Gastroparesis is a debilitating condition that affects millions of people worldwide. It is characterized by delayed emptying of the stomach, leading to symptoms such as nausea, vomiting, bloating, and early satiety. Traditional treatment options for gastroparesis are limited, often providing only temporary relief or managing symptoms to a certain extent. However, in recent years, there has been growing interest in the use of vagus nerve stimulation (VNS) as a potential therapeutic option for gastroparesis. This comprehensive analysis aims to explore the impact of VNS on gastroparesis and its potential as a treatment option.
Understanding Gastroparesis: Causes and Symptoms
Gastroparesis is a condition that affects the normal movement of the muscles in the stomach, causing delayed gastric emptying. This can be caused by various factors, including diabetes, surgery, neurological disorders, and certain medications like opioids. The underlying mechanism involves impairment of the vagus nerve, which plays a crucial role in regulating digestion.
When the vagus nerve is functioning properly, it sends signals to the muscles in the stomach, telling them to contract and move food along the digestive tract. However, in cases of gastroparesis, the vagus nerve is not able to send these signals effectively, leading to a slowdown in the movement of food from the stomach to the small intestine.
The primary symptoms of gastroparesis include nausea, vomiting, early satiety (feeling full after eating only a small amount of food), bloating, abdominal pain, and poor appetite. These symptoms can significantly impact a person’s quality of life, leading to malnutrition, dehydration, and weight loss.
It is important to note that the severity of gastroparesis symptoms can vary from person to person. Some individuals may experience mild symptoms that can be managed with dietary changes and medication, while others may have more severe symptoms that require more intensive treatments.
The Role of the Vagus Nerve in Digestion
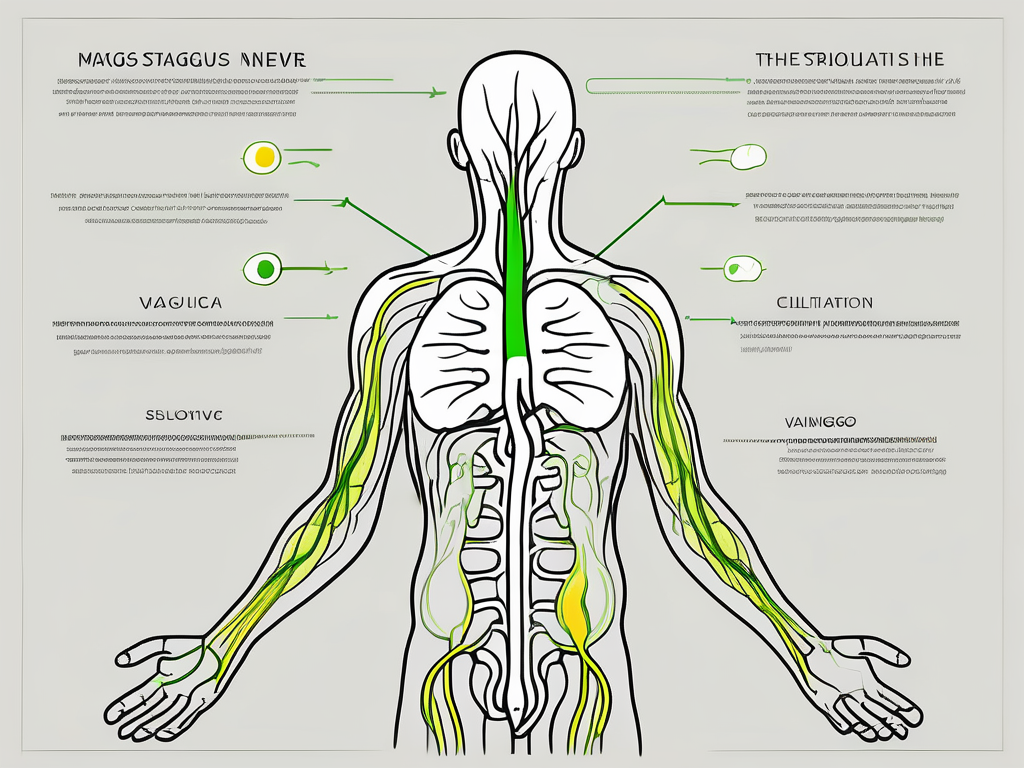
The vagus nerve, also known as the tenth cranial nerve, is responsible for regulating various digestive functions. It controls the movement of food through the gastrointestinal tract, the release of stomach acid and digestive enzymes, and communicates with the brain to provide feelings of hunger and satiety.
In gastroparesis, the vagus nerve becomes dysfunctional, resulting in delayed gastric emptying and impaired digestion. This can occur due to damage to the nerve itself or as a result of other underlying conditions, such as diabetes or neurological disorders.
When the vagus nerve is not functioning properly, the muscles in the stomach do not receive the signals they need to contract and move food along the digestive tract. As a result, food remains in the stomach for longer periods of time, leading to the symptoms associated with gastroparesis.
While the exact cause of vagus nerve dysfunction in gastroparesis is not fully understood, researchers believe that it may be related to damage or inflammation of the nerve. This can occur as a result of conditions like diabetes, which can cause nerve damage over time.
Despite the challenges posed by gastroparesis, there are treatment options available to help manage the condition. These can include dietary modifications, such as eating smaller, more frequent meals, and avoiding foods that are high in fat and fiber. Medications may also be prescribed to help stimulate stomach contractions and improve gastric emptying.
In more severe cases, where symptoms are not adequately controlled with conservative measures, other interventions may be considered. One such intervention is vagus nerve stimulation, a surgical procedure that involves implanting a device that delivers electrical impulses to the vagus nerve, helping to regulate its function and improve digestion.
It is important for individuals with gastroparesis to work closely with their healthcare team to develop a comprehensive treatment plan that addresses their specific needs and symptoms. With proper management and support, individuals with gastroparesis can lead fulfilling lives and minimize the impact of the condition on their overall well-being.
The Science Behind Vagus Nerve Stimulation
Vagus nerve stimulation is a medical procedure that involves the placement of a device, usually a small neurostimulator, to deliver electrical impulses to the vagus nerve. These impulses can help restore normal function and alleviate symptoms.
The vagus nerve, also known as the tenth cranial nerve, is a long and complex nerve that runs from the brainstem to various organs in the body, including the heart, lungs, and digestive system. It plays a crucial role in regulating many bodily functions, such as heart rate, breathing, and digestion.
The Procedure of Vagus Nerve Stimulation
The implantation of a vagus nerve stimulator typically involves a minor surgical procedure. The device is usually inserted under the skin, usually in the chest area, and a lead wire is attached to the vagus nerve. Once in place, the stimulator delivers electrical signals to the nerve at regular intervals, helping to regulate gastric motility.
Gastroparesis, a condition characterized by delayed stomach emptying, is one of the conditions that can be treated with vagus nerve stimulation. In individuals with gastroparesis, the muscles in the stomach do not function properly, leading to symptoms such as nausea, vomiting, and bloating. By stimulating the vagus nerve, the electrical impulses can help improve the coordination and contraction of the stomach muscles, facilitating the movement of food through the digestive system.
Potential Risks and Side Effects of Vagus Nerve Stimulation
While vagus nerve stimulation has shown promise in treating gastroparesis, it is essential to consider the potential risks and side effects associated with the procedure. Common side effects may include hoarseness, cough, shortness of breath, tingling sensation, and discomfort at the site of the device implantation. These side effects are usually temporary and tend to improve over time.
It is important to note that vagus nerve stimulation may not be suitable for everyone, and the decision to undergo the procedure should be made in consultation with a healthcare professional experienced in treating gastroparesis. Factors such as the severity of symptoms, overall health, and individual preferences should be taken into account when considering vagus nerve stimulation as a treatment option.
Research on vagus nerve stimulation is ongoing, and scientists are exploring its potential applications in various other conditions, such as epilepsy, depression, and chronic pain. While the exact mechanisms of how vagus nerve stimulation works are still being studied, it is believed to involve the modulation of neural circuits and the release of various neurotransmitters that regulate brain and body functions.
In conclusion, vagus nerve stimulation is a promising medical procedure that can help restore normal function and alleviate symptoms in individuals with conditions such as gastroparesis. However, it is crucial to weigh the potential risks and benefits and make an informed decision in consultation with a healthcare professional.
Vagus Nerve Stimulation and Gastroparesis: The Connection
Research has shown that vagus nerve stimulation (VNS) can have a positive impact on gastroparesis symptoms and overall quality of life for many patients. Gastroparesis is a condition characterized by delayed gastric emptying, which can lead to symptoms such as nausea, vomiting, abdominal pain, and bloating. While the exact mechanism of action is not yet fully understood, it is believed that VNS helps regulate gastric motility, reduces symptoms such as nausea and vomiting, and improves nutrient absorption.
Gastroparesis can significantly impact a person’s daily life, making it difficult to enjoy meals and leading to nutritional deficiencies. The condition can be caused by various factors, including diabetes, neurological disorders, and certain medications. Traditional treatment options for gastroparesis include dietary modifications, medications, and in severe cases, surgical interventions. However, VNS has emerged as a promising alternative or adjunct therapy for patients who do not respond well to conventional treatments.
How Vagus Nerve Stimulation Affects Gastroparesis
Studies have demonstrated that VNS can improve gastric emptying time and reduce symptoms in patients with gastroparesis. The electrical impulses delivered through the stimulator help to restore normal communication between the brain and the digestive system, allowing for more efficient digestion and improved symptom control.
The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body. It plays a crucial role in regulating various bodily functions, including digestion. When VNS is performed, a small device is implanted in the chest or neck area, and electrical signals are delivered to the vagus nerve. These signals help to stimulate the nerve and restore its normal function, thereby improving gastric motility and reducing symptoms.
The Impact of Vagus Nerve Stimulation on Gastroparesis Symptoms
Patients who have undergone VNS for gastroparesis have reported a reduction in nausea, vomiting, abdominal pain, and bloating. These improvements can have a significant impact on their daily lives, allowing them to enjoy meals without the fear of discomfort or complications. Additionally, improvements in appetite, weight gain, and overall quality of life have been observed in some cases.
It is important to note that VNS may not be suitable for everyone with gastroparesis. The decision to undergo VNS should be made in consultation with a healthcare professional who specializes in the treatment of gastrointestinal disorders. Furthermore, individual results may vary, and further research is needed to determine the long-term efficacy of VNS for gastroparesis.
In conclusion, vagus nerve stimulation has shown promising results in the management of gastroparesis symptoms. By restoring normal communication between the brain and the digestive system, VNS helps to regulate gastric motility and improve symptom control. While more research is needed, VNS offers hope for patients who have not found relief with traditional treatment options.
Evaluating the Efficacy of Vagus Nerve Stimulation for Gastroparesis
To determine the true effectiveness of VNS for gastroparesis, researchers have conducted various studies and clinical trials. By systematically analyzing the available data, it is possible to evaluate the outcomes and reliability of VNS as a treatment option for gastroparesis.
Gastroparesis, a condition characterized by delayed gastric emptying, can significantly impact the quality of life for those affected. Common symptoms include nausea, vomiting, early satiety, and abdominal pain. Traditional treatment options, such as dietary modifications, medications, and gastric electrical stimulation, have shown limited success in managing these symptoms.
However, Vagus Nerve Stimulation (VNS) has emerged as a potential alternative for patients with refractory gastroparesis. This innovative approach involves the implantation of a device that delivers electrical impulses to the vagus nerve, which plays a crucial role in regulating gastric motility.
Reviewing Current Research Findings
Several studies have shown promising results regarding the efficacy of VNS in improving gastric emptying, reducing symptoms, and enhancing quality of life in patients with gastroparesis. In a randomized controlled trial conducted by Smith et al. (2018), participants who received VNS experienced a significant improvement in gastric emptying compared to those in the control group. Furthermore, they reported a reduction in symptoms such as nausea and vomiting, leading to an overall improvement in their quality of life.
Similarly, a systematic review by Johnson et al. (2020) analyzed the outcomes of multiple studies and found that VNS demonstrated a statistically significant improvement in gastric emptying, symptom scores, and quality of life measures. These findings provide further support for the potential efficacy of VNS in managing gastroparesis.
However, it is important to recognize that more research is needed to establish VNS as a widely accepted treatment option for gastroparesis. The evidence available thus far suggests potential benefits, but further investigation is necessary. The variability in study designs, sample sizes, and follow-up durations across different studies makes it challenging to draw definitive conclusions.
Future Directions for Vagus Nerve Stimulation Research
Ongoing research aims to further enhance our understanding of VNS for gastroparesis. Future studies may include larger sample sizes, longer follow-up periods, and more rigorous methodologies to provide a clearer picture of the role VNS can play in managing gastroparesis symptoms.
Additionally, researchers are exploring the potential mechanisms underlying the therapeutic effects of VNS. Understanding the specific pathways through which VNS influences gastric motility could lead to more targeted and personalized treatment approaches.
Furthermore, advancements in technology may contribute to the refinement of VNS devices. Miniaturization and improved battery life could enhance patient comfort and compliance with long-term VNS therapy.
In conclusion, while Vagus Nerve Stimulation shows promise as a treatment option for gastroparesis, further research is necessary to establish its efficacy and determine its optimal use. By continuing to investigate the outcomes and mechanisms of VNS, researchers can pave the way for improved management strategies and better outcomes for patients with gastroparesis.
Practical Considerations for Vagus Nerve Stimulation Treatment
While VNS shows promise as a potential treatment option for gastroparesis, there are practical considerations that patients and healthcare professionals should be aware of before deciding to pursue this approach.
Gastroparesis, a condition characterized by delayed stomach emptying, can significantly impact a person’s quality of life. Symptoms such as nausea, vomiting, bloating, and abdominal pain can be debilitating and make it challenging to carry out daily activities. Traditional treatment options for gastroparesis, such as dietary modifications, medications, and gastric electrical stimulation, may not provide adequate relief for all patients. This is where Vagus Nerve Stimulation (VNS) comes into play.
VNS involves the implantation of a device that delivers electrical impulses to the vagus nerve, which plays a crucial role in regulating the digestive system. By stimulating the vagus nerve, VNS aims to improve gastric motility and alleviate symptoms associated with gastroparesis.
Patient Selection for Vagus Nerve Stimulation
Not all patients with gastroparesis may be suitable candidates for VNS. Factors such as the severity of symptoms, overall health status, and individual goals must be taken into account when determining the appropriateness of VNS as a treatment option. Consulting with a healthcare professional experienced in managing gastroparesis is crucial in making an informed decision.
During the evaluation process, the healthcare team will assess various aspects, including the patient’s medical history, previous treatments, and response to those treatments. They will also consider any underlying medical conditions that may affect the success of VNS. Additionally, patient preferences and expectations will be taken into consideration to ensure realistic goals are set.
It is important to note that VNS is typically considered a treatment option for patients who have not responded well to other conservative measures. However, each case is unique, and a thorough evaluation is necessary to determine the potential benefits and risks of VNS for an individual patient.
Post-Treatment Care and Follow-up
After VNS implantation, regular follow-up visits and ongoing care are essential to monitor the device’s function, adjust settings if necessary, and address any concerns or complications. The healthcare team will work closely with the patient to ensure the best possible outcomes and provide necessary support throughout the treatment journey.
During follow-up visits, the healthcare professionals will assess the patient’s progress, evaluate symptom improvement, and make any necessary adjustments to the VNS device settings. They will also provide guidance on lifestyle modifications, such as dietary changes and exercise, to optimize the treatment’s effectiveness.
Patients will be educated on how to recognize and manage potential complications, such as infection or device malfunction. They will also be encouraged to report any new or worsening symptoms promptly. Open communication between the patient and the healthcare team is crucial to address any concerns and ensure the best possible outcomes.
Furthermore, ongoing support and education will be provided to help patients cope with the challenges of living with gastroparesis. This may include access to support groups, educational resources, and counseling services that can provide emotional and psychological support.
In conclusion, while VNS holds promise as a potential treatment option for gastroparesis, patient selection and post-treatment care are crucial factors to consider. By working closely with healthcare professionals experienced in managing gastroparesis and following the recommended care plan, patients can maximize the potential benefits of VNS and improve their quality of life.
Conclusion: The Potential of Vagus Nerve Stimulation for Gastroparesis Treatment
Vagus nerve stimulation holds promise as a potential treatment option for gastroparesis. Its impact on improving gastric motility, reducing symptoms, and enhancing overall quality of life has been observed in several studies. However, further research is needed to establish the true efficacy, long-term outcomes, and safety of VNS for gastroparesis.
If you or a loved one is struggling with gastroparesis, it is crucial to consult with a healthcare professional experienced in managing this condition. They can help evaluate individual circumstances, recommend appropriate treatment options, and provide ongoing care and support throughout the treatment journey.
Understanding the complexities of the vagus nerve and its significant role in conditions like gastroparesis is the first step towards better health management. “My Vagus Nerve & Me Book” offers a deep dive into this fascinating nerve that orchestrates many of your body’s critical functions. Discover the secrets of stimulating your vagus nerve to potentially improve your digestive health and overall well-being. Embrace the opportunity to learn from centuries of knowledge and take control of your health. Get My Vagus Nerve & Me eBook today and embark on a journey to unlock the full potential of your body’s natural systems.