Cardiac arrest is a life-threatening condition that occurs when the heart suddenly stops beating. This can be caused by various factors such as a heart attack, a severe electrolyte imbalance, or trauma to the heart. While the causes and symptoms of cardiac arrest are well-documented, recent research has shed light on the potential role of the vagus nerve in this condition. Understanding the connection between the vagus nerve and cardiac arrest is crucial in developing new therapeutic approaches and improving patient outcomes.
Understanding the Vagus Nerve
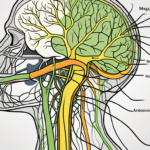
The vagus nerve, also known as the tenth cranial nerve, is a complex and vital part of the autonomic nervous system. It is the longest cranial nerve in the body and extends from the brainstem to various organs, including the heart, lungs, and digestive system. The vagus nerve is responsible for regulating many essential bodily functions, such as heart rate, digestion, and breathing.
But what exactly makes the vagus nerve so fascinating? Let’s dive deeper into the anatomy and function of this remarkable nerve.
Anatomy and Function of the Vagus Nerve
The vagus nerve consists of both sensory and motor fibers, which allow it to transmit information between the brain and various organs. It originates from the medulla oblongata, a region in the brainstem, and branches out into multiple smaller nerve fibers. These branches innervate different organs and tissues, enabling communication between the brain and the body.
Interestingly, the vagus nerve is not just a one-way street. It carries signals from the body back to the brain, providing crucial feedback that helps maintain homeostasis. This bidirectional communication allows the brain to constantly monitor and adjust various bodily functions.
Furthermore, the vagus nerve is a key player in the parasympathetic branch of the autonomic nervous system. The parasympathetic branch is responsible for the body’s “rest and digest” functions, promoting relaxation and conserving energy. The vagus nerve plays a vital role in maintaining homeostasis by controlling heart rate, gastrointestinal motility, and other vital functions.
When the body is in a state of rest, the vagus nerve releases acetylcholine, a neurotransmitter that slows down heart rate, dilates blood vessels, and aids in digestion. This allows the body to allocate resources to essential processes like nutrient absorption and tissue repair.
Moreover, recent research has shown that the vagus nerve also plays a crucial role in regulating inflammation. It communicates with the immune system, helping to modulate the body’s response to infection and injury. This connection between the nervous and immune systems highlights the intricate interplay between different physiological processes.
The Vagus Nerve and the Autonomic Nervous System
The autonomic nervous system consists of two main branches: the sympathetic and the parasympathetic systems. While the sympathetic system is associated with the “fight or flight” response, the parasympathetic system, regulated by the vagus nerve, promotes relaxation and counterbalances the sympathetic response.
During times of stress or danger, the sympathetic system prepares the body for action by increasing heart rate, constricting blood vessels, and releasing stress hormones like adrenaline. However, once the threat has passed, the parasympathetic system, under the control of the vagus nerve, takes over to restore balance and calmness.
The vagus nerve acts as a brake pedal, slowing down the body’s stress response and allowing it to return to a state of equilibrium. This delicate balance between the sympathetic and parasympathetic systems ensures the body functions optimally under different circumstances.
Interestingly, the vagus nerve’s influence extends beyond the physical realm. Emerging research suggests that it also plays a role in regulating emotions and social behavior. Studies have shown that stimulating the vagus nerve can have mood-enhancing effects and may even be beneficial in treating certain psychiatric disorders.
In conclusion, the vagus nerve is an extraordinary component of the autonomic nervous system, connecting the brain to various organs and playing a crucial role in maintaining homeostasis. Its intricate anatomy and multifaceted functions make it a subject of great interest and ongoing research. Understanding the vagus nerve opens up new possibilities for improving our overall well-being and sheds light on the fascinating interplay between mind and body.
The Vagus Nerve’s Role in Heart Function
The vagus nerve plays a significant role in regulating heart function, including heart rate and rhythm. This intricate connection between the vagus nerve and the heart is crucial for maintaining a healthy cardiovascular system. Understanding how the vagus nerve influences heart function is essential in comprehending its potential impact on cardiac arrest.
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It originates in the brainstem and extends down to various organs in the body, including the heart. This extensive network of nerve fibers allows for bidirectional communication between the brain and the heart, enabling precise control over heart rate and rhythm.
Heart Rate Regulation and the Vagus Nerve
The vagus nerve acts as a natural pacemaker for the heart, helping to regulate heart rate. When activated, the vagus nerve releases acetylcholine, which slows down the heart rate. This mechanism ensures that the heart pumps blood efficiently, adapting to the body’s needs.
Interestingly, the vagus nerve’s influence on heart rate can be observed in various situations. For example, during periods of rest or relaxation, the vagus nerve is more active, resulting in a lower resting heart rate. On the other hand, during times of stress or physical exertion, the vagus nerve activity decreases, allowing the heart rate to increase to meet the body’s demands.
However, in certain situations, an overactive vagus nerve can lead to bradycardia, a condition characterized by an extremely low heart rate. This can result in inadequate blood flow to vital organs and potentially trigger cardiac arrest. Understanding the delicate balance between the vagus nerve’s influence on heart rate and the potential risks involved is crucial in cardiac arrest prevention.
The Vagus Nerve and Heart Rhythm
In addition to heart rate regulation, the vagus nerve also plays a role in maintaining normal heart rhythm. Abnormalities in heart rhythm, known as arrhythmias, can increase the risk of cardiac arrest. The vagus nerve helps to stabilize heart rhythm by modulating the electrical signals within the heart.
The electrical signals that control heart rhythm are generated by specialized cells in the heart called pacemaker cells. These cells create a synchronized pattern of electrical impulses that coordinate the contraction of the heart muscles. The vagus nerve exerts its influence on heart rhythm by altering the activity of these pacemaker cells.
In situations where the vagus nerve is overactive or hypersensitive, it can lead to an increased incidence of arrhythmias, including ventricular fibrillation, a life-threatening rhythm disturbance. Ventricular fibrillation occurs when the heart’s electrical signals become chaotic, causing the heart to quiver instead of pumping blood effectively. Immediate medical intervention, such as defibrillation, is required to restore a normal heart rhythm and prevent cardiac arrest.
Researchers are actively studying the vagus nerve’s role in heart rhythm disorders and exploring potential therapeutic interventions. By understanding the intricacies of the vagus nerve’s influence on heart function, medical professionals can develop targeted treatments that aim to restore balance and prevent life-threatening arrhythmias.
Cardiac Arrest: A Brief Overview
Before delving deeper into the vagus nerve’s role in cardiac arrest, it is essential to understand the basics of this life-threatening condition. Cardiac arrest occurs when the heart suddenly stops pumping blood effectively, leading to a lack of blood flow and oxygen to the organs and tissues.
Cardiac arrest is a medical emergency that requires immediate attention. Without prompt intervention, it can quickly lead to irreversible damage to vital organs and, ultimately, death. It is estimated that more than 350,000 out-of-hospital cardiac arrests occur in the United States each year, with survival rates ranging from 2% to 12%.
Causes and Symptoms of Cardiac Arrest
Cardiac arrest can be caused by various factors, including coronary artery disease, heart attack, electrolyte imbalances, and structural abnormalities of the heart. These underlying conditions can disrupt the heart’s normal electrical activity and rhythm, leading to a sudden cessation of effective pumping.
The symptoms of cardiac arrest are often abrupt and severe. The affected individual may experience a sudden loss of consciousness, lack of pulse, and cessation of breathing. It is important to note that not all individuals will experience warning signs or symptoms before cardiac arrest occurs. Therefore, recognizing the risk factors and being prepared to respond swiftly is crucial for improving the chances of survival.
While the causes and symptoms of cardiac arrest are multifaceted and can vary from person to person, understanding the underlying mechanisms and potential triggers is crucial in developing effective preventive strategies.
The Role of the Heart’s Electrical System in Cardiac Arrest
The heart relies on a complex electrical system to maintain a synchronized contraction and pump blood efficiently. Disruptions in this electrical system can lead to abnormal heart rhythms and, in severe cases, cause cardiac arrest.
One of the primary risk factors for cardiac arrest is ventricular fibrillation, a chaotic and disorganized rhythm that prevents the heart from effectively pumping blood. Ventricular fibrillation is often triggered by underlying heart conditions such as coronary artery disease or previous heart attacks.
Understanding the intricate interplay between the heart’s electrical system and the vagus nerve can provide valuable insights into preventing and managing cardiac arrest. The vagus nerve, also known as the “wandering nerve,” is a critical component of the parasympathetic nervous system. It plays a significant role in regulating heart rate, blood pressure, and other vital functions.
Research suggests that the vagus nerve can influence the heart’s electrical activity and potentially contribute to the development of abnormal rhythms that can lead to cardiac arrest. By studying the complex interactions between the vagus nerve and the heart, scientists and healthcare professionals aim to develop targeted interventions and therapies to prevent and treat cardiac arrest.
Advancements in medical technology and research have paved the way for innovative approaches to managing cardiac arrest. From the development of automated external defibrillators (AEDs) to the implementation of bystander CPR training programs, efforts are being made to improve survival rates and outcomes for individuals experiencing cardiac arrest.
In conclusion, cardiac arrest is a life-threatening condition that requires immediate medical attention. Understanding the causes, symptoms, and underlying mechanisms of cardiac arrest is crucial for developing effective preventive strategies and improving survival rates. Ongoing research into the role of the heart’s electrical system and the vagus nerve provides hope for future advancements in the management and treatment of this critical condition.
The Vagus Nerve-Cardiac Arrest Connection
Emerging research suggests that the vagus nerve may be involved in the development and progression of cardiac arrest. Understanding the potential mechanisms by which the vagus nerve can trigger or contribute to cardiac arrest is essential for identifying novel therapeutic approaches.
How the Vagus Nerve Can Trigger Cardiac Arrest
Excessive vagal activity, often as a result of an overactive or hypersensitive vagus nerve, can lead to a sudden drop in heart rate and blood pressure. In extreme cases, this can cause the heart to stop altogether, resulting in cardiac arrest. Identifying the triggers that can prompt an overactive vagus nerve response is a crucial area of ongoing research.
One potential trigger for an overactive vagus nerve response is stress. When a person experiences high levels of stress, the body’s sympathetic nervous system is activated, leading to an increase in heart rate and blood pressure. In response to this activation, the vagus nerve may attempt to counterbalance the sympathetic response by slowing down the heart rate. However, if the vagus nerve becomes overactive, it can cause the heart rate to drop too low, potentially leading to cardiac arrest.
Another factor that can contribute to an overactive vagus nerve response is certain medications. Some medications, such as beta blockers, are known to affect the function of the vagus nerve. These medications are commonly prescribed to individuals with high blood pressure or heart conditions. While beta blockers can be effective in managing these conditions, they can also increase the risk of cardiac arrest if the vagus nerve becomes overly stimulated.
It is important to note that the vagus nerve is just one factor in the development of cardiac arrest. Other risk factors such as underlying heart disease, electrolyte imbalances, and genetic predispositions also play a significant role. Consultation with a medical professional is essential in comprehensively evaluating an individual’s risk and developing appropriate preventive strategies.
The Vagus Nerve and Sudden Cardiac Arrest Risk
Individuals with certain medical conditions, such as epilepsy or long QT syndrome, may be at an increased risk of sudden cardiac arrest triggered by vagal activity. The interplay between these conditions and the vagus nerve warrants further investigation to develop targeted interventions and preventive measures.
Epilepsy is a neurological disorder characterized by recurrent seizures. During a seizure, there can be abnormal electrical activity in the brain, which can also affect the vagus nerve. In some cases, this abnormal activity can lead to an overstimulation of the vagus nerve, resulting in a sudden drop in heart rate and potentially triggering cardiac arrest. Understanding the specific mechanisms involved in this interplay between epilepsy, the vagus nerve, and cardiac arrest is crucial for developing effective treatment strategies for individuals with epilepsy.
Long QT syndrome is a genetic disorder that affects the heart’s electrical activity. It can cause an abnormal prolongation of the QT interval on an electrocardiogram (ECG), which increases the risk of life-threatening arrhythmias. In some cases, vagal activity can further disrupt the heart’s electrical system, potentially leading to sudden cardiac arrest. Identifying the specific genetic mutations and mechanisms that contribute to this increased risk is an area of active research.
In conclusion, while the vagus nerve plays a significant role in the development and progression of cardiac arrest, it is important to consider it as part of a complex interplay of various factors. Ongoing research aims to unravel the intricate mechanisms involved in the vagus nerve-cardiac arrest connection, with the ultimate goal of developing targeted interventions and preventive measures to reduce the incidence and impact of cardiac arrest.
Potential Therapeutic Approaches
Understanding the vagus nerve’s role in cardiac arrest opens up new avenues for potential therapeutic approaches. One such approach is vagus nerve stimulation.
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It plays a crucial role in regulating various bodily functions, including heart rate, digestion, and respiratory function. By stimulating the vagus nerve, researchers hope to harness its potential in preventing and treating cardiac arrest.
Vagus Nerve Stimulation and Cardiac Arrest
Vagus nerve stimulation (VNS) involves the use of electrical impulses to stimulate the vagus nerve. This technique has shown promise in various medical conditions, including epilepsy and depression. In the context of cardiac arrest, VNS holds potential as a preventive and therapeutic modality, by modulating vagal activity and reducing the risk of arrhythmias.
Studies have demonstrated that VNS can influence heart rate variability, a measure of the heart’s ability to adapt to changing conditions. By enhancing parasympathetic activity through VNS, researchers believe they can improve cardiac function and reduce the likelihood of life-threatening arrhythmias that can lead to cardiac arrest.
However, it is important to note that VNS is still an evolving field of research, and its specific role in preventing cardiac arrest is yet to be established conclusively. Consulting with a healthcare professional is vital for a comprehensive evaluation of an individual’s suitability for VNS and to explore other appropriate therapeutic options.
Future Research Directions in Vagus Nerve and Cardiac Health
The vagus nerve’s impact on cardiac arrest is an exciting area of research that continues to evolve. Ongoing studies aim to elucidate the intricate mechanisms underlying the vagus nerve’s role in cardiac health and develop more targeted and effective preventive strategies.
Future research directions may include evaluating the potential influence of lifestyle factors and interventions such as stress reduction, exercise, and dietary modifications on vagal activity and cardiac arrest risk. For example, stress is known to have a negative impact on heart health, and finding ways to reduce stress levels could potentially improve vagal tone and reduce the risk of cardiac arrest.
Additionally, exploring the efficacy of emerging technologies and non-invasive interventions in modulating vagal activity could pave the way for innovative therapeutic approaches. For instance, transcutaneous vagus nerve stimulation (tVNS) is a non-invasive technique that involves the application of electrical impulses to the skin overlying the vagus nerve. Preliminary studies have shown promising results in improving cardiac function and reducing the risk of arrhythmias.
Furthermore, advancements in neuroimaging techniques, such as functional magnetic resonance imaging (fMRI), can provide valuable insights into the neural pathways involved in vagal modulation of cardiac function. By understanding these pathways, researchers can develop more targeted interventions to optimize vagal activity and improve cardiac health.
In conclusion, the vagus nerve’s role in cardiac arrest is a complex and fascinating area of study. Vagus nerve stimulation and other therapeutic approaches hold promise in preventing and treating cardiac arrest, but further research is needed to fully understand their potential benefits and limitations. With continued investigation and innovation, we can hope to develop more effective strategies to protect and enhance cardiac health.
Conclusion
The connection between the vagus nerve and cardiac arrest is a complex and multifaceted area of research. Understanding the vagus nerve’s role in heart function, its potential impact on cardiac arrest, and identifying appropriate therapeutic approaches are critical for improving patient outcomes and reducing the burden of cardiac arrest.
While research continues to expand our knowledge in this field, it is important to consult with healthcare professionals for comprehensive evaluation, risk assessment, and personalized management strategies. By harnessing the power of scientific advancements and collaborative efforts, we can make significant strides in unraveling the complexities of the vagus nerve-cardiac arrest connection and pave the way for more effective preventive and therapeutic interventions.
As we’ve explored the critical role of the vagus nerve in cardiac health and its connection to cardiac arrest, it’s clear that understanding this complex system is key to our overall well-being. The “My Vagus Nerve & Me Book” delves into the fascinating intricacies of the vagus nerve, offering insights into its functions and the natural and artificial ways to stimulate it for optimal health. Whether you’re interested in enhancing your immune system, regulating your heart rate, or improving mental health, this book is an invaluable resource. Don’t miss the opportunity to learn more about one of the most sophisticated systems in your body. Get My Vagus Nerve & Me eBook today and embark on a journey to better understand and harness the power of your vagus nerve.