The vagus nerve is a crucial component of the human nervous system, playing a vital role in the neck and its various functions. In this comprehensive guide, we will explore the anatomy, functions, disorders, diagnosis, and treatment options related to the vagus nerve. It is important to note that while this article provides valuable information, it is not intended to serve as medical advice. For any concerns regarding your health, it is always recommended to consult with a healthcare professional.
Understanding the Vagus Nerve
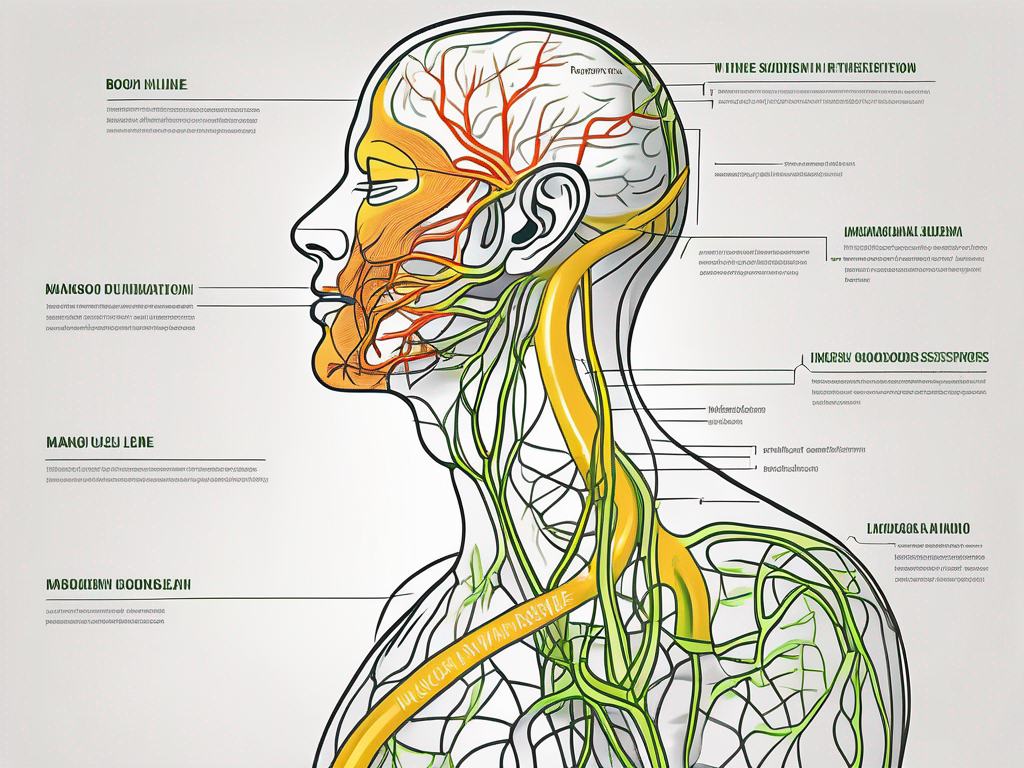
The vagus nerve, also known as the tenth cranial nerve, is one of the longest and most complex nerves in the human body. It originates in the brainstem and extends down through the neck to the abdomen, innervating various organs along its pathway.
The vagus nerve is a fascinating structure that has captivated the attention of scientists and medical professionals for centuries. Its intricate anatomy and vital functions make it a topic of great interest and research.
Anatomy of the Vagus Nerve
The vagus nerve consists of both sensory and motor fibers. It is divided into two main branches: the superior vagal ganglion and the inferior vagal ganglion. These branches provide innervation to numerous structures, including the neck muscles, heart, lungs, and digestive system.
The superior vagal ganglion is located in the medulla oblongata, a part of the brainstem responsible for controlling vital functions. From there, it sends out fibers that travel down the neck, branching out to innervate the muscles responsible for swallowing and speaking.
The inferior vagal ganglion, on the other hand, is situated in the chest and abdomen. It sends fibers to the heart, where it helps regulate heart rate and blood pressure. Additionally, it extends to the lungs, where it controls the rate and depth of breathing. The vagus nerve also plays a crucial role in the digestive system, providing innervation to the stomach, liver, and intestines.
Functions of the Vagus Nerve
The vagus nerve plays a crucial role in regulating many bodily functions, including heart rate, digestion, breathing, and vocalization. It is responsible for transmitting sensory information from organs to the brain and controlling motor responses.
One of the most well-known functions of the vagus nerve is its role in the parasympathetic nervous system, which is responsible for promoting rest and relaxation. When the vagus nerve is activated, it slows down the heart rate, increases digestive activity, and promotes a sense of calm and well-being.
Furthermore, the vagus nerve is involved in the body’s stress response. When we experience stress or danger, the vagus nerve can trigger the release of stress hormones, such as cortisol, to prepare the body for fight or flight.
Interestingly, recent research has also shown that the vagus nerve may have an impact on mental health. Studies have suggested that stimulating the vagus nerve through techniques like vagus nerve stimulation (VNS) may help alleviate symptoms of depression and anxiety.
In conclusion, the vagus nerve is a remarkable structure with a wide range of functions. Its intricate anatomy and vital role in regulating various bodily processes make it a subject of ongoing research and exploration. Understanding the vagus nerve is not only important for medical professionals but also for anyone interested in the fascinating world of human physiology.
The Vagus Nerve and the Neck
The pathway of the vagus nerve through the neck is of significant importance. Understanding its course and impact on neck functions can provide insight into various disorders that may arise.
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It originates in the medulla oblongata, the lower part of the brainstem, and extends down through the neck, chest, and abdomen, innervating various organs along the way.
As the vagus nerve descends through the neck, it branches off to innervate the muscles responsible for swallowing and speaking. These muscles include the muscles of the pharynx, larynx, and esophagus. The vagus nerve’s intricate network of branches ensures the coordinated movement of these muscles, allowing for efficient swallowing and clear speech.
In addition to its role in controlling swallowing and speaking, the vagus nerve also plays a crucial role in regulating the tone of the vocal cords. It provides the necessary innervation to the muscles that control the tension and position of the vocal cords, allowing for the production of different pitches and tones during speech.
Furthermore, the vagus nerve has a significant impact on blood flow to the neck. It helps regulate the constriction and dilation of blood vessels in the neck, ensuring adequate blood supply to the various structures in the region. This regulation is essential for maintaining optimal oxygen and nutrient delivery to the neck tissues.
Moreover, the vagus nerve is involved in certain reflexes that occur in the neck. For example, it plays a role in the gag reflex, which is a protective mechanism that helps prevent choking. When the back of the throat is stimulated, the vagus nerve sends signals to the brain, triggering a reflexive contraction of the muscles in the throat to expel any potential obstructions.
Overall, the vagus nerve’s influence on neck functions is extensive. Its intricate pathway through the neck and its connections to various muscles and structures ensure the proper functioning of swallowing, speaking, vocalization, blood flow regulation, and reflexes. Any disruption or dysfunction of the vagus nerve in the neck can lead to a range of disorders, including difficulty swallowing, hoarseness, and impaired blood flow to the neck tissues.
Disorders Related to the Vagus Nerve
When the vagus nerve is affected by injury, compression, or dysfunction, various disorders may arise. Awareness of common symptoms and conditions related to the vagus nerve can aid in seeking timely medical attention.
The vagus nerve, also known as the tenth cranial nerve, is one of the longest and most important nerves in the body. It is responsible for regulating many vital functions, including heart rate, digestion, and speech. When this nerve is disrupted, it can lead to a range of disorders that can significantly impact a person’s quality of life.
Symptoms of Vagus Nerve Disorders
Disorders involving the vagus nerve may present with a wide range of symptoms, including difficulty swallowing, hoarseness, voice changes, chronic cough, heart palpitations, dizziness, and gastrointestinal disturbances. These symptoms can vary in severity and may occur individually or in combination.
Difficulty swallowing, also known as dysphagia, can be a result of vagus nerve dysfunction. This can make it challenging to eat and drink, leading to weight loss and malnutrition if left untreated. Hoarseness and voice changes may occur due to vocal cord paralysis, which can affect the ability to speak clearly and communicate effectively.
Chronic cough is another common symptom associated with vagus nerve disorders. It can be persistent and bothersome, often disrupting daily activities and causing discomfort. Heart palpitations, characterized by a rapid or irregular heartbeat, may also occur when the vagus nerve is affected. These palpitations can be alarming and may require medical attention to determine the underlying cause.
In addition to these symptoms, dizziness and gastrointestinal disturbances, such as nausea, bloating, and constipation, can also be present in vagus nerve disorders. These symptoms can significantly impact a person’s daily life and may require medical intervention to alleviate discomfort and improve overall well-being.
However, it is important to note that these symptoms can also be associated with other medical conditions, so a thorough evaluation by a healthcare professional is crucial for an accurate diagnosis. They will conduct a comprehensive medical history review, physical examination, and may order additional tests to determine the underlying cause of the symptoms.
Common Vagus Nerve Disorders
Several conditions may affect the vagus nerve, including vagus nerve damage, vocal cord paralysis, gastroesophageal reflux disease (GERD), and certain types of heart conditions. Vagus nerve damage can occur due to trauma, surgery, or underlying medical conditions, leading to a disruption in the nerve’s normal functioning.
Vocal cord paralysis, on the other hand, can result from damage to the nerves that control the vocal cords, including the vagus nerve. This can cause difficulty speaking, breathlessness, and a weak or hoarse voice. Treatment for vocal cord paralysis may include voice therapy, surgical intervention, or both, depending on the severity of the condition.
GERD, a chronic condition characterized by the reflux of stomach acid into the esophagus, can also be associated with vagus nerve dysfunction. The vagus nerve plays a crucial role in regulating the movement of food through the digestive system, and when it is affected, it can lead to problems such as acid reflux, heartburn, and difficulty swallowing.
Certain types of heart conditions, such as arrhythmias and bradycardia, can also be related to vagus nerve dysfunction. The vagus nerve helps regulate heart rate, and when it is disrupted, it can lead to abnormal heart rhythms and a slower heart rate. These conditions may require medical intervention, such as medication or pacemaker implantation, to manage the symptoms and prevent complications.
In conclusion, disorders related to the vagus nerve can manifest in various ways, affecting different aspects of a person’s health. Recognizing the symptoms and seeking timely medical attention is crucial for an accurate diagnosis and appropriate management of these conditions. Healthcare professionals play a vital role in evaluating and treating vagus nerve disorders, helping individuals regain their quality of life and overall well-being.
Diagnosing Vagus Nerve Disorders
Diagnosing vagus nerve disorders involves a combination of medical history, physical examination, and diagnostic tests. It is important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment options.
When it comes to diagnosing vagus nerve disorders, healthcare professionals employ a comprehensive approach that includes a thorough review of the patient’s medical history and a meticulous physical examination. During the medical history assessment, the healthcare professional will inquire about the patient’s symptoms, their duration, and any factors that may aggravate or alleviate them. Additionally, they will ask about the patient’s overall health, medical conditions, and any medications they may be taking.
The physical examination is a crucial step in the diagnostic process. The healthcare professional will conduct a detailed assessment, paying close attention to the patient’s ability to swallow and speak. They will also check for any signs of nerve dysfunction, such as muscle weakness, impaired reflexes, or abnormal sensations. By carefully examining the patient, healthcare professionals can gather valuable information that aids in the diagnosis of vagus nerve disorders.
Diagnostic Tests for Vagus Nerve Disorders
To confirm a diagnosis and identify the underlying cause of vagus nerve disorders, various diagnostic tests may be recommended. These tests go beyond the medical history and physical examination, providing more detailed insights into the condition.
One common diagnostic test used for vagus nerve disorders is imaging studies. X-rays or magnetic resonance imaging (MRI) can help visualize the structures surrounding the vagus nerve, such as the throat, neck, and chest. These images can reveal any abnormalities or obstructions that may be affecting the nerve’s function.
In addition to imaging studies, specialized tests may be conducted to assess the specific functions of the vagus nerve. Laryngoscopy, for example, involves the insertion of a thin, flexible tube with a camera into the throat to examine the vocal cords and larynx. This test can help identify any issues with vocal cord movement or function.
Esophageal manometry is another specialized test that measures the pressure and movement of the esophagus. This test can provide valuable information about the function of the vagus nerve in relation to swallowing and digestion.
By combining the information gathered from the medical history, physical examination, and diagnostic tests, healthcare professionals can make an accurate diagnosis of vagus nerve disorders. This diagnosis is crucial for developing an appropriate treatment plan tailored to the individual patient’s needs.
Treatment Options for Vagus Nerve Disorders
Treatment options for vagus nerve disorders depend on the specific condition and its underlying cause. Once again, it is crucial to consult with a healthcare professional for individualized treatment recommendations.
The vagus nerve, also known as the tenth cranial nerve, plays a vital role in regulating various bodily functions, including heart rate, digestion, and breathing. When this nerve is affected by a disorder, it can lead to a wide range of symptoms and complications.
Medications are often prescribed to address symptoms associated with vagus nerve disorders. For example, in cases of gastroesophageal reflux disease (GERD), medications can help manage heartburn and reflux symptoms. Additionally, certain medications can be used to relieve pain caused by nerve inflammation, providing much-needed relief to individuals suffering from conditions such as trigeminal neuralgia.
Medications for Vagus Nerve Disorders
In some cases, medications may be prescribed to address symptoms associated with vagus nerve disorders. For example, medications can help manage heartburn and reflux symptoms in cases of GERD or relieve pain caused by nerve inflammation.
There are various types of medications that can be used to target specific symptoms. Proton pump inhibitors (PPIs) are commonly prescribed to reduce stomach acid production and alleviate symptoms of GERD. Antacids, on the other hand, neutralize stomach acid and provide temporary relief from heartburn. For individuals experiencing nerve pain, medications such as anticonvulsants or tricyclic antidepressants may be prescribed to help manage the discomfort.
It is important to note that medication alone may not always be sufficient to treat vagus nerve disorders. In some cases, surgical interventions may be necessary to address the underlying cause or provide long-term relief.
Surgical Treatments for Vagus Nerve Disorders
In certain situations, surgical interventions may be considered to address vagus nerve disorders. These procedures can range from vocal cord augmentation or repositioning for vocal cord paralysis to surgical interventions addressing nerve compression.
Vocal cord paralysis, a condition that can result from damage to the vagus nerve, can significantly impact an individual’s ability to speak and breathe properly. Surgical options, such as vocal cord augmentation or repositioning, aim to restore vocal cord function and improve overall quality of life.
Nerve compression, another common issue associated with vagus nerve disorders, can cause pain and discomfort. Surgical interventions, such as decompression surgeries, can help alleviate the pressure on the nerve, providing relief from symptoms and improving nerve function.
It is important to consult with a qualified healthcare professional to determine the most appropriate treatment option for your specific condition. They will consider factors such as the severity of your symptoms, underlying cause, and overall health before recommending a course of action.
The Future of Vagus Nerve Research
Research and advancements in vagus nerve-related treatments continue to evolve, offering potential for improved outcomes and novel therapeutic approaches.
The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body. It extends from the brainstem down into the abdomen, innervating various organs along the way. This nerve plays a crucial role in regulating many bodily functions, including heart rate, digestion, and inflammation.
Emerging Treatments for Vagus Nerve Disorders
Scientists and medical professionals are exploring new treatment modalities for vagus nerve disorders. These include vagus nerve stimulation techniques, which involve the use of electrical impulses to modulate nerve activity and potentially alleviate symptoms in certain individuals.
Vagus nerve stimulation has shown promise in the management of epilepsy, a neurological disorder characterized by recurrent seizures. By delivering electrical pulses to the vagus nerve, this treatment can help reduce the frequency and intensity of seizures in some patients. Additionally, research suggests that vagus nerve stimulation may have potential applications in the treatment of depression and inflammatory disorders, such as rheumatoid arthritis and Crohn’s disease.
The Potential of Vagus Nerve Stimulation
Vagus nerve stimulation is a promising area of research, with potential applications in the treatment of various conditions, including epilepsy, depression, and inflammatory disorders. However, further studies are needed to determine its efficacy and safety in different patient populations.
Recent advancements in technology have led to the development of innovative devices specifically designed for vagus nerve stimulation. These devices are implanted under the skin, usually in the chest area, and are connected to the vagus nerve via a wire. They can be programmed to deliver electrical impulses at specific intervals, tailored to each patient’s needs.
While vagus nerve stimulation holds great promise, it is important to note that it may not be suitable for everyone. Like any medical intervention, it has potential risks and side effects. Therefore, a thorough evaluation by a healthcare professional is essential to determine the appropriateness of this treatment option for each individual.
As our understanding of the vagus nerve and its role in the neck continues to deepen, it opens up new possibilities for the diagnosis, management, and treatment of related disorders. However, it is crucial to remember that each person’s situation is unique, and consulting with a healthcare professional is essential for individualized care. By working together with medical experts, patients can receive the best possible guidance and support for their specific needs.
If you’re fascinated by the intricate workings of the vagus nerve as highlighted in this guide and wish to delve deeper into its wonders, the “My Vagus Nerve & Me Book” is your next must-read. This comprehensive eBook will expand your knowledge on the vagus nerve’s extensive role in your health, from heart rate regulation to supporting liver detoxification. Discover natural and artificial methods to stimulate this vital nerve for improved well-being. Embrace the opportunity to learn how to harness the power of your vagus nerve for a healthier life. Get My Vagus Nerve & Me eBook today and embark on a journey to optimal health.