The human body is a complex system of intertwined networks and the connections between different organs and bodily functions are often both fascinating and crucial for our understanding of health and wellbeing. One such connection that has garnered increasing attention in recent years is the relationship between the vagus nerve, gastroesophageal reflux disease (GERD), and tachycardia. In this article, we will delve into the roles played by the vagus nerve in the body, explore the nature and manifestations of GERD and tachycardia, and examine the intricate interplay between these three components.
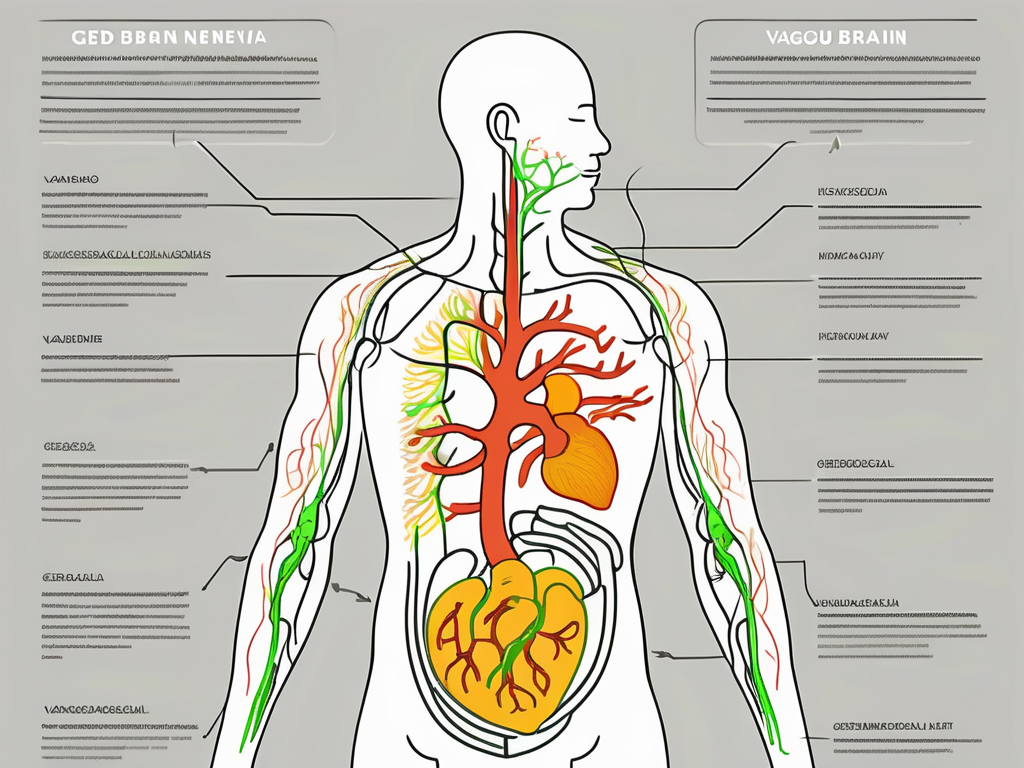
The Role of the Vagus Nerve in the Body
The vagus nerve, also known as the tenth cranial nerve, is a part of the autonomic nervous system that controls many involuntary bodily functions. Originating in the brainstem and extending down into the chest and abdomen, the vagus nerve is responsible for regulating heart rate, digestion, respiratory functions, and more. It is often described as the “wandering” nerve due to its vast network of branches that reach multiple organs and tissues throughout the body.
The Anatomy and Function of the Vagus Nerve
The vagus nerve consists of both sensory and motor fibers, allowing it to convey signals to and from various organs. On the sensory side, it collects information regarding the state of the organs it innervates and relays it back to the brain. This feedback loop is crucial for the body to maintain optimal functioning. For example, if the vagus nerve detects that the stomach is full, it sends a signal to the brain to trigger a feeling of satiety, preventing overeating.
On the motor side, the vagus nerve transmits signals from the brain to control the functioning of these organs. It acts as a messenger, carrying instructions to the organs it innervates, such as the heart, lungs, liver, and intestines. This bidirectional communication enables the vagus nerve to play a pivotal role in maintaining homeostasis within the body.
The Vagus Nerve’s Impact on Heart Rate and Digestion
One of the key functions of the vagus nerve is its influence over heart rate. It acts as a brake on the heart, slowing it down when necessary to maintain a steady rhythm. This ability to regulate heart rate is crucial for overall cardiovascular health. When the body is under stress or in a fight-or-flight response, the vagus nerve helps to counterbalance the increased heart rate, promoting a state of calm and relaxation.
Additionally, the vagus nerve plays a crucial role in the digestion process by enhancing the secretion of digestive enzymes and facilitating the contraction of muscles in the gastrointestinal tract. When we eat, the vagus nerve stimulates the release of stomach acid and digestive enzymes, aiding in the breakdown of food. It also helps to coordinate the rhythmic contractions of the intestines, ensuring proper movement of food through the digestive system.
Beyond its direct impact on heart rate and digestion, the vagus nerve also plays a role in other bodily functions. It influences respiratory functions, helping to regulate breathing rate and depth. The vagus nerve also has an impact on the immune system, with studies suggesting that vagus nerve stimulation can have anti-inflammatory effects. Additionally, it is involved in the regulation of blood pressure, pupil constriction, and even plays a role in vocalization.
Overall, the vagus nerve is a vital component of the autonomic nervous system, with far-reaching effects on various bodily functions. Its intricate network of branches and its ability to communicate bidirectionally with organs make it a key player in maintaining homeostasis and overall well-being. Understanding the role of the vagus nerve can provide valuable insights into the complex interplay between the brain and the body.
Exploring GERD: Gastroesophageal Reflux Disease
Gastroesophageal reflux disease, commonly referred to as GERD, is a chronic condition characterized by the backflow of stomach acid and digestive juices into the esophagus. This occurs when the lower esophageal sphincter, a muscular ring located between the esophagus and the stomach, fails to close properly. The resulting acid reflux can cause a range of uncomfortable symptoms and, if left untreated, may lead to more serious complications.
What is GERD and How Does it Occur?
GERD occurs when the lower esophageal sphincter weakens or relaxes at inappropriate times, allowing stomach acid to flow back into the esophagus. This can occur due to various factors such as obesity, hiatal hernia, pregnancy, or certain medications. The prolonged exposure of the esophagus to stomach acid can result in irritation and inflammation, causing symptoms such as heartburn, chest pain, difficulty swallowing, and a persistent cough.
Obesity is a significant risk factor for developing GERD. Excess weight can put pressure on the stomach, causing the lower esophageal sphincter to weaken and allowing acid to flow back into the esophagus. Additionally, hiatal hernia, a condition where a portion of the stomach protrudes through the diaphragm, can also contribute to the development of GERD. The hernia can disrupt the normal functioning of the lower esophageal sphincter, leading to acid reflux.
Pregnancy is another common factor that can contribute to the development of GERD. The hormonal changes that occur during pregnancy can relax the lower esophageal sphincter, allowing stomach acid to flow back into the esophagus. The growing uterus can also put pressure on the stomach, further exacerbating the symptoms of GERD.
Certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can also increase the risk of developing GERD. These medications can irritate the lining of the stomach and weaken the lower esophageal sphincter, making it easier for acid to reflux into the esophagus.
The Symptoms and Complications of GERD
The symptoms of GERD can range from mild to severe and can have a significant impact on an individual’s quality of life. In addition to heartburn and chest pain, other common symptoms include regurgitation of acid or food, a sour taste in the mouth, and excessive belching.
Individuals with GERD may experience difficulty swallowing, also known as dysphagia. This can occur when the esophagus becomes narrowed due to inflammation or the formation of strictures. Dysphagia can make it challenging to eat and drink, leading to weight loss and malnutrition if not properly managed.
If left untreated, GERD can lead to complications such as esophagitis, which is inflammation of the esophagus. This inflammation can cause pain, difficulty swallowing, and even bleeding. Over time, the constant exposure of the esophagus to stomach acid can lead to the development of strictures, which are narrowings of the esophagus. Strictures can make it difficult for food to pass through the esophagus, causing further swallowing difficulties.
In some cases, GERD can result in the development of Barrett’s esophagus, a condition where the lining of the esophagus undergoes changes that can increase the risk of esophageal cancer. Regular monitoring and treatment are essential for individuals with Barrett’s esophagus to prevent the progression to cancer.
Esophageal cancer is a rare but serious complication of GERD. Prolonged exposure of the esophagus to stomach acid can lead to the development of cancerous cells. Early detection and treatment are crucial for improving outcomes in individuals with esophageal cancer.
Tachycardia: A Closer Look
Tachycardia is a condition characterized by an abnormally rapid heart rate, typically exceeding the normal resting heart rate of 60-100 beats per minute. It can be a transient response to stress or physical exertion, but persistent or recurrent tachycardia may indicate an underlying issue that requires medical attention.
Let’s delve deeper into the world of tachycardia and explore its causes, symptoms, and effects on the body.
Understanding Tachycardia: Causes and Symptoms
Tachycardia can be caused by various factors, such as underlying heart conditions, hormonal imbalances, medications, stimulants, or excessive consumption of caffeine or alcohol. These triggers can disrupt the electrical signals that regulate the heart’s rhythm, leading to a faster heartbeat.
When experiencing tachycardia, individuals may notice a racing or pounding heart, shortness of breath, dizziness, lightheadedness, and even fainting. These symptoms can be alarming and may prompt individuals to seek medical attention.
It is essential to distinguish between different types of tachycardia, as the treatment and potential risks vary depending on the specific underlying cause. Some common types of tachycardia include atrial fibrillation, ventricular tachycardia, and supraventricular tachycardia.
The Effects of Tachycardia on the Body
When the heart beats too quickly, it may not pump blood effectively throughout the body, resulting in compromised organ function. The rapid heartbeat can strain the heart muscles and decrease the amount of blood pumped with each beat. This can lead to reduced blood flow to vital organs, such as the brain, kidneys, and liver.
Prolonged episodes of tachycardia can be physically and mentally taxing. Individuals may experience fatigue, weakness, decreased exercise tolerance, and reduced overall wellbeing. The constant strain on the heart can also increase the risk of developing more severe cardiac conditions, such as heart failure or heart attack.
Moreover, tachycardia can have psychological effects, causing anxiety and panic in some individuals. The fear of experiencing rapid heartbeats can lead to a vicious cycle of increased stress, which can further exacerbate the condition.
It is important to note that tachycardia itself is not a disease but a symptom of an underlying issue. Therefore, proper diagnosis and treatment are crucial to address the root cause and manage the condition effectively.
In conclusion, tachycardia is a condition characterized by an abnormally rapid heart rate. It can be caused by various factors and may present with symptoms such as a racing heart, shortness of breath, and dizziness. Prolonged episodes of tachycardia can have detrimental effects on the body, affecting organ function and overall wellbeing. Seeking medical attention and proper management are essential to prevent further complications and improve quality of life.
The Vagus Nerve-GERD-Tachycardia Connection
The connection between the vagus nerve, GERD, and tachycardia lies in the intricate network of signals and feedback mechanisms that intertwine these components. While the exact mechanisms are not fully understood, researchers have identified several pathways through which the vagus nerve can influence both GERD and tachycardia.
How the Vagus Nerve Influences GERD and Tachycardia
In the case of GERD, the vagus nerve’s function in regulating digestion becomes relevant. The vagus nerve helps stimulate the release of stomach acid and promotes the emptying of the stomach. If there is an imbalance in its signaling, it may contribute to the development or exacerbation of GERD. Additionally, the vagus nerve plays a role in the relaxation of the lower esophageal sphincter, which is responsible for preventing the backflow of stomach acid into the esophagus. Dysfunction in this aspect of vagal control may lead to increased acid reflux and worsen GERD symptoms.
Furthermore, the vagus nerve’s role in heart rate regulation means that dysfunction in this nerve can potentially contribute to the occurrence or persistence of tachycardia. The vagus nerve acts as a brake on the heart, helping to slow down the heart rate during periods of rest and relaxation. However, if there is an imbalance in vagal signaling, it can result in an overactive vagus nerve, leading to a decrease in heart rate variability and potentially causing tachycardia.
The Interplay Between GERD and Tachycardia
GERD and tachycardia can potentially interact with each other, although the precise relationship is still being explored. It is believed that the presence of acid reflux from GERD can stimulate the vagus nerve, leading to an increase in heart rate. This response may be mediated by the release of certain neurotransmitters, such as acetylcholine, which can affect heart rate through its actions on the vagus nerve.
Conversely, the physiological stress of tachycardia may worsen GERD symptoms due to increased pressure within the chest cavity and alterations in the digestive process. The rapid heartbeat and increased cardiac output associated with tachycardia can lead to changes in blood flow and pressure, potentially affecting the function of the lower esophageal sphincter and promoting acid reflux.
Understanding and addressing this interplay is crucial for a comprehensive approach to managing both conditions. By targeting the underlying dysfunctions in the vagus nerve, such as through vagal nerve stimulation or pharmacological interventions, it may be possible to alleviate symptoms of both GERD and tachycardia. Additionally, lifestyle modifications, such as dietary changes and stress management techniques, can also play a significant role in managing these conditions and reducing their impact on daily life.
Treatment Options and Lifestyle Changes
When it comes to managing the vagus nerve, GERD, and tachycardia, a holistic approach is often recommended. Medical treatments may include medications to reduce acid production, regulate heart rate, or address underlying causes. However, it is important to consult with a healthcare professional to determine the most appropriate treatment plan for each individual’s specific situation.
The treatment options for vagus nerve disorders, GERD, and tachycardia are diverse and can vary depending on the severity of the condition and the underlying causes. In some cases, medications such as proton pump inhibitors (PPIs) may be prescribed to reduce stomach acid production and alleviate symptoms of GERD. These medications work by blocking the enzyme in the stomach lining that produces acid, thus reducing the amount of acid that is released into the esophagus.
In addition to PPIs, prokinetic agents may also be used to improve gastric emptying. These medications help to increase the contractions of the muscles in the stomach and intestines, which can aid in the movement of food through the digestive system. By improving gastric emptying, prokinetic agents can help to reduce symptoms such as bloating, nausea, and vomiting.
For individuals with tachycardia, medications may be prescribed to regulate heart rate and rhythm. These medications, known as antiarrhythmics, work by restoring the normal electrical activity of the heart and preventing abnormal heart rhythms. They can help to control the heart rate and reduce symptoms such as palpitations, dizziness, and shortness of breath.
In some cases, surgical interventions or medical devices may be recommended to address underlying issues or manage symptoms. For example, individuals with severe GERD may undergo a surgical procedure called fundoplication, which involves wrapping the upper part of the stomach around the lower esophagus to strengthen the valve between the esophagus and stomach. This can help to prevent acid reflux and alleviate symptoms.
Aside from medical treatments, lifestyle modifications can play a significant role in managing these conditions. Dietary adjustments are often recommended, such as avoiding trigger foods that can exacerbate symptoms of GERD, such as spicy or fatty foods, citrus fruits, and caffeine. Eating smaller and more frequent meals can also help to reduce the pressure on the stomach and minimize acid reflux.
Other lifestyle changes that can be beneficial include maintaining a healthy weight, as excess weight can put pressure on the abdomen and increase the risk of acid reflux. Elevating the head of the bed by using a wedge pillow or raising the head of the bed can help to prevent acid from flowing back into the esophagus during sleep. Avoiding tight clothing, especially around the waist, can also help to reduce pressure on the stomach and minimize symptoms.
Engaging in stress management techniques, such as meditation, deep breathing exercises, or yoga, can also be helpful in managing these conditions. Stress has been known to exacerbate symptoms of GERD and tachycardia, so finding ways to relax and reduce stress levels can have a positive impact on overall well-being.
It is important to note that lifestyle changes can differ for each individual, so it is advisable to seek guidance from a healthcare professional in designing a personalized plan. They can provide tailored recommendations based on the specific needs and circumstances of each individual, ensuring that the treatment approach is effective and sustainable.
Future Research Directions
The connections between the vagus nerve, GERD, and tachycardia continue to be a subject of ongoing research. As our understanding of these relationships deepens, new treatment modalities and innovative strategies may emerge to better manage and improve patient outcomes.
The Potential for New Treatments and Therapies
Advancements in medical research may lead to the development of novel treatments and therapies that specifically target the vagus nerve, GERD, and tachycardia. For example, neuromodulation techniques that aim to modify the activity of the vagus nerve are being explored as potential treatments for various conditions, including GERD and tachycardia. These techniques involve the use of electrical impulses or targeted medications to regulate the nerve’s activity and potentially alleviate symptoms. Additionally, advancements in diagnostic tools and precision medicine approaches may allow for more targeted treatment plans tailored to individual patients’ needs.
Researchers are also investigating the potential benefits of non-invasive therapies, such as transcutaneous vagus nerve stimulation (tVNS). This technique involves applying electrical stimulation to the skin overlying the vagus nerve, which may modulate its activity and potentially provide relief for GERD and tachycardia symptoms. Early studies have shown promising results, but further research is needed to determine its effectiveness and long-term benefits.
Unanswered Questions and Areas for Further Study
While significant progress has been made in unraveling the relationship between the vagus nerve, GERD, and tachycardia, there are still many unanswered questions and areas for further study. Researchers are working to elucidate the underlying mechanisms that link these conditions, refine diagnostic approaches, explore potential risk factors, and enhance treatment efficacy.
One area of ongoing research focuses on the gut-brain axis, which involves bidirectional communication between the gastrointestinal system and the central nervous system. Understanding how the vagus nerve, which plays a crucial role in this axis, influences GERD and tachycardia could provide valuable insights into potential treatment targets. Additionally, investigating the impact of lifestyle factors, such as diet and stress, on the vagus nerve’s function and its relationship to these conditions may help identify new avenues for intervention.
Furthermore, researchers are exploring the potential role of inflammation in the development and progression of GERD and tachycardia. Chronic inflammation in the gastrointestinal tract and cardiovascular system may contribute to the symptoms experienced by individuals with these conditions. Investigating the underlying inflammatory processes and their interaction with the vagus nerve could lead to the development of targeted anti-inflammatory therapies.
Continued research efforts hold the promise of a better understanding and management of these conditions in the future. By uncovering the intricate mechanisms at play and identifying novel therapeutic targets, researchers aim to improve patient outcomes and enhance quality of life for individuals affected by GERD and tachycardia.
Conclusion:
In conclusion, the relationship between the vagus nerve, GERD, and tachycardia is a fascinating area of study in the field of medical research. Understanding the anatomy and function of the vagus nerve, along with the complexities of GERD and tachycardia, allows us to appreciate the interconnectedness of different bodily systems. It highlights the importance of comprehensive approaches to management that encompass both medical treatments and lifestyle modifications.
As research continues to shed light on this intricate connection, it is important for individuals experiencing symptoms related to GERD or tachycardia to consult with a healthcare professional for a thorough evaluation and guidance on appropriate management options. By staying informed about the latest research findings and advancements, patients and healthcare providers can work together to optimize treatment strategies and improve patient outcomes.
If you’re intrigued by the vital role the vagus nerve plays in conditions like GERD and tachycardia, and you’re eager to learn more about this remarkable nerve that orchestrates so many of your body’s essential functions, then “My Vagus Nerve & Me Book” is the perfect resource for you. Dive deep into the world of the vagus nerve with our comprehensive eBook, where you’ll discover the intricacies of its anatomy, the breadth of its regulatory powers, and practical ways to stimulate it for better health. Whether you’re looking to enhance your immune system, improve digestion, regulate your heart rate, or support your mental health, this book has the insights you need. Take the first step towards harnessing the power of your vagus nerve for a healthier, more balanced life. Get My Vagus Nerve & Me eBook today and embark on a journey of discovery and well-being.