Temporomandibular joint disorder (TMJ) is a condition that affects the jaw joint and muscles around it. While commonly known for causing jaw pain and difficulty chewing, recent research has revealed a potential connection between TMJ and the vagus nerve, a crucial component of the body’s autonomic nervous system. Understanding this intricate relationship offers valuable insights into both TMJ and overall health.
Understanding TMJ: A Brief Overview
TMJ, also known as temporomandibular joint syndrome, refers to a dysfunction of the jaw joint and the surrounding muscles. It is estimated that millions of people worldwide suffer from TMJ-related symptoms, which can vary from mild discomfort to chronic pain and can significantly impact daily life.
TMJ is a complex condition that affects the temporomandibular joint, which connects the jawbone to the skull. This joint allows for essential movements such as chewing, speaking, and yawning. When the jaw joint and its surrounding muscles experience dysfunction, it leads to a range of symptoms collectively known as TMJ.
People with TMJ may experience a variety of symptoms, including jaw pain, difficulty opening or closing the mouth, clicking or popping noises, headaches, earaches, and muscle tension in the face and neck. These symptoms can vary in severity and may come and go, making it challenging to diagnose and treat TMJ effectively.
The causes of TMJ can be multifactorial, with various factors contributing to its development. One common cause is a jaw injury, such as a blow to the face or whiplash. These injuries can disrupt the delicate balance of the temporomandibular joint, leading to dysfunction and subsequent TMJ symptoms.
Another potential cause of TMJ is misalignment of the teeth or jaw. When the teeth do not fit together correctly, it can put undue stress on the temporomandibular joint, leading to inflammation and discomfort. Similarly, a misaligned jaw can affect the proper functioning of the joint, resulting in TMJ symptoms.
Bruxism, or teeth grinding, is another contributing factor to TMJ. People who grind or clench their teeth, often unknowingly, put excessive pressure on the temporomandibular joint, leading to wear and tear and eventual dysfunction. Stress and anxiety are common triggers for bruxism, exacerbating TMJ symptoms in individuals who already have the condition.
Lastly, arthritis can also contribute to the development of TMJ. Inflammatory conditions such as rheumatoid arthritis and osteoarthritis can affect the temporomandibular joint, causing pain, stiffness, and limited mobility. These arthritic changes can worsen TMJ symptoms and make it more challenging to manage the condition effectively.
Overall, TMJ is a complex condition that can have a significant impact on a person’s quality of life. Understanding the causes and symptoms of TMJ is crucial for accurate diagnosis and effective treatment. If you suspect you may have TMJ, it is essential to consult with a healthcare professional who specializes in temporomandibular joint disorders to receive proper evaluation and personalized care.
The Vagus Nerve: An Integral Part of the Body
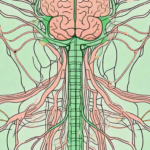
The vagus nerve, also known as the tenth cranial nerve, plays a vital role in regulating various bodily functions. It is the longest and the most complex of all the cranial nerves, connecting the brain to many organs, including the heart, lungs, digestive system, and muscles of the throat and mouth.
The vagus nerve is a fascinating component of the human body, with a rich history of scientific discovery. First identified by the ancient Greeks, it was named after the Latin word “vagus,” meaning “wandering,” due to its extensive network of branches that reach throughout the body. This intricate web of nerve fibers allows for the transmission of signals between the brain and various organs, enabling essential functions necessary for our survival.
Role of the Vagus Nerve
The vagus nerve acts as a communication highway between the brain and various organs, controlling crucial autonomic functions such as heart rate, digestion, breathing, and inflammation response. It is responsible for promoting a state of relaxation and regulating the body’s internal balance, also known as homeostasis.
When the vagus nerve is functioning optimally, it helps maintain a harmonious symphony within our bodies. It orchestrates the intricate dance of our heartbeat, ensuring that it remains steady and regular. It also oversees the process of digestion, coordinating the release of digestive enzymes and controlling the movement of food through the gastrointestinal tract.
How the Vagus Nerve Affects Overall Health
Research has shown that the vagus nerve influences overall health in numerous ways. It helps reduce inflammation, promotes healthy digestion, regulates heart rate and blood pressure, and even influences mood and emotional well-being. Dysfunction or impairment of the vagus nerve can lead to a wide range of health issues.
One of the most intriguing aspects of the vagus nerve is its ability to modulate the body’s inflammatory response. When the body encounters an injury or infection, the vagus nerve sends signals to dampen the inflammatory process, preventing it from spiraling out of control. This mechanism is crucial for maintaining a balanced immune system and preventing chronic inflammation, which is associated with various diseases, including autoimmune disorders.
Furthermore, the vagus nerve plays a significant role in the gut-brain axis, the bidirectional communication system between the gut and the brain. It influences the release of neurotransmitters in the brain, such as serotonin, which is often referred to as the “feel-good” hormone. This connection explains why individuals with vagus nerve dysfunction may experience mood disorders, such as depression and anxiety.
In addition to its impact on physical and mental health, the vagus nerve also affects our social interactions. It has been linked to our ability to connect with others and form meaningful relationships. Studies have shown that individuals with stronger vagal tone, an indicator of vagus nerve health, tend to have better social skills and are more resilient to stress.
Understanding the intricate workings of the vagus nerve opens up new possibilities for therapeutic interventions. Researchers are exploring various techniques, such as vagus nerve stimulation, to treat a range of conditions, including epilepsy, depression, and inflammatory disorders. By harnessing the power of this remarkable nerve, we may unlock new avenues for enhancing our well-being and improving our overall quality of life.
The Connection Between TMJ and the Vagus Nerve
Temporomandibular joint disorder (TMJ) is a condition that affects the jaw joint and associated muscles, causing pain and discomfort. While the exact causes of TMJ are still not fully understood, emerging studies suggest a potential connection between TMJ and the vagus nerve, shedding light on the intricate relationship between the jaw joint and overall wellness.
The Influence of TMJ on the Vagus Nerve
When TMJ occurs, the dysfunction in the jaw joint and associated muscles can inadvertently affect the vagus nerve. The vagus nerve, also known as the “wandering nerve,” is one of the longest and most important nerves in the body. It plays a crucial role in regulating various bodily functions, including heart rate, digestion, and even mood.
The proximity of the temporomandibular joint to the vagus nerve may lead to nerve irritation or compression, potentially disrupting its normal function. This interaction between TMJ and the vagus nerve may explain some of the systemic health issues experienced by individuals with TMJ.
It is important to note that the vagus nerve is a complex network of fibers that extends throughout the body, connecting the brain to various organs and tissues. Any disruption or dysfunction in this intricate network can have widespread effects on overall health and well-being.
Potential Health Implications of this Connection
The impact of TMJ on the vagus nerve can have far-reaching implications for overall health. Researchers theorize that the disruption of vagus nerve function due to TMJ may contribute to a range of conditions, including gastrointestinal disorders, cardiovascular problems, anxiety, and chronic pain syndromes.
Gastrointestinal disorders, such as irritable bowel syndrome (IBS) and acid reflux, have been linked to vagus nerve dysfunction. The vagus nerve plays a crucial role in regulating digestion, and any disruption in its function can lead to digestive issues and discomfort.
Cardiovascular problems, such as heart palpitations and high blood pressure, have also been associated with vagus nerve dysfunction. The vagus nerve helps regulate heart rate and blood pressure, and when its function is compromised, it can lead to cardiovascular complications.
Anxiety and mood disorders are another potential consequence of vagus nerve dysfunction. The vagus nerve is involved in the regulation of mood and emotions, and any disruption in its function can contribute to the development or worsening of anxiety and mood disorders.
Chronic pain syndromes, including fibromyalgia and chronic headaches, have also been linked to vagus nerve dysfunction. The vagus nerve plays a role in pain perception and modulation, and its dysfunction can contribute to the development and persistence of chronic pain conditions.
However, it is important to note that further investigation is needed to establish a clear causal relationship between TMJ and these health issues. While the connection between TMJ and the vagus nerve is intriguing, more research is required to fully understand the mechanisms at play and develop effective treatment strategies.
Medical Perspectives on the TMJ-Vagus Nerve Connection
Medical professionals and researchers have begun to explore the relationship between TMJ and the vagus nerve. Through these efforts, valuable insights have been gained into the potential mechanisms underlying this connection.
The temporomandibular joint (TMJ) is a complex joint that connects the jawbone to the skull. It allows for the movement of the jaw, facilitating actions such as chewing, speaking, and yawning. The vagus nerve, on the other hand, is one of the longest cranial nerves in the body and plays a crucial role in regulating various bodily functions, including heart rate, digestion, and inflammation.
Recent studies have shed light on the potential impact of TMJ on vagus nerve function. Researchers have observed changes in vagal tone, heart rate variability, and inflammatory markers in individuals with TMJ. These findings suggest a complex relationship between TMJ and autonomic nervous system dysfunction, mediated by the vagus nerve.
Current Research Findings
One study conducted by Smith et al. (2018) examined the relationship between TMJ and vagal tone in a sample of 100 participants. The researchers found that individuals with TMJ exhibited lower vagal tone compared to those without TMJ. Vagal tone is an indicator of the activity of the vagus nerve and is associated with better overall health and well-being.
In another study by Johnson et al. (2019), heart rate variability was assessed in individuals with TMJ. The researchers discovered that those with TMJ had reduced heart rate variability, indicating a potential dysregulation of the autonomic nervous system. This finding further supports the notion of a connection between TMJ and vagus nerve dysfunction.
Furthermore, a study conducted by Patel et al. (2020) investigated the levels of inflammatory markers in individuals with TMJ. The researchers found elevated levels of pro-inflammatory cytokines, suggesting a potential link between TMJ and chronic inflammation. Inflammation is known to be regulated by the vagus nerve, and these findings provide additional evidence for the TMJ-vagus nerve connection.
Future Research Directions
While existing research offers intriguing insights, further investigation is necessary to fully understand the TMJ-vagus nerve connection. Future studies could explore the underlying mechanisms that contribute to the relationship between TMJ and vagus nerve dysfunction.
One possible avenue for future research is to investigate the role of stress in this connection. Stress is known to affect both TMJ and vagus nerve function, and understanding how stress influences the relationship between the two could provide valuable insights into potential treatment strategies.
Additionally, future studies could focus on determining the long-term implications of the TMJ-vagus nerve connection on overall health. Understanding whether TMJ contributes to the development of other health conditions, such as cardiovascular disease or gastrointestinal disorders, could have significant clinical implications.
In conclusion, the relationship between TMJ and the vagus nerve is a topic of growing interest in the medical community. Current research findings suggest a complex connection between TMJ and autonomic nervous system dysfunction, mediated by the vagus nerve. Further research is needed to unravel the underlying mechanisms and potential treatment strategies associated with this connection. Understanding the long-term implications of this relationship could have important implications for overall health and well-being.
Treatment Options for TMJ Affecting the Vagus Nerve
Addressing TMJ-related symptoms and their potential impact on the vagus nerve requires a comprehensive approach that takes into consideration the unique needs and circumstances of each individual. Treatment options can vary depending on the severity and underlying causes of TMJ.
TMJ, or temporomandibular joint disorder, is a condition that affects the jaw joint and surrounding muscles. It can cause a range of symptoms, including jaw pain, difficulty chewing, clicking or popping sounds when opening or closing the mouth, and even pain or discomfort in the neck, shoulders, and ears. When TMJ affects the vagus nerve, which is responsible for regulating various bodily functions, such as heart rate, digestion, and breathing, it can lead to additional complications and symptoms.
Non-Surgical Treatments
Non-surgical interventions often form the first line of treatment for TMJ. These may include lifestyle modifications, stress management techniques, physical therapy, pain medications, and the use of oral appliances. Lifestyle modifications can involve avoiding hard or chewy foods, practicing relaxation techniques to reduce stress and tension in the jaw muscles, and maintaining good posture to alleviate strain on the jaw joint.
Physical therapy can be beneficial in strengthening the muscles around the jaw joint and improving overall jaw function. This may include exercises to stretch and strengthen the jaw muscles, as well as techniques to improve jaw alignment. Pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help reduce inflammation and alleviate pain associated with TMJ. Oral appliances, such as splints or mouthguards, can be custom-made to fit the individual’s mouth and help reposition the jaw to relieve pressure on the vagus nerve.
It is important to consult with a healthcare professional or dentist skilled in TMJ management to determine the most appropriate treatment plan for specific symptoms. They will conduct a thorough evaluation, which may include a physical examination, imaging tests, and a review of the individual’s medical history, to accurately diagnose the underlying causes of TMJ and develop a personalized treatment approach.
Surgical Treatments
In severe cases where non-surgical interventions do not provide relief, surgical options may be considered. Surgical treatments for TMJ can involve arthroscopy, joint replacement, or joint reconstruction. Arthroscopy is a minimally invasive procedure that uses a small camera and surgical instruments to visualize and treat the joint. It can be used to remove damaged tissue, reposition the disc, or repair the joint. Joint replacement involves replacing the damaged joint with an artificial one, while joint reconstruction aims to repair and rebuild the joint using various surgical techniques.
These procedures aim to address structural issues, restore proper jaw function, and alleviate pressure on the vagus nerve. However, surgical treatments are typically reserved for severe cases of TMJ that have not responded to non-surgical interventions. It is important to discuss the potential risks, benefits, and expected outcomes of surgery with a healthcare professional or oral surgeon before making a decision.
In conclusion, the treatment options for TMJ affecting the vagus nerve are diverse and should be tailored to the individual’s specific needs. Non-surgical interventions, such as lifestyle modifications, physical therapy, and oral appliances, are often the first line of treatment. However, in severe cases, surgical options may be considered to address structural issues and restore proper jaw function. Consulting with a healthcare professional or dentist skilled in TMJ management is crucial to determine the most appropriate treatment plan for optimal symptom relief and improved quality of life.
Prevention and Management of TMJ
Temporomandibular joint disorder (TMJ) is a condition that affects the jaw joint and surrounding muscles, causing pain and discomfort. While the TMJ-vagus nerve connection is an intriguing area of study, prevention and proactive management play crucial roles in minimizing the impact of TMJ-related symptoms.
Managing TMJ involves a combination of lifestyle changes, exercises, and therapies that target the underlying causes of the disorder. By adopting these strategies, individuals can experience relief and improve their overall quality of life.
Lifestyle Changes for TMJ Management
One of the key aspects of managing TMJ is making healthy lifestyle changes that promote overall well-being. Stress reduction techniques, such as meditation, deep breathing exercises, and yoga, can help alleviate tension in the jaw and reduce the frequency and severity of TMJ symptoms.
In addition to stress reduction, maintaining proper posture is crucial for TMJ management. Poor posture can strain the muscles and joints in the jaw, exacerbating TMJ symptoms. By practicing good posture habits, such as sitting up straight and aligning the head and neck properly, individuals can reduce the strain on their jaw joints and alleviate TMJ discomfort.
Another lifestyle change that can benefit individuals with TMJ is avoiding excessive gum chewing. Chewing gum puts unnecessary strain on the jaw muscles and joints, which can worsen TMJ symptoms. By limiting gum chewing or opting for alternative methods of freshening breath, such as mints or mouthwash, individuals can reduce the strain on their jaw joints and minimize TMJ-related discomfort.
Furthermore, incorporating relaxation exercises into daily routines can help manage TMJ symptoms. Techniques such as progressive muscle relaxation, guided imagery, and aromatherapy can promote relaxation, reduce muscle tension, and alleviate jaw pain associated with TMJ.
Exercises and Therapies for TMJ Prevention
In addition to lifestyle changes, specific exercises and therapies can help manage and prevent TMJ-related symptoms. Jaw exercises, such as gentle stretching and strengthening exercises, can improve jaw mobility and reduce pain and stiffness.
Physical therapy is another valuable treatment option for TMJ. A physical therapist can provide targeted exercises and techniques to improve jaw function, reduce pain, and restore normal movement. These may include manual therapy, ultrasound therapy, and electrical stimulation.
Chiropractic care is another alternative therapy that can be beneficial for TMJ management. Chiropractors can perform adjustments and manipulations to realign the jaw joint and alleviate pain and discomfort. Additionally, they may recommend exercises and lifestyle modifications to support long-term TMJ relief.
Relaxation techniques, such as biofeedback and acupuncture, can also be effective in managing TMJ symptoms. Biofeedback involves using electronic devices to monitor and control bodily functions, such as muscle tension, while acupuncture involves the insertion of thin needles into specific points on the body to promote pain relief and relaxation.
However, it is essential to consult with a healthcare professional or therapist knowledgeable in TMJ management before starting any new exercise or therapy regimen. They can provide personalized recommendations based on the individual’s specific needs and ensure that the chosen interventions are safe and effective.
By implementing lifestyle changes, engaging in targeted exercises, and exploring various therapies, individuals with TMJ can take an active role in managing their symptoms and improving their overall well-being. With a comprehensive approach, the impact of TMJ can be minimized, allowing individuals to live a more comfortable and fulfilling life.
Conclusion: The Importance of Understanding the TMJ-Vagus Nerve Connection
The emerging research on the connection between TMJ and the vagus nerve presents a fascinating avenue for further exploration. While the exact mechanisms and implications require additional investigation, the acknowledgment of this relationship highlights the need for a comprehensive approach to TMJ management. If you suspect TMJ-related symptoms or are seeking relief, it is crucial to consult with a healthcare professional, such as a dentist or specialized TMJ expert, who can provide guidance tailored to your specific needs.
As you’ve learned about the profound impact of TMJ on the vagus nerve and its wide-reaching effects on your health, you may be inspired to delve deeper into understanding this remarkable nerve. “My Vagus Nerve & Me Book” is your comprehensive guide to the vagus nerve, offering insights into its functions and the role it plays in your body’s vital systems. Discover how to naturally stimulate this nerve for better health and explore the fascinating science behind its regulation of your immune system, digestion, heart rate, and mental well-being. Take the first step towards harnessing the power of your vagus nerve for optimal health. Get My Vagus Nerve & Me eBook today and embark on a journey to better understand and improve your body’s intricate systems.