Vertigo is a common health condition that can have a significant impact on an individual’s quality of life. It is characterized by a spinning sensation or a feeling of dizziness, often accompanied by nausea and imbalance. While there can be various causes for vertigo, one connection that has been increasingly studied is the link between the vagus nerve and vertigo. In this article, we will explore the role of the vagus nerve in relation to vertigo, recent medical research findings, and practical tips for managing vertigo symptoms.
An Overview of the Vagus Nerve
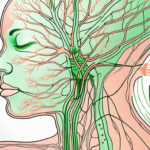
The vagus nerve, also known as the tenth cranial nerve, is one of the longest and most complex nerves in the body. It originates in the brainstem and extends down through the neck, chest, and abdomen, reaching various organs along the way. The vagus nerve plays a crucial role in regulating many bodily functions, including heart rate, digestion, and respiratory functions.
The vagus nerve, often referred to as the “wandering nerve,” gets its name from its extensive and intricate pathway throughout the body. It branches out like a network of highways, connecting the brain to various organs such as the heart, lungs, liver, stomach, and intestines. This extensive reach allows the vagus nerve to have a significant impact on multiple bodily systems.
The Role and Function of the Vagus Nerve
The primary function of the vagus nerve is to control the parasympathetic nervous system, which is responsible for promoting relaxation and restorative processes in the body. It helps regulate heart rate, promoting a sense of calm and balance. When activated, the vagus nerve releases acetylcholine, a neurotransmitter that slows down the heart rate and lowers blood pressure. This calming effect is essential for maintaining overall cardiovascular health.
In addition to its role in heart rate regulation, the vagus nerve also plays a crucial role in digestion. It stimulates the production of stomach acid and digestive enzymes, aiding in the breakdown and absorption of nutrients. Furthermore, the vagus nerve helps coordinate the movement of food through the digestive tract, ensuring efficient digestion and absorption.
Moreover, the vagus nerve has been found to have anti-inflammatory effects. It can reduce the production of pro-inflammatory molecules and promote the release of anti-inflammatory substances, helping to modulate the body’s immune response. This anti-inflammatory action is vital for maintaining a healthy immune system and preventing chronic inflammation, which is linked to various diseases.
Interestingly, the vagus nerve also has an impact on mood and emotional responses. It connects to areas of the brain involved in regulating emotions, such as the amygdala and prefrontal cortex. Activation of the vagus nerve has been shown to reduce anxiety and improve mood, highlighting its role in emotional well-being.
Anatomy of the Vagus Nerve
The vagus nerve consists of both sensory and motor fibers. The sensory fibers transmit signals from various organs back to the brain, providing information about the body’s internal environment. For example, sensory fibers in the stomach send signals to the brain about feelings of fullness or hunger. This feedback loop allows the brain to make appropriate adjustments to maintain homeostasis.
On the other hand, the motor fibers of the vagus nerve carry signals from the brain to the organs, enabling the brain to control their functions. For instance, the brain can send signals through the vagus nerve to increase or decrease heart rate, depending on the body’s needs. This bidirectional communication allows for precise regulation of bodily functions.
The vagus nerve is not just a single nerve but a complex network of interconnected fibers. It branches out extensively, forming connections with other nerves and creating a vast communication network within the body. This intricate web of connections allows for efficient coordination of various physiological processes and ensures the proper functioning of the body as a whole.
Understanding Vertigo
Vertigo is often described as a spinning sensation or feeling like the world is spinning around you. It can be caused by various factors, including inner ear disorders, migraines, medication side effects, or underlying health conditions. Some of the common symptoms of vertigo include dizziness, imbalance, nausea, vomiting, and difficulty concentrating.
Vertigo can have a significant impact on a person’s daily life. Imagine waking up in the morning, ready to start your day, only to be hit with a sudden wave of dizziness and a feeling that the room is spinning. Simple tasks like getting out of bed or walking down the stairs become a challenge. The fear of falling or losing control can be overwhelming, leading to anxiety and a decreased quality of life.
Causes and Symptoms of Vertigo
Vertigo can occur due to a disruption in the inner ear’s balance mechanisms, which are responsible for detecting head position and movement. The inner ear is a complex structure consisting of fluid-filled canals and tiny hair-like sensors. When these sensors are not functioning properly, they send incorrect signals to the brain, resulting in the sensation of vertigo.
Inflammation of the inner ear, also known as labyrinthitis, is a common cause of vertigo. This inflammation can be triggered by viral or bacterial infections, leading to a disruption in the delicate balance within the inner ear. The symptoms of labyrinthitis can be severe, with intense dizziness, nausea, and even hearing loss.
Another common cause of vertigo is benign paroxysmal positional vertigo (BPPV). This condition occurs when tiny calcium crystals in the inner ear become dislodged and float into one of the fluid-filled canals. These crystals interfere with the normal flow of fluid, causing the sensation of vertigo. BPPV is often triggered by certain head movements, such as rolling over in bed or looking up.
Meniere’s disease is a chronic condition that affects the inner ear and can cause recurring episodes of vertigo. Along with vertigo, individuals with Meniere’s disease may experience hearing loss, tinnitus (ringing in the ears), and a feeling of fullness or pressure in the affected ear. The exact cause of Meniere’s disease is unknown, but it is believed to be related to fluid buildup in the inner ear.
Vertigo can also be a symptom of vestibular migraine, a type of migraine headache that is characterized by vertigo or dizziness. These migraines are often accompanied by other symptoms, such as headache, sensitivity to light and sound, and visual disturbances. Vestibular migraines can be debilitating, making it difficult for individuals to carry out their daily activities.
Common Treatments for Vertigo
Treatment for vertigo depends on the underlying cause. In some cases, the symptoms may resolve on their own, especially if the vertigo is caused by a viral infection or a temporary disruption in the inner ear. However, for more persistent or severe cases, medical intervention might be necessary.
Medication can be prescribed to alleviate the symptoms of vertigo. These medications may include anti-nausea drugs, such as meclizine, to help control the nausea and vomiting associated with vertigo. Other medications, such as antihistamines or benzodiazepines, may be used to reduce dizziness and improve balance.
In addition to medication, exercises can be performed to improve balance and coordination. These exercises, known as vestibular rehabilitation therapy, involve specific head and body movements that help retrain the brain to compensate for the inner ear’s dysfunction. Vestibular rehabilitation therapy can be highly effective in reducing the frequency and severity of vertigo episodes.
In rare cases, surgical procedures may be considered for individuals with severe and persistent vertigo that does not respond to other treatments. These procedures aim to correct the underlying cause of vertigo, such as removing a tumor or repairing a damaged inner ear structure. Surgical intervention is usually reserved for cases where all other treatment options have been exhausted.
It is important to consult with a healthcare professional to determine the most appropriate treatment plan for vertigo. Each individual’s situation is unique, and a thorough evaluation is necessary to identify the underlying cause and develop an effective treatment strategy. With the right approach, vertigo can be managed, allowing individuals to regain control of their lives and enjoy a better quality of life.
The Vagus Nerve-Vertigo Connection
Research has suggested that the vagus nerve may play a role in the development and modulation of vertigo symptoms. Although the exact mechanisms are still being studied, it is believed that the vagus nerve’s influence on various bodily processes, including inflammation and autonomic nervous system regulation, may contribute to the occurrence and severity of vertigo episodes.
How the Vagus Nerve Influences Vertigo
Studies have indicated that the vagus nerve’s activation or stimulation can impact the vestibular system, which is responsible for detecting changes in head position and movement. By modulating the activity of the vestibular system, the vagus nerve may influence the perception of balance and contribute to vertigo symptoms. However, further research is necessary to fully understand this complex interaction.
One possible explanation for the vagus nerve’s influence on vertigo is its role in regulating inflammation. Inflammation is a natural response of the immune system to injury or infection, but excessive or chronic inflammation can have detrimental effects on various bodily functions. It has been suggested that the vagus nerve, through its anti-inflammatory properties, may help regulate the inflammatory response in the inner ear, which could potentially impact the occurrence and severity of vertigo episodes.
Furthermore, the vagus nerve is also involved in the regulation of the autonomic nervous system, which controls involuntary bodily functions such as heart rate, blood pressure, and digestion. Dysregulation of the autonomic nervous system has been implicated in various vestibular disorders, including vertigo. The vagus nerve’s influence on autonomic functions may therefore contribute to the development and modulation of vertigo symptoms.
The Impact of Vagus Nerve Stimulation on Vertigo
Vagus nerve stimulation (VNS) is a therapeutic approach that involves the use of mild electrical pulses to stimulate the vagus nerve. While VNS has shown promise in the treatment of various neurological and psychiatric disorders, its role in managing vertigo is still under investigation.
Some studies have suggested potential benefits of VNS in reducing vertigo symptoms. The electrical stimulation of the vagus nerve may help regulate the abnormal neural activity associated with vertigo, leading to a decrease in the frequency and severity of vertigo episodes. Additionally, VNS may also have indirect effects on other areas of the brain that are involved in balance and spatial orientation, further contributing to its potential therapeutic effects.
However, it is important to note that the use of VNS for vertigo is still considered experimental, and more research is needed to establish its efficacy and safety in this context. Clinical trials are currently underway to evaluate the effectiveness of VNS as a treatment option for vertigo, and the results of these studies will provide valuable insights into the potential benefits and limitations of this approach.
In conclusion, the vagus nerve appears to have a significant influence on the development and modulation of vertigo symptoms. Its impact on the vestibular system, inflammation regulation, and autonomic nervous system regulation may all contribute to the occurrence and severity of vertigo episodes. While VNS shows promise as a potential therapeutic approach for vertigo, further research is necessary to fully understand its mechanisms of action and establish its effectiveness in clinical practice.
Medical Research on the Vagus Nerve and Vertigo
Medical research on the vagus nerve’s connection to vertigo has been an area of growing interest. Recent findings have shed light on the potential mechanisms underlying this relationship and opened doors for new treatment possibilities.
Vertigo, a sensation of spinning or dizziness, can be debilitating and significantly impact a person’s quality of life. It is often caused by problems in the inner ear, but recent studies have suggested that the vagus nerve may also play a role in its development and severity.
Recent Findings and Developments
A study published in the Journal of Vestibular Research found that vagus nerve dysfunction may be associated with increased vertigo symptoms in individuals with vestibular migraine. This highlights the importance of considering the vagus nerve’s role in assessing and managing vertigo cases, particularly in individuals with migraines.
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It is responsible for regulating various bodily functions, including heart rate, digestion, and even mood. Recent research has shown that it also has connections to the vestibular system, which is responsible for maintaining balance and spatial orientation.
Further studies have revealed that the vagus nerve may influence the release of neurotransmitters in the brain, such as serotonin and gamma-aminobutyric acid (GABA), which play a crucial role in regulating the vestibular system. Dysfunction of the vagus nerve could disrupt the delicate balance of these neurotransmitters, leading to vertigo symptoms.
Additionally, researchers have found that the vagus nerve may interact with other structures involved in vertigo, such as the trigeminal nerve, which is responsible for sensation in the face and head. This interaction suggests a complex network of neural pathways that contribute to the development and perception of vertigo.
Implications for Future Treatment
The growing understanding of the vagus nerve’s involvement in vertigo holds promise for future treatment approaches. Targeted therapeutic interventions aimed at modulating the vagus nerve’s activity or influencing its interactions with the vestibular system may provide new avenues for managing vertigo symptoms.
For example, vagus nerve stimulation, a technique that involves delivering electrical impulses to the nerve, has shown promise in treating various neurological conditions, including epilepsy and depression. It is possible that this approach could be adapted for vertigo treatment, helping to regulate the nerve’s activity and alleviate symptoms.
Furthermore, researchers are exploring the potential of pharmacological interventions that target the vagus nerve. By developing drugs that specifically modulate the nerve’s function, it may be possible to provide relief to individuals suffering from vertigo. However, further research is necessary to explore these possibilities and ensure their safety and efficacy.
In conclusion, the vagus nerve’s role in vertigo is an exciting area of medical research. Recent findings have provided valuable insights into the mechanisms underlying this relationship, highlighting the potential for novel treatment approaches. As our understanding of the vagus nerve continues to expand, it is hoped that new therapies will emerge, offering relief to those affected by vertigo.
Practical Tips for Managing Vertigo
Vertigo is a condition characterized by a spinning sensation, often accompanied by dizziness, nausea, and difficulty maintaining balance. While medical advice should always be sought for evaluation and treatment of vertigo, there are some practical tips that individuals experiencing vertigo can incorporate into their daily lives to help manage their symptoms.
One of the most important aspects of managing vertigo is making lifestyle changes. Simple adjustments to daily routines can sometimes make a significant difference in reducing the frequency and severity of vertigo episodes. For example, individuals may find it helpful to avoid triggers such as certain foods or beverages that can exacerbate their symptoms. Common triggers include caffeine, alcohol, and foods high in salt or sugar.
Getting enough rest and sleep is also crucial for managing vertigo. Fatigue can worsen symptoms and make it more challenging to cope with the spinning sensation. By prioritizing rest and establishing a consistent sleep schedule, individuals can give their bodies the opportunity to recover and reduce the likelihood of vertigo episodes.
Stress management techniques can also play a role in managing vertigo symptoms. Stress and anxiety can trigger or worsen vertigo, so finding effective ways to relax and reduce stress levels is essential. This can include activities such as meditation, deep breathing exercises, yoga, or engaging in hobbies that bring joy and relaxation.
Staying hydrated is another important aspect of managing vertigo. Dehydration can contribute to dizziness and lightheadedness, which can exacerbate vertigo symptoms. By drinking an adequate amount of water throughout the day, individuals can help maintain their body’s fluid balance and potentially reduce the severity of vertigo episodes.
Maintaining regular exercise can also be beneficial for managing vertigo. Engaging in physical activity helps improve overall balance and coordination, which can help individuals better cope with the spinning sensation. It is important to note that individuals should consult with their healthcare provider before starting any exercise regimen to ensure it is safe and appropriate for their specific condition.
In addition to lifestyle changes, there are some home remedies that may be recommended by a healthcare professional to help alleviate vertigo symptoms in specific cases. One such remedy is head positioning exercises, which involve moving the head in specific positions to dislodge any particles that may be causing vertigo. Another technique called canalith repositioning maneuvers can also be effective in repositioning these particles and providing relief from vertigo.
When to Seek Medical Help
While lifestyle changes and home remedies may provide relief for some individuals, it is essential to consult with a healthcare professional for a comprehensive evaluation and tailored treatment plan. Medical intervention may be necessary, especially if vertigo symptoms are severe, persistent, or interfering with daily functioning.
A healthcare provider can conduct a thorough assessment, perform diagnostic tests if required, and recommend the most appropriate course of action based on an individual’s unique circumstances. Treatment options may include medications to alleviate symptoms, physical therapy to improve balance and coordination, or in some cases, surgical intervention.
It is important to remember that vertigo can have various underlying causes, such as inner ear disorders, vestibular migraines, or even certain medications. Therefore, a healthcare professional’s expertise is crucial in identifying the root cause of vertigo and developing an effective treatment plan.
In conclusion, while medical intervention and consultation with a healthcare professional are crucial for diagnosing and treating vertigo, individuals can also incorporate lifestyle changes and home remedies under medical supervision to help manage their symptoms more effectively. By making simple adjustments to their daily routines, individuals can potentially reduce the frequency and severity of vertigo episodes, improving their overall quality of life.
With the advancements in medical research, the future may hold innovative approaches that target the vagus nerve for more targeted and personalized vertigo treatment. Understanding the connection between the vagus nerve and vertigo is an ongoing area of research that holds promising implications for the management of this debilitating condition.
It is an exciting time in the field of vertigo research, as scientists continue to unravel the complexities of this condition and develop new treatment strategies. By staying informed and working closely with healthcare professionals, individuals can navigate the challenges of vertigo and find effective ways to manage their symptoms, ultimately improving their overall well-being.
If you’re fascinated by the critical role the vagus nerve plays in your health and are eager to delve deeper into its functions and the ways to nurture it, “My Vagus Nerve & Me Book” is the perfect resource for you. Discover the secrets of this remarkable system that orchestrates your heart rate, digestion, immune response, and so much more. Learn practical tips on how to stimulate your vagus nerve both naturally and artificially, enhancing your overall well-being. Embrace the opportunity to unlock the full potential of your body’s most astonishing nerve. Get My Vagus Nerve & Me eBook today and take the first step towards a deeper understanding of your inner workings and improved health.