The temporomandibular joint (TMJ) is a complex joint that connects the jawbone to the skull. It plays a crucial role in daily activities such as chewing, speaking, and yawning. However, TMJ disorders can cause chronic pain and discomfort, affecting the quality of life for millions of people worldwide. Recent research has revealed a fascinating connection between the vagus nerve and TMJ disorders, shedding light on potential new treatment approaches. In this article, we will explore the anatomy and function of the vagus nerve, understand its role in the body’s response to stress, and delve into the complexities of TMJ disorder. We will then discuss the interplay between the vagus nerve and TMJ pain, explore potential therapies targeting the vagus nerve, and conclude with a summary of the importance of the vagus nerve in TMJ management.
Understanding the Vagus Nerve
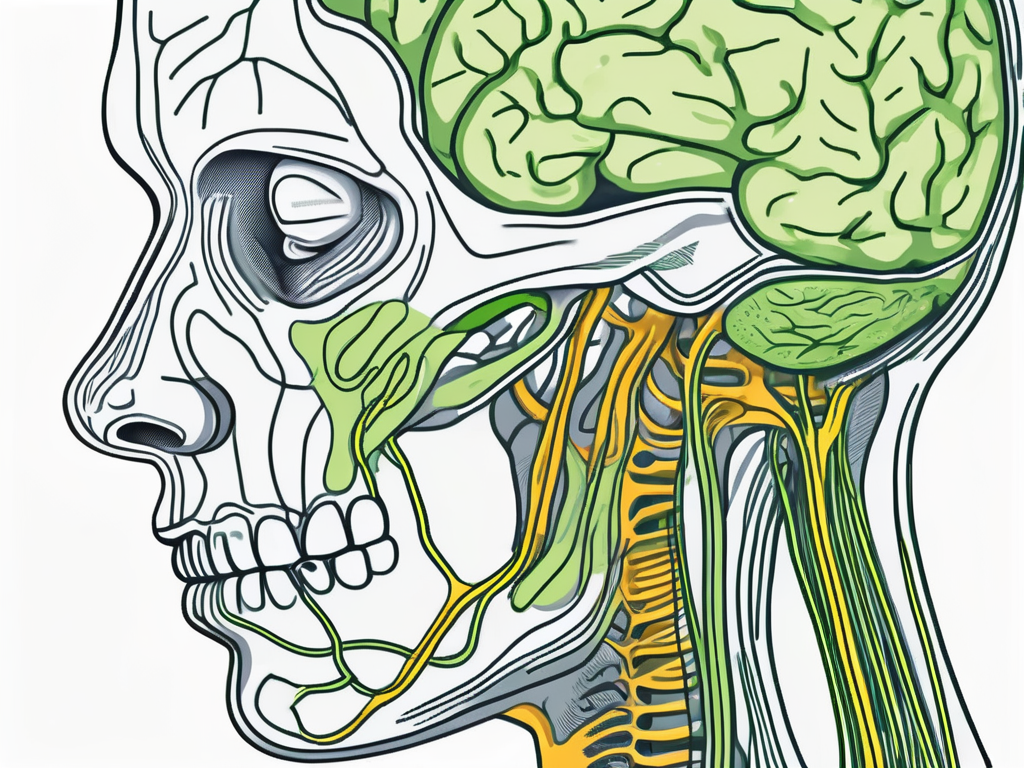
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex cranial nerve in the body. It extends from the brainstem to various organs throughout the body, including the heart, lungs, and gastrointestinal tract. The vagus nerve is responsible for regulating vital functions such as heart rate, breathing, digestion, and even emotional responses. It acts as a communication pathway between the brain and the body, playing a crucial role in maintaining homeostasis.
Let’s delve deeper into the anatomy and function of the vagus nerve to gain a better understanding of its significance in our overall well-being.
Anatomy of the Vagus Nerve
The vagus nerve originates in the medulla oblongata, a part of the brainstem located at the base of the skull. It emerges from the brainstem as a pair of nerves, one on each side of the head, and then descends through the neck and into the chest and abdomen. Along its journey, the vagus nerve branches out extensively, forming connections with various organs and tissues.
One of the major branches of the vagus nerve is the recurrent laryngeal nerve, which innervates the muscles in the larynx, enabling us to speak and produce sound. Another important branch is the auricular branch, which provides sensory innervation to the external ear.
Function of the Vagus Nerve
The vagus nerve plays a multifaceted role in regulating numerous bodily functions. One of its primary functions is to control the parasympathetic nervous system, which is responsible for promoting rest, relaxation, and digestion. When the body is in a state of calm, the vagus nerve helps slow down the heart rate, decrease blood pressure, and increase digestive activity.
In addition to its role in the parasympathetic nervous system, the vagus nerve also has a profound impact on our emotional well-being. It is intricately involved in the regulation of our mood, stress response, and social interactions. Studies have shown that stimulating the vagus nerve can alleviate symptoms of depression and anxiety, highlighting its therapeutic potential.
The Vagus Nerve’s Role in the Body’s Response to Stress
During times of stress, the body enters a state of heightened arousal known as the fight-or-flight response. The vagus nerve plays a critical role in regulating this response by activating the parasympathetic nervous system. By activating the parasympathetic nervous system, the vagus nerve helps counterbalance the stress response by promoting relaxation, reducing heart rate, and aiding digestion. This activation is essential for the body to return to a state of balance after a stressful event.
Moreover, the vagus nerve is involved in the release of neurotransmitters such as acetylcholine and gamma-aminobutyric acid (GABA), which have calming and inhibitory effects on the brain. These neurotransmitters help dampen the stress response and promote a sense of calm and well-being.
Furthermore, recent research has uncovered a fascinating connection between the vagus nerve and the gut microbiome. The vagus nerve communicates bidirectionally with the gut, influencing the composition and activity of the trillions of microorganisms residing in our digestive system. This gut-brain axis plays a crucial role in regulating mood, cognition, and overall mental health.
In conclusion, the vagus nerve is a remarkable structure that serves as a vital link between the brain and the body. Its intricate network of connections and its role in regulating various physiological and emotional processes make it a fascinating area of study. Understanding the vagus nerve can provide valuable insights into how we can optimize our well-being and harness its therapeutic potential.
The Complexities of Temporomandibular Joint (TMJ) Disorder
Symptoms and Causes of TMJ Disorder
TMJ disorder is a complex condition that affects the temporomandibular joint and the surrounding muscles. It is characterized by pain, discomfort, and dysfunction in the jaw joint. People with TMJ disorder may experience a range of symptoms, including:
- Jaw pain
- Clicking or popping sounds when opening or closing the mouth
- Difficulty chewing
- Headaches
The exact cause of TMJ disorder is often multifactorial, meaning that it involves a combination of factors. Some of the common causes and contributing factors include:
- Genetics: Certain genetic factors may predispose individuals to develop TMJ disorder.
- Jaw injury: Trauma to the jaw, such as a direct blow or whiplash, can lead to the development of TMJ disorder.
- Arthritis: Various forms of arthritis, including osteoarthritis and rheumatoid arthritis, can affect the temporomandibular joint and contribute to TMJ disorder.
- Teeth grinding: Habitual teeth grinding, also known as bruxism, can put excessive pressure on the jaw joint and lead to TMJ disorder.
- Stress and anxiety: High levels of stress and anxiety can exacerbate TMJ symptoms, as they can cause muscle tension and increase jaw clenching.
The Role of the Nervous System in TMJ Disorder
The nervous system plays a crucial role in the development and maintenance of TMJ disorder. One of the key players in this intricate relationship is the trigeminal nerve, which is responsible for sensation in the face and motor control of the jaw muscles. Dysfunction in the trigeminal nerve can contribute to TMJ pain and discomfort.
Recent studies have also shed light on the potential involvement of the vagus nerve in TMJ disorder. The vagus nerve, known for its role in regulating the stress response, may play a role in the development and modulation of TMJ disorder. This suggests that the connection between stress and TMJ symptoms may be mediated, at least in part, by the vagus nerve.
Understanding the complexities of TMJ disorder requires a comprehensive approach that takes into account the various factors involved, including genetics, injury, arthritis, teeth grinding, and the role of the nervous system. By gaining a deeper understanding of these complexities, healthcare professionals can develop more effective treatment strategies and improve the quality of life for individuals with TMJ disorder.
The Vagus Nerve-TMJ Connection
How the Vagus Nerve Influences TMJ Disorder
Researchers have found that the vagus nerve’s activity can impact the severity of TMJ symptoms. When the vagus nerve is not functioning optimally, as seen in individuals experiencing chronic stress or anxiety, it may contribute to increased inflammation and sensitivity in the jaw joint. Moreover, the vagus nerve may influence the release of neurotransmitters in the brain that modulate pain perception, potentially exacerbating TMJ-related pain.
Understanding the intricate connection between the vagus nerve and TMJ disorder is crucial in developing effective treatment strategies. The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It plays a vital role in regulating various bodily functions, including heart rate, digestion, and inflammation. Additionally, recent research has shed light on its involvement in pain modulation, making it a potential target for managing TMJ-related pain.
Chronic stress and anxiety have been shown to negatively impact vagus nerve function, leading to a dysregulated autonomic nervous system response. This dysregulation can result in heightened inflammation and increased pain sensitivity in the temporomandibular joint (TMJ). The TMJ is the joint that connects the jawbone to the skull and is responsible for facilitating movements such as chewing and speaking. When the vagus nerve is not functioning optimally, it may contribute to the development or worsening of TMJ disorder.
The Interplay Between the Vagus Nerve and TMJ Pain
Studies have suggested that the vagus nerve may play a role in reducing pain sensitivity and promoting pain relief. Vagus nerve stimulation, a therapeutic approach that involves gentle electrical stimulation of the vagus nerve, has shown promise in various pain-related conditions. While further research is needed to determine its effectiveness specifically in TMJ disorder, it opens up possibilities for potential new treatment modalities.
Exploring the interplay between the vagus nerve and TMJ pain is a fascinating area of research. The vagus nerve has been found to release neurotransmitters, such as acetylcholine and gamma-aminobutyric acid (GABA), which are involved in pain modulation. By stimulating the vagus nerve, it may be possible to activate these neurotransmitters and dampen the perception of pain in individuals with TMJ disorder.
Furthermore, the vagus nerve’s role in regulating inflammation adds another layer of complexity to the relationship between the nerve and TMJ pain. Inflammation is a common feature of TMJ disorder, contributing to pain and discomfort. The vagus nerve’s anti-inflammatory properties may help mitigate the inflammatory response in the jaw joint, potentially providing relief for individuals suffering from TMJ-related symptoms.
While vagus nerve stimulation shows promise as a potential treatment for TMJ disorder, it is important to note that it is still in the early stages of investigation. Further research is needed to determine the optimal parameters for stimulation, the long-term effects, and its efficacy in different patient populations. However, the potential of this approach offers hope for individuals seeking alternative treatments for their TMJ symptoms.
Potential Therapies Targeting the Vagus Nerve
The vagus nerve, also known as the tenth cranial nerve, is a crucial component of the parasympathetic nervous system. It plays a vital role in regulating various bodily functions, including heart rate, digestion, and inflammation. In recent years, researchers have been exploring the potential of vagus nerve stimulation as a treatment for various medical conditions, such as epilepsy and treatment-resistant depression.
While its specific application for TMJ disorder is still being explored, initial studies have shown promising results. TMJ disorder, also known as temporomandibular joint disorder, is a condition that affects the jaw joint and surrounding muscles. It can cause pain, difficulty in jaw movement, and even headaches. The use of vagus nerve stimulation in TMJ disorder aims to modulate pain perception, reduce inflammation, and restore balance in the nervous system, potentially providing relief for individuals with this condition.
Vagus Nerve Stimulation as a Treatment for TMJ
TMJ disorder can significantly impact an individual’s quality of life, affecting their ability to eat, speak, and even sleep comfortably. Traditional treatment approaches for TMJ disorder include physical therapy, pain medications, and in severe cases, surgery. However, these treatments may not always provide long-term relief.
Vagus nerve stimulation, on the other hand, offers a novel approach to managing TMJ disorder. By delivering electrical impulses to the vagus nerve, this therapy aims to regulate the neural activity associated with TMJ disorder. The electrical impulses can help modulate the perception of pain, reduce inflammation in the jaw joint, and restore a sense of balance in the nervous system.
Research studies have shown that vagus nerve stimulation can lead to significant improvements in TMJ symptoms, including reduced pain intensity, improved jaw mobility, and decreased frequency of headaches. This non-invasive treatment option has garnered attention from both patients and healthcare providers, offering hope for those who have been struggling with TMJ disorder.
The Future of Vagus Nerve Therapies for TMJ Disorder
As researchers continue to deepen their understanding of the vagus nerve and its role in TMJ disorder, new treatment approaches may emerge. The field of vagus nerve therapies for TMJ disorder is still in its early stages, but the potential is vast.
One area of research focuses on optimizing the parameters of vagus nerve stimulation to maximize its therapeutic effects. By fine-tuning the intensity, frequency, and duration of the electrical impulses, researchers hope to achieve even better outcomes for individuals with TMJ disorder.
Another avenue of exploration is the development of targeted drug therapies that can specifically modulate the vagus nerve’s activity. These medications could potentially enhance the effects of vagus nerve stimulation or be used as an alternative treatment option for individuals who are not suitable candidates for electrical stimulation.
Furthermore, advancements in neuroimaging techniques, such as functional magnetic resonance imaging (fMRI), are allowing researchers to visualize the changes that occur in the brain and nervous system during vagus nerve stimulation. This deeper understanding of the underlying mechanisms can help refine and personalize the therapy for optimal results.
However, it is important to note that while vagus nerve therapies show promise, they may not be suitable for everyone. Each individual’s TMJ disorder is unique, and a personalized approach to treatment is crucial. It is essential for individuals with TMJ disorder to consult with their healthcare providers to determine the best course of treatment for their specific situation.
Conclusion: The Importance of the Vagus Nerve in TMJ Management
Summarizing the Vagus Nerve-TMJ Relationship
The vagus nerve’s impact on TMJ disorder highlights the intricate connections between the nervous system and musculoskeletal health. Dysfunction in the vagus nerve, particularly in the context of chronic stress and anxiety, may contribute to the development and maintenance of TMJ symptoms. Understanding this relationship opens up new avenues of research and treatment options for individuals with TMJ disorder.
The Potential for New Treatment Approaches
While there is still much to learn about the vagus nerve’s precise role in TMJ disorder, current research suggests that therapies targeting this complex cranial nerve may hold promise for future treatment interventions. However, it is crucial to approach these potential therapies with caution, ensuring that they are evidence-based and tailored to each individual’s needs. Consulting with a healthcare provider who specializes in TMJ disorders is essential to ensure appropriate diagnosis and treatment recommendations.
In conclusion, the impact of the vagus nerve on TMJ disorder is an exciting area of research that sheds light on the complex interplay between the nervous system and musculoskeletal health. While further studies are needed to fully elucidate the connection between the vagus nerve and TMJ disorder, it opens up new possibilities for potential therapies and management approaches. If you are experiencing TMJ symptoms, it is important to seek medical advice and consult with a healthcare professional who specializes in TMJ disorders to determine the best course of treatment for your individual situation.
If you’re intrigued by the profound influence of the vagus nerve on TMJ disorder and overall health, as discussed in this article, you’ll find the “My Vagus Nerve & Me Book” an invaluable resource. Dive deeper into the complexities of this remarkable nerve that orchestrates critical bodily functions and discover practical ways to stimulate it for enhanced well-being. Whether you’re looking to improve your immune system, digestion, heart rate, or mental health, this book is your guide to unlocking the secrets of one of the most sophisticated systems in the human body. Get My Vagus Nerve & Me eBook today and embark on a journey to better health.