gastrointestinal motility studies may be conducted to evaluate how well the vagus nerve is functioning in relation to the digestive system.
Consulting with a healthcare professional is essential to receive an accurate diagnosis and determine the appropriate treatment plan. They will consider the individual’s symptoms, medical history, and the results of diagnostic tests to develop a personalized treatment approach.
Treatment Approaches for Vagus Nerve and Hiatal Hernia
The treatment approaches for vagus nerve disorders and hiatal hernias vary depending on the severity of symptoms and individual circumstances. For hiatal hernia, lifestyle changes can often be beneficial in managing symptoms. Maintaining a healthy weight is important, as excess weight can put pressure on the stomach and worsen the hernia. Elevating the head of the bed during sleep can help prevent acid reflux, a common symptom of hiatal hernia. Additionally, avoiding trigger foods, such as spicy or fatty foods, can reduce acid reflux and alleviate discomfort. In more severe cases, medications that reduce stomach acid production or surgical interventions may be necessary to repair the hernia and alleviate symptoms.
When it comes to vagus nerve disorders, the treatment focuses on managing underlying conditions and promoting overall health. Lifestyle modifications, such as stress reduction techniques and regular exercise, can help improve vagus nerve function. Stress reduction techniques, such as meditation, deep breathing exercises, and yoga, can help calm the nervous system and enhance vagal tone. In some cases, medications may be prescribed to manage specific symptoms or conditions associated with vagus nerve dysfunction. It is important to follow the guidance of a healthcare professional when considering medication interventions.
In conclusion, diagnosing and treating vagus nerve disorders and hiatal hernias require a comprehensive approach that takes into account the individual’s symptoms, medical history, and diagnostic test results. Lifestyle modifications, medications, and surgical interventions are all potential treatment options, depending on the severity of the condition and the patient’s specific needs. Consulting with a healthcare professional is crucial to receive an accurate diagnosis and develop an appropriate treatment plan.
Prevention and Management Tips
While the development of a hiatal hernia or vagus nerve disorders may not always be preventable, certain strategies can help reduce the risk and manage symptoms effectively.
One important aspect of prevention and management is maintaining a healthy lifestyle. Engaging in activities that promote vagus nerve health, such as deep breathing exercises, mindfulness, regular physical activity, and maintaining social connections, can contribute to overall well-being. These activities help stimulate the vagus nerve and keep it functioning optimally. Additionally, adopting a balanced diet rich in whole foods, fiber, and antioxidants can support proper vagus nerve function. These nutrients provide the necessary building blocks for the nerve to function efficiently and transmit signals effectively.
It is essential to consult with a healthcare professional before making any significant changes to your lifestyle or healthcare routine. They can provide personalized guidance based on your unique circumstances and help you develop a plan that aligns with your specific needs and goals.
Lifestyle Changes to Support Vagus Nerve Health
Engaging in deep breathing exercises is an excellent way to stimulate the vagus nerve. By taking slow, deep breaths and focusing on your breath, you activate the parasympathetic nervous system, which is controlled by the vagus nerve. This can help reduce stress, lower blood pressure, and promote relaxation.
Mindfulness practices, such as meditation and yoga, can also have a positive impact on the vagus nerve. These practices encourage present-moment awareness and help regulate the body’s stress response. By incorporating mindfulness into your daily routine, you can enhance vagus nerve function and promote overall well-being.
Regular physical activity is another crucial aspect of supporting vagus nerve health. Exercise increases blood flow and oxygenation throughout the body, including the vagus nerve. This helps nourish the nerve and keeps it in optimal condition. Whether it’s going for a brisk walk, practicing yoga, or participating in your favorite sport, finding ways to stay active can have a significant impact on your vagus nerve health.
Maintaining social connections is also vital for vagus nerve health. Engaging in meaningful relationships and spending time with loved ones can help reduce stress and promote emotional well-being. The vagus nerve plays a role in regulating social engagement, so nurturing your social connections can have a positive impact on its function.
Additionally, adopting a balanced diet is crucial for supporting vagus nerve health. Including whole foods, such as fruits, vegetables, whole grains, and lean proteins, provides essential nutrients that support nerve function. Fiber-rich foods, like legumes and whole grains, help regulate digestion, which is closely linked to the vagus nerve. Antioxidant-rich foods, such as berries and leafy greens, protect against oxidative stress and inflammation, which can affect nerve health.
It is important to note that while these lifestyle changes can be beneficial for vagus nerve health, individual circumstances may vary. Consulting with a healthcare professional is highly advisable to ensure that these strategies align with your specific needs and medical history.
Tips to Prevent and Manage Hiatal Hernia
Avoiding triggers that worsen acid reflux is key to managing hiatal hernia symptoms. Spicy foods, citrus fruits, and fatty foods are known to exacerbate acid reflux, so minimizing or avoiding them can help alleviate symptoms. Opting for milder spices, non-citrus fruits, and leaner proteins can be a better choice for individuals with hiatal hernia.
Maintaining a healthy weight is also crucial for preventing and managing hiatal hernia. Excess weight puts pressure on the abdomen, which can contribute to the development or worsening of a hiatal hernia. By adopting a balanced diet and engaging in regular physical activity, you can achieve and maintain a healthy weight, reducing the strain on your abdomen and potentially alleviating hiatal hernia symptoms.
Eating smaller, more frequent meals can also be beneficial for individuals with hiatal hernia. Large meals can put additional pressure on the stomach and increase the likelihood of acid reflux. By opting for smaller portions and spacing out your meals throughout the day, you can help prevent symptoms and manage the condition more effectively.
Avoiding lying down immediately after eating is another helpful tip for managing hiatal hernia. When you lie down, gravity no longer helps keep stomach acid in the stomach, which can lead to acid reflux. By staying upright for at least two to three hours after a meal, you can minimize the risk of acid reflux and reduce discomfort.
Elevating the head of the bed during sleep can further alleviate hiatal hernia symptoms. By using bed risers or placing a wedge-shaped pillow under the upper body, you can create an incline that helps prevent stomach acid from flowing back into the esophagus. This can significantly reduce nighttime symptoms and improve sleep quality.
Wearing loose-fitting clothing can also contribute to symptom management. Tight clothing, especially around the waist, can put pressure on the abdomen and potentially worsen hiatal hernia symptoms. Opting for looser clothing allows for more comfortable movement and reduces the likelihood of discomfort.
However, it is important to remember that these lifestyle changes may vary based on individual circumstances. Consulting with a healthcare professional is highly advisable to ensure that these strategies align with your specific needs and medical history. They can provide personalized guidance and recommend additional interventions, such as medication or surgical options, if necessary.
Conclusion
In conclusion, understanding the connection between the vagus nerve and hiatal hernia provides valuable insights into the complex interplay between these two entities. The vagus nerve’s influence on hiatal hernia formation and symptoms underscores the importance of preserving its function through a healthy lifestyle and appropriate medical management. By considering the interaction between the vagus nerve and hiatal hernia, healthcare professionals can develop individualized approaches to diagnose, treat, and prevent these conditions effectively. If you are experiencing symptoms or have concerns related to the vagus nerve or hiatal hernia, consult with a healthcare professional who can provide personalized guidance based on your unique circumstances.
Ready to dive deeper into the wonders of the vagus nerve and its impact on your health, including its role in conditions like hiatal hernia? Discover the secrets of this remarkable nerve with the “My Vagus Nerve & Me Book.” Learn about its extensive functions, from regulating your heart rate and digestion to its involvement in your immune system and mental health. Gain insights on how to nurture and stimulate your vagus nerve for optimal well-being. Don’t miss out on this opportunity to unlock the full potential of your body’s most intricate system. Get My Vagus Nerve & Me eBook today and embark on a journey to better health!