Headaches are a common ailment that can have a significant impact on our daily lives. Many factors can contribute to the development of headaches, including stress, diet, and hormonal changes. However, one often overlooked aspect is the effect of the vagus nerve on headaches. In this article, we will dive deep into the connection between the vagus nerve and headaches, exploring its anatomy, functions, and potential treatments.
Understanding the Vagus Nerve
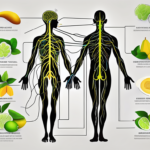
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in the autonomic nervous system. It is the longest cranial nerve and extends from the brainstem down to the abdomen, innervating various organs along the way. The vagus nerve is responsible for regulating many bodily functions, including heart rate, digestion, and even immune responses.
The vagus nerve consists of both sensory and motor fibers. The sensory fibers relay information from the organs to the brain, providing feedback on their status. On the other hand, the motor fibers carry impulses from the brain to the organs, controlling their actions. This bidirectional communication allows the vagus nerve to coordinate and fine-tune the body’s responses.
Some of the key functions of the vagus nerve include:
- Regulating heart rate and blood pressure
- Influencing digestion and nutrient absorption
- Controlling the release of various neurotransmitters
- Modulating inflammation and immune responses
Regulating heart rate and blood pressure is one of the most important functions of the vagus nerve. Through its connections with the heart, the nerve helps maintain a steady heart rate and blood pressure, ensuring proper circulation throughout the body. It achieves this by sending signals to the heart to either speed up or slow down its contractions, depending on the body’s needs.
In addition to its role in cardiovascular regulation, the vagus nerve also influences digestion and nutrient absorption. It sends signals to the digestive organs, such as the stomach and intestines, to stimulate the release of digestive enzymes and promote the movement of food through the gastrointestinal tract. This ensures efficient digestion and absorption of nutrients from the food we consume.
Furthermore, the vagus nerve plays a crucial role in controlling the release of various neurotransmitters in the brain. Neurotransmitters are chemical messengers that transmit signals between nerve cells. By modulating the release of neurotransmitters like serotonin and dopamine, the vagus nerve helps regulate mood, sleep, and overall brain function.
Another fascinating function of the vagus nerve is its ability to modulate inflammation and immune responses. When the body encounters an infection or injury, the vagus nerve can dampen the inflammatory response, preventing excessive inflammation that could be harmful to the body. This mechanism helps maintain a balance between the immune system’s protective response and the potential damage caused by inflammation.
The Vagus Nerve and the Nervous System
Within the nervous system, the vagus nerve interacts with other important structures, such as the brainstem and the trigeminal nerve. The brainstem is responsible for relaying sensory information and controlling basic bodily functions. It serves as a vital connection between the brain and the rest of the body, allowing for the transmission of signals to and from various organs.
The trigeminal nerve, specifically, plays a significant role in transmitting pain signals from the head and face. It works in conjunction with the vagus nerve to ensure the proper perception and processing of pain sensations. This collaboration between the two nerves helps the body respond appropriately to painful stimuli, allowing for protective reflexes and the initiation of pain-relieving mechanisms.
In conclusion, the vagus nerve is a remarkable component of the autonomic nervous system, responsible for regulating numerous bodily functions. Its intricate anatomy and bidirectional communication allow for precise control and coordination of the body’s responses. Understanding the vagus nerve’s functions and its interactions within the nervous system provides valuable insights into the complex mechanisms that govern our physiological well-being.
The Vagus Nerve-Headache Connection
Research suggests that the vagus nerve can influence pain perception, including headaches. How exactly does the vagus nerve impact pain? Let’s explore:
How the Vagus Nerve Influences Pain Perception
One theory is that the vagus nerve acts as a modulator of pain signals, dampening their intensity. By sending inhibitory signals to the central nervous system, the vagus nerve may help regulate pain responses. Dysfunction or imbalances in the vagus nerve could potentially lead to heightened pain sensitivity, including headaches.
But how does the vagus nerve actually accomplish this? The vagus nerve is the longest cranial nerve in the body, extending from the brainstem to various organs in the body, including the heart, lungs, and digestive system. It is responsible for regulating many bodily functions, such as heart rate, digestion, and breathing. In the context of pain perception, the vagus nerve plays a crucial role in the “rest and digest” response, also known as the parasympathetic nervous system. When activated, this system promotes relaxation and reduces stress, which can help alleviate pain.
Furthermore, the vagus nerve is connected to the release of various neurotransmitters, such as serotonin and norepinephrine, which are involved in pain modulation. These neurotransmitters can inhibit the transmission of pain signals, reducing the overall perception of pain. The vagus nerve also interacts with other pain-regulating systems in the body, such as the endogenous opioid system, which produces natural pain-relieving substances.
The Role of the Vagus Nerve in Migraines and Other Headaches
Migraines, in particular, have been closely linked to the vagus nerve. Studies have shown that stimulation of the vagus nerve can relieve migraine symptoms in some individuals. Additionally, researchers have found abnormal electrical activity in the vagus nerve during migraines, further highlighting its involvement in these headaches.
During a migraine attack, the trigeminal nerve, which is responsible for transmitting pain signals from the head and face, becomes overactive. This overactivity can trigger a cascade of events, including the release of inflammatory substances and the dilation of blood vessels in the brain. The vagus nerve, through its extensive connections and regulatory functions, can help modulate this trigeminal overactivity and reduce the severity of migraines.
Furthermore, the vagus nerve is involved in the regulation of other types of headaches, such as tension headaches and cluster headaches. These headaches often have a strong association with stress and anxiety, which can activate the sympathetic nervous system, the counterpart of the parasympathetic nervous system. The vagus nerve, with its role in promoting relaxation and reducing stress, can help counterbalance the sympathetic response and alleviate headache symptoms.
It is important to note that the vagus nerve’s involvement in headaches is complex and multifaceted. While research has provided valuable insights into the connection between the vagus nerve and headaches, there is still much to learn. Further studies are needed to fully understand the mechanisms underlying this relationship and to develop targeted therapies that can effectively modulate vagus nerve activity for headache management.
The Science Behind Vagus Nerve Stimulation
Vagus nerve stimulation (VNS) is a technique that aims to modulate the vagus nerve’s activity to alleviate various conditions, including headaches. The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body and plays a crucial role in regulating many bodily functions, such as heart rate, digestion, and inflammation.
Here’s how VNS works:
VNS involves the use of an implanted device that delivers electrical impulses to the vagus nerve. This device, known as a vagus nerve stimulator, is typically placed under the skin in the chest area and connected to the vagus nerve through a lead wire. The stimulator can be programmed to deliver specific patterns and intensities of electrical impulses.
When the vagus nerve is stimulated, it sends signals to various parts of the brain, including the locus coeruleus, which is involved in pain modulation. By modulating the activity of the vagus nerve, VNS can potentially disrupt excessive pain signals and provide relief for individuals suffering from chronic headaches.
The Process of Vagus Nerve Stimulation
VNS is typically carried out under the supervision of a healthcare professional specializing in neurology or pain management. The process begins with a thorough evaluation of the individual’s medical history and symptoms to determine if VNS is a suitable treatment option.
If VNS is deemed appropriate, a surgical procedure is performed to implant the vagus nerve stimulator. This procedure is usually done under general anesthesia to ensure the comfort and safety of the patient. The surgeon makes a small incision in the chest area and carefully places the stimulator under the skin. The lead wire is then connected to the vagus nerve, allowing for the delivery of electrical impulses.
After the implantation, the healthcare professional will program the vagus nerve stimulator according to the individual’s specific needs. The settings can be adjusted to deliver the optimal level of stimulation for pain relief while minimizing side effects.
Potential Benefits and Risks of Vagus Nerve Stimulation
VNS has shown promise in reducing the frequency and severity of headaches in some individuals. It has been particularly effective for individuals with chronic migraines who have not responded well to other treatment options.
However, it’s important to note that VNS may not be suitable for everyone, and each case should be assessed on an individual basis. The decision to undergo VNS should be made in consultation with a healthcare professional who can evaluate the potential benefits and risks based on the individual’s specific circumstances.
Potential risks and side effects should also be thoroughly discussed with a healthcare professional before considering VNS as a treatment option. Some common side effects of VNS include hoarseness, coughing, shortness of breath, and tingling or prickling sensations in the skin. These side effects are usually temporary and can be managed with adjustments to the stimulation settings.
Overall, VNS offers a promising approach to managing chronic headaches by targeting the underlying neural pathways involved in pain perception. Ongoing research and advancements in technology continue to improve the effectiveness and safety of VNS, providing hope for individuals seeking relief from debilitating headaches.
Non-Invasive Vagus Nerve Stimulation for Headache Relief
Headaches can be debilitating, affecting our daily lives and productivity. While there are various treatment options available, some individuals may seek non-invasive alternatives to avoid surgical procedures. This is where non-invasive vagus nerve stimulation (nVNS) comes into play, offering a more accessible and convenient method for headache relief.
nVNS utilizes external devices that deliver mild electrical signals to the vagus nerve through the skin. By targeting this specific nerve, which is known to play a role in pain regulation, nVNS aims to provide relief from headaches without the need for invasive procedures.
Techniques for Non-Invasive Vagus Nerve Stimulation
nVNS devices often come in the form of handheld devices or wearable patches that can be applied to the neck or other relevant areas. These devices are designed to be user-friendly, allowing individuals to easily incorporate nVNS into their daily routine. By simply placing the device on the skin and activating it, the electrical impulses generated by the device stimulate the vagus nerve, potentially alleviating headache symptoms.
Furthermore, some nVNS devices are equipped with advanced features such as customizable settings and smartphone connectivity. This allows users to personalize their stimulation experience and track their progress over time, providing valuable insights into the effectiveness of the treatment.
Effectiveness of Non-Invasive Vagus Nerve Stimulation
Research studies have investigated the effectiveness of nVNS in reducing the frequency and severity of headaches. While results have been promising, it is important to note that the efficacy of nVNS may vary from person to person. Factors such as the type and cause of headaches, as well as individual physiological differences, can influence the response to nVNS.
Therefore, it is crucial for individuals considering nVNS as a treatment option to consult with a healthcare professional. A healthcare professional can assess the suitability of nVNS for a particular individual, taking into account their medical history and specific needs. Additionally, they can provide guidance on proper usage and potential side effects, ensuring the safe and effective implementation of nVNS for headache relief.
In conclusion, non-invasive vagus nerve stimulation offers a promising alternative for individuals seeking headache relief without invasive procedures. With its user-friendly devices and potential effectiveness, nVNS provides a convenient and accessible option for managing headaches. However, it is important to approach nVNS with guidance from healthcare professionals to ensure its proper usage and maximize its benefits.
Future Research and Potential Treatments
As scientific understanding of the vagus nerve and its connection to headaches continues to evolve, ongoing research is exploring new avenues for potential treatments:
Current Research on the Vagus Nerve and Headaches
Scientists are investigating various aspects of the vagus nerve, including its specific role in different types of headaches, the mechanisms behind its pain-regulating effects, and potential therapeutic targets. These ongoing studies hold promise for improving our understanding and treatment options for headaches.
One area of current research focuses on the vagus nerve’s involvement in migraines. Researchers are studying the relationship between the vagus nerve and the trigeminal nerve, which is known to play a significant role in migraines. By understanding how these two nerves interact, scientists hope to develop more targeted treatments that can provide relief specifically for migraine sufferers.
Another line of research is exploring the potential link between the vagus nerve and tension headaches. Tension headaches are the most common type of headache, characterized by a dull, aching pain and muscle tension in the head and neck. By investigating the vagus nerve’s role in pain modulation, researchers aim to uncover new therapeutic strategies for managing tension headaches.
The Future of Vagus Nerve Treatments for Headache Relief
While VNS and nVNS have shown promise in managing headaches, further advancements in technology and research may lead to even more targeted and personalized treatments. From pharmaceutical interventions to neuromodulation techniques, the future of vagus nerve treatments for headache relief looks promising.
One potential future treatment option being explored is the use of vagus nerve stimulation (VNS) implants. These implants deliver electrical impulses to the vagus nerve, helping to regulate its activity and potentially reducing headache frequency and severity. Researchers are currently investigating the long-term effectiveness and safety of VNS implants, as well as refining the implantation procedure to make it more accessible and minimally invasive.
Another area of interest is non-invasive vagus nerve stimulation (nVNS), which involves applying electrical stimulation to the skin overlying the vagus nerve. This approach has shown promise in clinical trials for both acute and preventive treatment of migraines. Ongoing research aims to optimize the parameters of nVNS, such as stimulation intensity and duration, to maximize its effectiveness and minimize side effects.
In addition to electrical stimulation, researchers are also exploring the potential of pharmacological interventions targeting the vagus nerve. By developing drugs that can modulate the activity of the vagus nerve, scientists hope to provide a non-invasive and easily accessible treatment option for headache sufferers.
Furthermore, advancements in neuromodulation techniques, such as transcranial magnetic stimulation (TMS) and transcutaneous electrical nerve stimulation (TENS), may offer alternative approaches to modulating the vagus nerve and providing headache relief. These techniques involve applying magnetic fields or electrical currents to specific areas of the brain or nerves, respectively, to alter their activity and potentially alleviate pain.
In conclusion, the impact of the vagus nerve on headaches is an intriguing area of study. The vagus nerve’s role in pain modulation and its connection to migraines and other headaches have significant implications for both scientific research and potential treatments. If you suffer from chronic headaches or migraines, it is crucial to consult with a healthcare professional who can provide personalized recommendations and guidance. The ongoing research on the vagus nerve holds promise for the development of more effective and targeted treatments, bringing hope to those who experience the debilitating effects of headaches.
If you’re fascinated by the role of the vagus nerve in managing headaches and wish to delve deeper into understanding this complex system, “My Vagus Nerve & Me Book” is the perfect resource. Discover the wonders of one of the most sophisticated systems in the human body and learn how it influences everything from your heart rate to your mental health. This comprehensive book will guide you through the intricacies of the vagus nerve, its functions, and both natural and artificial methods of stimulation. Take the first step towards harnessing the power of your vagus nerve for improved well-being. Get My Vagus Nerve & Me eBook today and embark on a journey to better health.