Recurrent seizures are a neurological condition known as epilepsy. It is a complicated tapestry that is woven throughout the lives of numerous people in the modern world. One phrase that frequently comes up among the many aspects of this illness is refractory epilepsy. Together, we will set out on a quest to uncover the meaning behind this mysterious term.
In essence, epilepsy that is resistant to conventional therapy approaches is called resistant epilepsy. Think of it as a tough enemy that refuses to be defeated by the usual drugs used to stop seizures. Although antiepileptic medications provide relief for the majority of epileptics, there is a subgroup for whom these treatments are unsatisfactory.
The etiology of refractory epilepsy is as varied as the range of human experiences it affects. Genetic predispositions might set the stage, entwining themselves with the intricate network of abnormalities in brain anatomy. Infections, strokes, and head traumas can also leave shadows that increase the brain’s susceptibility to defiant seizures. Refractory epilepsy is like a puzzle where every piece—genetic or environmental—contributes to the complex whole.
So how can one spot the presence of such a powerful foe? Refractory epilepsy shares symptoms with its more prevalent counterpart, seizures. But they get more frequent and intense, which has a significant effect on day-to-day living. Imagine navigating a world where uncertainty looms over every move you make.
Refractory epilepsy treatment crosses the line into specialized care. The application of electrical impulses to alter brain function, or neurostimulation, appears to be a promising development. Surgical therapies, where precision meets brain complexity to create a path toward seizure control, may also be investigated.
Refractory epilepsy necessitates a multidisciplinary approach outside of the medical domain. To people who are struggling with the uncertainty this condition entails, emotional support becomes a lifeline. Like holding a lantern in the dark, a sympathetic understanding can make a big difference.
Intractable Vs Refractory Epilepsy
A challenging clinical situation in which seizures remain unresponsive to multiple therapeutic attempts is intractable epilepsy. This resistance suggests that obtaining seizure control with traditional therapy methods will be extremely difficult. People with uncontrollably severe epilepsy frequently go through a depressing cycle of trying various drugs and therapies with little to no success. The phrase emphasizes how frustrating it may be for both patients and medical professionals to deal with ongoing seizure activity that doesn’t respond to early treatment attempts.
While there are similarities between intractable epilepsy and refractive epilepsy, the former adopts a more focused approach. It is used to characterize seizures that continue even after careful adherence to a sufficient and well-chosen antiepileptic medication regimen (AED). The word “refractory” here refers to the seizures’ resistance to medication treatments that would typically work on the wider population.
The term “refractory” is frequently used to highlight the fact that the seizures are persistent after a thorough trial of various drugs has been completed.
Similarities: Intractable and refractory epilepsy both highlight how complex and multifaceted seizure management can be for some people. The intricate nature results from the interaction of genetic variables, differences in the architecture of the brain, and the distinct way that neural circuits react to interventions. The need for more individualized and creative approaches to seizure management is highlighted by the failure of numerous medications and the persistence of seizures despite adherence to treatment regimens. These terms function as clinical indicators, assisting medical practitioners in identifying the difficulties encountered by people whose seizures resist standard control measures.
Causes of Cogwheeling in Refractory Seizures Epilepsy
Due to multiple factors, cogwheeling can be seen in refractory seizures in epilepsy. These include inherited tendencies, abnormalities in the structure of the brain, and other external factors. The abnormalities in brain circuit coordination are complex and difficult to pinpoint to a single cause, especially when they occur in the setting of seizures that do not respond to conventional therapies.
Here are some of the possible causes of cogwheeling
1. Genetic Predispositions: In refractory seizures, cogwheeling may occur due to specific genetic factors. Genetic differences can affect how neural pathways function and have the ability to predispose people to a particular seizure-related phenomenon.
2. Brain Structural Abnormalities: The emergence of cogwheeling in refractory seizures is largely dependent on abnormalities in the structure of the brain. The jerky movements that have been observed could be caused by structural irregularities interfering with the smooth coordination of neural circuits.
3. External Influences: In refractory seizures, external factors like triggers or stressors in the environment may make cogwheeling symptoms worse. These outside factors could interact with underlying structural and genetic factors to produce a complex network of factors that contribute to movements associated with seizures.
Cogwheeling in refractory seizures is caused by specific mechanisms that must be understood, and this requires a thorough analysis of each case.
Refractory Epilepsy With Lung Involvement Syndromes
Refractory epilepsy linked to syndromes with lung manifestations adds a complex element to the clinical picture. This fascinating combination of respiratory and neurological complexity calls into question what is generally thought regarding epilepsy.
Neurological Component: The basis of this complex scenario is Refractory Epilepsy, which is characterized by seizures that are resistant to conventional therapeutic interventions. The neurological foundations comprise a variety of elements, such as genetic susceptibilities, anatomical abnormalities in the brain, and the complex web of neural pathways that contribute to the refractory nature of seizures.
Respiratory Involvement Syndromes: These syndromes add a unique component and layers of issues to the clinical picture when they involve lung manifestations. These syndromes can include a variety of respiratory problems, from structural pathologies in the pulmonary system to functional abnormalities.
It has often been shown that altered respiratory function is associated with epileptic discharges. Respiratory abnormalities, most notably brief episodes of apnea, were regularly noted in petit mal seizures. Whether respiratory arrest occurred during inspiration or expiration was determined by the respiratory cycle phase that corresponded with the beginning of the epileptic discharge.
Similar respiratory changes have been observed in the setting of focal epilepsy, especially in those cases of leptazol-induced temporal lobe epilepsy (4).
Studies have demonstrated that certain brain regions, such as the anterior cingulate gyrus, deep temporal structures, and occasionally the inferior parts of the sensorimotor region, can cause respiratory arrest in people.
These respiratory changes are especially important when refractory epilepsy with lung involvement syndromes is present. Refractory epilepsy adds a level of complexity due to its persistent and treatment-resistant nature, which may make respiratory issues related to epileptic discharges worse. It becomes essential to comprehend the nuances of these respiratory alterations to provide patients with refractory epilepsy and concurrent lung involvement syndromes with comprehensive care.
What Are The Options For Treating Refractory Epilepsy?
Adjusting Medications
Polypharmacy: This strategy involves combining multiple antiepileptic drugs (AEDs) to address refractory epilepsy. The rationale behind polypharmacy is to target seizures through different mechanisms of action, aiming for a more comprehensive and effective seizure control(5). Fine-tuning the dosage of existing medications is a critical aspect of managing refractory epilepsy. This process involves optimizing the balance between achieving adequate seizure control and minimizing side effects. It requires close monitoring of the individual’s response to the medication and may involve gradual adjustments to find the most effective and tolerable dosage(6).
Dietary Changes
Ketogenic Diet: A high-fat, low-carbohydrate diet that alters the body’s metabolism and has shown efficacy in reducing seizures. The ketogenic diet helps some individuals with epilepsy. It is a high-fat, no-carb, low-protein diet. You have to start following orders from your medical practitioners to be properly supervised.
Surgical Interventions:
Resective Surgery: This involves the surgical removal of the brain region responsible for seizures, often considered focal epilepsy.
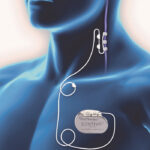
Responsive Neurostimulation (RNS): This method involves Implanting a device that monitors brain activities and delivers targeted stimulation to interrupt the onset of seizures.
Vagus Nerve Stimulation (VNS): Placing a device under the skin that stimulates the vagus nerve, potentially reducing seizure frequency. This device sends current to the nerve, which potentially reduces the number of seizures a person gets or reduces the intensity of the seizures.
Lifestyle Modifications:
Sleep Management: Ensuring consistent sleep patterns to minimize seizure triggers.
Avoid Stress: Implementing stress management techniques, such as mindfulness or relaxation exercises, to mitigate seizure risk.
Clinical Trials:
Experimental Treatments: You may ask about the possibility of Participating in research studies testing innovative therapies and medications for refractory epilepsy.
Continuous Monitoring and Adjustments:
Regular Follow-ups: Frequent consultations with healthcare providers for ongoing evaluation, ensuring that treatment plans are dynamic and responsive to the evolving nature of refractory epilepsy.
Refractory Epilepsy in Children vs Adults
Children with refractory epilepsy may present differently from adults with the condition, which is marked by seizures that are not controlled by common antiepileptic drugs. Here are some significant differences:
Developmental anomalies, genetic factors, or structural abnormalities that may have started during pregnancy or the period immediately after conception are frequently the underlying causes of pediatric refractory epilepsy, whereas, in adults, these factors are usually more common. Brain tumors, cerebrovascular accidents, and head injuries are among the acquired conditions that may be linked to Refractory Epilepsy. As people age, neurodegenerative diseases and specific infections become more common causes.
⦁ Types of Epilepsy
Refractory epilepsy in children is more frequently linked to specific epilepsy syndromes, such as Lennox-Gastaut syndrome or Dravet syndrome whereas in adults, Refractory cases of focal epilepsies associated with temporal lobe epilepsy or structural brain lesions are more common.
⦁ Effect on Mental Development
Childhood-onset reflexive epilepsy can significantly affect cognitive development. Learning disabilities or behavioral issues may be brought on by recurrent seizures or drug side effects. Whereas The duration and level of seizure control of adults with epilepsy may have an impact on their cognitive function. Long-term uncontrollably occurring seizures may be a factor in cognitive aging.
⦁ Modes of Treatment:
When treating pediatric patients, a multidisciplinary approach that takes their developmental and educational needs into account is frequently used. Dietary treatments such as the ketogenic diet could be taken into account. In adults, the emphasis is frequently on optimizing pharmacological interventions and also taking into account possible effects on quality of life and day-to-day functioning.
⦁ Psychosocial Effect:
Children with resistant epilepsy may experience difficulties in their social interactions and academic performance, necessitating extra help from educators and carers while adults may experience difficulties with their jobs, relationships, and general quality of life.
Best Medication For Refractory Epilepsy
Determining the best medication for refractory epilepsy is highly individualized and depends on various factors, including the type of seizures, underlying causes, and individual response to medications. There is no one-size-fits-all solution, and sometimes treatment involves a trial-and-error process. However, here are some common medications used in the management of refractory epilepsy (7)
1. Levetiracetam (Keppra): Levetiracetam is often used as an adjunctive therapy in refractory epilepsy. It has a broad spectrum of activity and is well-tolerated in many patients.
2. Lamotrigine (Lamictal): Lamotrigine is used in various types of epilepsy and is considered in cases of refractory seizures. It may be particularly effective in certain focal epilepsies.
3. Topiramate (Topamax): Topiramate is another antiepileptic drug with broad-spectrum activity. It is considered in refractory cases, especially when other medications have not provided sufficient seizure control.
4. Zonisamide (Zonegran): Zonisamide is used as an adjunctive therapy in refractory epilepsy. It may be considered in various seizure types, including focal seizures.
5. Clobazam (Onfi): Clobazam, a benzodiazepine derivative, is used in refractory epilepsies, especially in the treatment of certain types of seizures associated with Lennox-Gastaut syndrome.
6. Perampanel (Fycompa): Perampanel is a newer antiepileptic drug that works as an AMPA receptor antagonist. It is considered in refractory cases, particularly in focal epilepsy.
References
https://epilepsysociety.org.uk/sites/default/files/2020-08/Epilepsy-Notes-PDF-Book-2019-low.pdf
https://pubmed.ncbi.nlm.nih.gov/25602999/
https://pubmed.ncbi.nlm.nih.gov/15111660/
National Institutes of Health (.gov)https://pubmed.ncbi.nlm.nih.gov › …Definition of drug-resistant epilepsy: consensus proposal by the ad hoc Task …
https://www.webmd.com/epilepsy/refractory-epilepsy