Post-concussion syndrome (PCS) is a condition that can occur after a mild traumatic brain injury, such as a concussion. It is characterized by a range of symptoms that persist beyond the initial injury, including headaches, dizziness, fatigue, and difficulty with memory and concentration. While the exact cause of PCS is still not fully understood, recent research has shed light on the potential role of the vagus nerve in this condition.
Understanding the Vagus Nerve
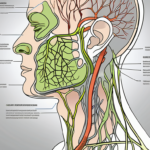
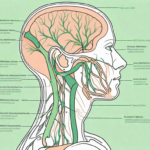
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of all the cranial nerves. It is a major component of the autonomic nervous system, which controls many involuntary body functions, such as heart rate, digestion, and breathing. The vagus nerve has both sensory and motor functions, and it extends from the brainstem to various organs throughout the body.
Anatomy and Function of the Vagus Nerve
The vagus nerve consists of tens of thousands of nerve fibers that originate in the brainstem and branch out to innervate different organs, including the heart, lungs, stomach, and intestines. It plays a crucial role in regulating many bodily functions, such as heart rate, blood pressure, digestion, and immune response. In addition, the vagus nerve is involved in the release of certain neurotransmitters, such as acetylcholine, which has anti-inflammatory effects and helps to promote relaxation.
When it comes to the anatomy of the vagus nerve, it is fascinating to note that it is the only cranial nerve that extends beyond the head and neck region. It travels through the neck, thorax, and abdomen, making connections with various organs along the way. This extensive reach allows the vagus nerve to have a profound impact on the overall functioning of the body.
Furthermore, the vagus nerve is not a single entity but rather a complex network of fibers. These fibers are organized into different branches, each responsible for specific functions. For example, one branch of the vagus nerve controls the heart rate, ensuring that it beats at a steady pace. Another branch regulates digestion, ensuring that food is properly broken down and absorbed by the body. The intricate organization of the vagus nerve highlights its importance in maintaining overall health and well-being.
The Vagus Nerve’s Role in the Autonomic Nervous System
One of the key functions of the vagus nerve is its role in the autonomic nervous system. This system has two branches: the sympathetic nervous system and the parasympathetic nervous system. The sympathetic nervous system is responsible for the “fight-or-flight” response, while the parasympathetic nervous system promotes the “rest-and-digest” response.
The vagus nerve is part of the parasympathetic branch and helps to counterbalance the effects of the sympathetic nervous system. It helps regulate heart rate, promote digestion, and maintain a state of relaxation. When the vagus nerve is functioning properly, it helps the body return to a state of balance after a stressful event or injury.
It is fascinating to consider the intricate dance between the sympathetic and parasympathetic branches of the autonomic nervous system. The vagus nerve, with its extensive reach and influence, plays a crucial role in maintaining this delicate balance. Without the vagus nerve’s counterbalancing effects, the body would struggle to return to a state of equilibrium, leading to potential health issues.
Moreover, recent research has shed light on the connection between the vagus nerve and mental health. Studies have shown that stimulating the vagus nerve can have a positive impact on conditions such as depression and anxiety. This further emphasizes the importance of understanding and nurturing the health of the vagus nerve.
In conclusion, the vagus nerve is a remarkable structure that extends throughout the body, connecting various organs and playing a vital role in regulating numerous bodily functions. Its involvement in the autonomic nervous system ensures that the body can respond appropriately to different situations, maintaining a delicate balance between the sympathetic and parasympathetic branches. Understanding the vagus nerve and its functions is essential for appreciating the complexity and interconnectedness of the human body.
Post-Concussion Syndrome: An Overview
Post-concussion syndrome refers to a collection of symptoms that persist for weeks, months, or even years after a concussion or mild traumatic brain injury. While most people recover fully within a few weeks, some individuals experience ongoing symptoms that can significantly impact their daily lives.
When it comes to post-concussion syndrome, there is still much to be discovered and understood. Researchers are constantly working to unravel the complexities of this condition, aiming to provide better treatment options and improve the overall quality of life for those affected.
Symptoms and Diagnosis of Post-Concussion Syndrome
The symptoms of post-concussion syndrome can vary from person to person, but some common symptoms include persistent headaches, dizziness, fatigue, difficulty with memory and concentration, sleep disturbances, and mood changes. These symptoms can be similar to those experienced immediately following a concussion but tend to persist for a longer period of time.
It is important to note that the severity and duration of symptoms can vary greatly among individuals. While some may experience mild symptoms that gradually fade away, others may face more debilitating and long-lasting effects. The impact of post-concussion syndrome on an individual’s life can be significant, affecting their ability to work, engage in social activities, and maintain relationships.
Diagnosing post-concussion syndrome is often based on a person’s medical history and the persistence of symptoms for several weeks after the initial injury. It is important to consult with a healthcare professional for an accurate diagnosis, as other conditions with similar symptoms need to be ruled out.
Medical professionals may use a combination of physical and neurological examinations, imaging tests, and cognitive assessments to evaluate the extent of the injury and determine the presence of post-concussion syndrome. This comprehensive approach helps ensure an accurate diagnosis and appropriate treatment plan.
Long-Term Effects of Post-Concussion Syndrome
While most people with post-concussion syndrome eventually recover, some individuals may experience long-term impacts on their cognitive abilities and overall quality of life. The exact mechanisms behind these long-term effects are still not fully understood, but researchers continue to investigate the underlying factors.
Studies have shown that individuals with a history of concussion are at a higher risk for developing neurodegenerative disorders later in life, such as Alzheimer’s disease and Parkinson’s disease. This association raises important questions about the potential long-term consequences of post-concussion syndrome and the need for proactive management and support.
Understanding the underlying mechanisms that contribute to the persistence of post-concussion symptoms is essential for developing effective treatment strategies and mitigating long-term effects. Researchers are exploring various factors, including inflammation, neurotransmitter imbalances, and structural changes in the brain, to gain a deeper understanding of the condition.
Furthermore, ongoing research aims to identify potential risk factors that may predispose individuals to developing post-concussion syndrome and its long-term effects. This knowledge can help healthcare professionals tailor treatment plans and provide necessary support to those at higher risk.
Overall, post-concussion syndrome is a complex condition that requires further investigation and understanding. By continuing to explore its underlying mechanisms and long-term effects, researchers hope to improve the lives of individuals affected by this condition and develop more targeted and effective treatment approaches.
The Connection between the Vagus Nerve and Post-Concussion Syndrome
The vagus nerve has gained attention in recent years as a potential key player in the development and persistence of post-concussion syndrome. Research suggests that dysfunction of the vagus nerve may contribute to the ongoing symptoms experienced by individuals with PCS.
How the Vagus Nerve Influences Brain Health
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It originates in the brainstem and extends down to various organs in the body, including the heart, lungs, and digestive system. While traditionally known for its role in regulating the heart rate and digestion, the vagus nerve has also been found to have a significant impact on brain health.
One of the key functions of the vagus nerve is its neuroprotective role. It helps to regulate and maintain the health of brain cells by promoting the release of neurotrophic factors, which are proteins that support the growth and survival of neurons. These factors play a crucial role in neuroplasticity, the brain’s ability to adapt and reorganize itself in response to injury or changes in the environment.
In addition to its neuroprotective role, the vagus nerve is also involved in modulating the inflammatory response in the brain. It helps regulate the release of pro-inflammatory cytokines, which are signaling molecules involved in the immune response, and promotes the production of anti-inflammatory substances. This delicate balance between pro-inflammatory and anti-inflammatory factors is crucial for maintaining brain health and preventing excessive inflammation.
Dysregulation of the vagus nerve’s inflammatory response may contribute to the neuroinflammation observed in individuals with post-concussion syndrome. When the vagus nerve is not functioning optimally, there may be an imbalance in the release of pro-inflammatory and anti-inflammatory factors, leading to chronic inflammation in the brain. This chronic inflammation can contribute to the ongoing symptoms experienced by individuals with PCS, such as headaches, cognitive difficulties, and mood disturbances.
Vagus Nerve Dysfunction in Post-Concussion Syndrome
Studies have shown that individuals with post-concussion syndrome may have altered vagal tone, which refers to the balance between the sympathetic and parasympathetic branches of the autonomic nervous system. The sympathetic branch is responsible for the body’s “fight or flight” response, while the parasympathetic branch is responsible for the body’s “rest and digest” response.
Reduced vagal tone has been associated with increased inflammation, cognitive deficits, and mood disturbances, all of which are commonly observed in PCS. When the vagus nerve is not functioning properly, it can lead to an overactivation of the sympathetic branch and a decreased activation of the parasympathetic branch. This imbalance can result in a heightened inflammatory response, impairments in cognitive function, and mood dysregulation.
Furthermore, vagus nerve dysfunction can also affect other aspects of brain health, such as sleep and stress regulation. The vagus nerve plays a crucial role in the regulation of sleep-wake cycles and helps promote restful sleep. When the vagus nerve is not functioning optimally, it can disrupt sleep patterns and contribute to sleep disturbances commonly experienced by individuals with PCS.
In addition, the vagus nerve is involved in the regulation of the body’s stress response. It helps to dampen the stress response by activating the parasympathetic branch and promoting relaxation. However, in individuals with vagus nerve dysfunction, this regulation may be impaired, leading to an exaggerated stress response and increased susceptibility to stress-related symptoms.
Overall, the connection between the vagus nerve and post-concussion syndrome is a complex and multifaceted one. Dysfunction of the vagus nerve can contribute to the ongoing symptoms experienced by individuals with PCS, including neuroinflammation, cognitive deficits, mood disturbances, sleep disturbances, and stress-related symptoms. Understanding and addressing vagus nerve dysfunction may hold promise for the development of novel treatment approaches for post-concussion syndrome.
Potential Treatments Targeting the Vagus Nerve
Targeting the vagus nerve shows promise as a potential treatment approach for individuals with post-concussion syndrome. However, it is important to note that more research is needed to establish the efficacy and safety of these interventions. Consulting with a healthcare professional is crucial before considering any specific treatment.
Post-concussion syndrome is a complex condition that can manifest with a wide range of symptoms, including headaches, dizziness, cognitive difficulties, and mood disturbances. As researchers continue to explore new treatment options, targeting the vagus nerve has emerged as a potential avenue for intervention.
Vagus Nerve Stimulation Therapy
Vagus nerve stimulation (VNS) therapy involves the implantation of a small device that delivers electrical impulses to the vagus nerve. This therapy is approved for the treatment of epilepsy and depression and has shown promise in improving symptoms of various neurological disorders.
By stimulating the vagus nerve, VNS therapy aims to modulate the activity of the autonomic nervous system, which plays a crucial role in regulating bodily functions. This modulation can have a positive impact on various physiological processes, including inflammation, cognition, and mood.
While VNS therapy has been extensively studied in other neurological conditions, its potential benefits for individuals with post-concussion syndrome are still being explored. Preliminary research suggests that VNS therapy may help alleviate symptoms such as headaches, cognitive difficulties, and mood disturbances. However, further studies are needed to establish its efficacy specifically for post-concussion syndrome.
Non-Invasive Approaches to Vagus Nerve Stimulation
In addition to invasive VNS therapy, there are also non-invasive approaches to vagus nerve stimulation that are being explored. These approaches offer the potential for a less invasive and more accessible treatment option.
One such approach is transcutaneous vagus nerve stimulation (tVNS), which involves the application of electrical impulses to the skin overlying the vagus nerve. This can be achieved using specialized devices that deliver controlled electrical stimulation.
tVNS has shown promise in reducing inflammation, improving cognition, and alleviating symptoms in individuals with various neurological conditions. By targeting the vagus nerve, tVNS aims to modulate the activity of the autonomic nervous system, similar to invasive VNS therapy. However, unlike invasive VNS therapy, tVNS does not require surgical implantation and can be administered in a non-invasive manner.
Research on tVNS for post-concussion syndrome is still in its early stages. Preliminary studies have reported positive outcomes, including improvements in cognitive function and reduction in symptoms such as headaches and mood disturbances. However, more research is needed to establish the effectiveness of tVNS specifically for post-concussion syndrome.
It is important to note that while targeting the vagus nerve shows promise as a potential treatment approach, it is not a one-size-fits-all solution. Each individual’s condition is unique, and consulting with a healthcare professional is crucial before considering any specific treatment. A healthcare professional can provide personalized guidance based on an individual’s medical history, symptoms, and overall health.
Future Research Directions
While the role of the vagus nerve in post-concussion syndrome is an area of ongoing research, there are still many unanswered questions. Further investigation is needed to elucidate the specific mechanisms by which the vagus nerve impacts PCS and to identify optimal treatment strategies.
Unanswered Questions in Vagus Nerve and Post-Concussion Research
Some of the unanswered questions surrounding the vagus nerve’s involvement in post-concussion syndrome include: How does vagal dysfunction contribute to the persistence of symptoms? What specific inflammatory pathways are affected? Can targeting the vagus nerve provide long-term benefits for individuals with PCS?
One possible explanation for the persistence of symptoms in post-concussion syndrome is the disruption of the autonomic nervous system, which includes the vagus nerve. The vagus nerve plays a crucial role in regulating various bodily functions, including heart rate, digestion, and inflammation. Dysfunction of the vagus nerve may lead to an imbalance in these functions, contributing to the ongoing symptoms experienced by individuals with PCS.
Furthermore, the specific inflammatory pathways affected by vagal dysfunction in PCS remain unclear. Inflammation is a key component of the body’s response to injury, but excessive or prolonged inflammation can have detrimental effects. Understanding how the vagus nerve modulates inflammation in the context of post-concussion syndrome could provide valuable insights into potential therapeutic targets.
Another intriguing question is whether targeting the vagus nerve can provide long-term benefits for individuals with PCS. The vagus nerve has been a target for various therapeutic interventions, such as vagus nerve stimulation, which involves the delivery of electrical impulses to the nerve. This approach has shown promise in the treatment of epilepsy and depression, but its potential in PCS remains to be explored.
The Potential of Vagus Nerve Treatments in Neurological Disorders
Understanding the role of the vagus nerve in post-concussion syndrome may have broader implications for the treatment of other neurological disorders. It opens up the possibility of developing novel therapies targeting the vagus nerve to improve brain health and mitigate the effects of various conditions.
For instance, disorders such as Alzheimer’s disease and Parkinson’s disease are characterized by neuroinflammation and neurodegeneration. If vagal dysfunction is found to contribute to the progression of these conditions, interventions aimed at modulating the vagus nerve could potentially slow down or even halt the neurodegenerative processes.
Additionally, mental health disorders such as anxiety and post-traumatic stress disorder (PTSD) have been associated with dysregulation of the autonomic nervous system. Given the vagus nerve’s role in regulating stress responses and emotional well-being, therapies targeting the vagus nerve could offer new avenues for the treatment of these conditions.
In conclusion, while there are still many unanswered questions regarding the role of the vagus nerve in post-concussion syndrome, further research in this area holds great promise. By unraveling the mechanisms by which the vagus nerve impacts PCS and exploring its potential as a therapeutic target, we may not only improve the lives of individuals with PCS but also pave the way for novel treatments in a wide range of neurological disorders.
Conclusion
The vagus nerve plays a vital role in regulating various bodily functions and maintaining overall health. Its potential involvement in post-concussion syndrome highlights the complex nature of this condition and provides avenues for further research and treatment development. If you suspect you may be experiencing post-concussion syndrome, it is crucial to consult with a healthcare professional for an accurate diagnosis and appropriate management strategies.
As you’ve learned from this article, the vagus nerve is a cornerstone of your health, intricately involved in everything from your immune response to your mental well-being. If you’re intrigued by the profound impact of the vagus nerve on post-concussion syndrome and want to delve deeper into understanding this remarkable part of your anatomy, the “My Vagus Nerve & Me Book” is an essential resource. Discover how to harness the power of your vagus nerve for optimal health, learn natural and artificial stimulation techniques, and explore its myriad functions. Ready to embark on a journey to better health? Get My Vagus Nerve & Me eBook today and take the first step towards unlocking the secrets of one of the most sophisticated systems in your body.