Nausea is a common and unpleasant sensation that many of us experience at some point in our lives. It can be caused by various factors such as motion sickness, food poisoning, pregnancy, or even anxiety. While it is often associated with the stomach, recent research has shown that the vagus nerve plays a significant role in the development and regulation of nausea.
Understanding the Vagus Nerve
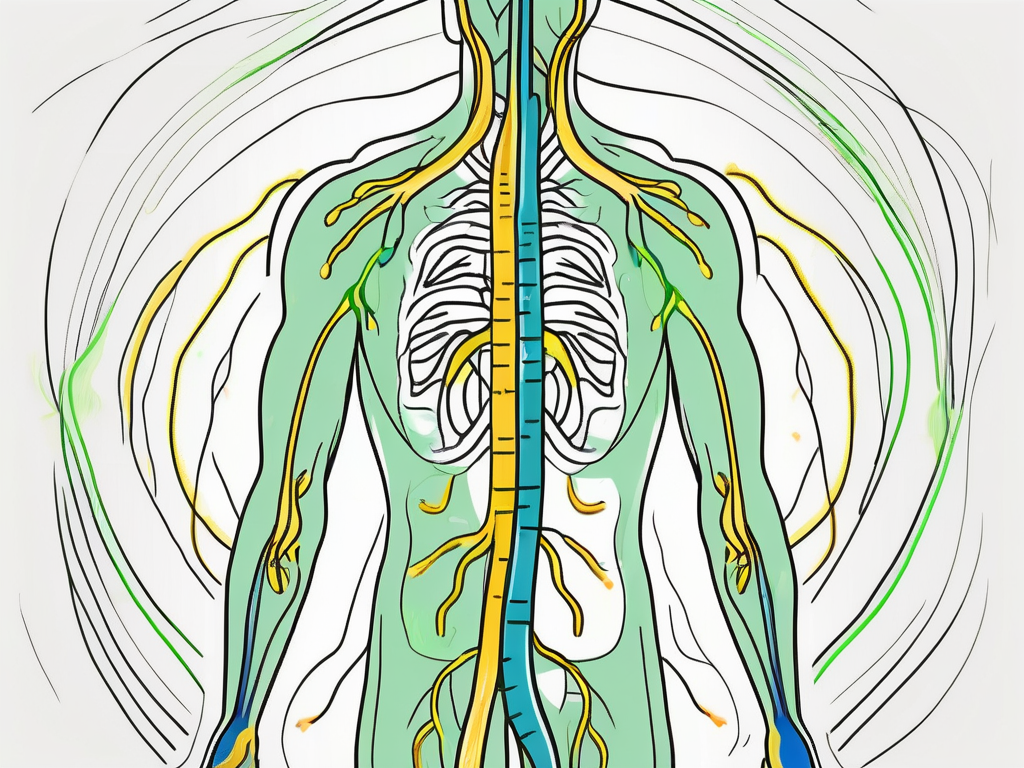
The vagus nerve, also known as the tenth cranial nerve, is one of the major nerves in the human body. It originates in the brainstem and travels down through the neck, chest, and abdomen, connecting various organs along the way. The word “vagus” actually means “wandering” in Latin, which is fitting as this nerve has a widespread reach.
As the vagus nerve makes its way through the body, it branches out and innervates several important organs. One of its primary destinations is the heart, where it helps regulate heart rate and rhythm. This intricate connection between the vagus nerve and the heart allows for precise control over cardiovascular function.
Another vital organ that the vagus nerve interacts with is the lungs. It plays a crucial role in controlling the rate and depth of breathing, ensuring a steady supply of oxygen to the body. Additionally, the vagus nerve influences the secretion of digestive enzymes in the stomach and intestines, aiding in the breakdown and absorption of nutrients.
Anatomy and Function of the Vagus Nerve
The vagus nerve is a complex network of fibers that carries signals between the brain and many vital organs, including the heart, lungs, stomach, and intestines. It has both sensory and motor functions, meaning it can transmit information from the body to the brain and vice versa. This bidirectional communication is crucial for maintaining homeostasis and controlling bodily functions.
One fascinating aspect of the vagus nerve is its involvement in the gut-brain axis. This bidirectional communication pathway between the gut and the brain is mediated by the vagus nerve, allowing for constant feedback and coordination. This connection has significant implications for mental health, as imbalances in the gut microbiome can influence mood and cognition through vagal signaling.
In addition to its role in digestion and heart rate regulation, the vagus nerve is also involved in the body’s stress response. When activated, it can lower blood pressure, reduce inflammation, and promote relaxation. This is why techniques such as deep breathing and meditation, which stimulate the vagus nerve, are often used to manage stress and anxiety.
Furthermore, the vagus nerve has been found to play a role in the regulation of appetite and metabolism. It communicates with the brain to signal feelings of fullness and satiety, helping to maintain a healthy body weight. Dysfunction of the vagus nerve can contribute to conditions such as obesity and eating disorders.
The Vagus Nerve’s Role in the Nervous System
The vagus nerve is part of the parasympathetic branch of the autonomic nervous system. This branch is responsible for promoting rest, digestion, and repair. When the body perceives a threat or stressor, the sympathetic nervous system takes over, triggering the “fight-or-flight” response. The vagus nerve helps to restore balance by counteracting the effects of stress and promoting relaxation.
Moreover, the vagus nerve is also involved in the body’s inflammatory response. It sends signals to the brain to release anti-inflammatory neurotransmitters, which help reduce inflammation and promote healing. This connection between the vagus nerve and inflammation has led to the development of novel therapies targeting this nerve for various conditions, including nausea.
Interestingly, recent research has uncovered a link between the vagus nerve and the immune system. It has been found that the vagus nerve can modulate immune responses, influencing the body’s ability to fight off infections and diseases. This discovery opens up new avenues for understanding and treating autoimmune disorders and other immune-related conditions.
In conclusion, the vagus nerve is a remarkable and intricate part of the human body. Its extensive reach and multifaceted functions make it a crucial player in maintaining overall health and well-being. Understanding the complexities of the vagus nerve can provide valuable insights into various physiological processes and potentially lead to innovative therapeutic approaches.
The Vagus Nerve and Nausea Connection
While the exact mechanisms underlying nausea are not fully understood, it is believed that the vagus nerve plays a significant role in the development of this unpleasant sensation. Studies have shown that stimulating the vagus nerve can trigger nausea, while blocking its activity can alleviate it.
How the Vagus Nerve Influences Nausea
When the body detects something potentially harmful, such as a toxin or pathogen, it activates the vagus nerve as part of its defense mechanism. This activation can lead to a cascade of events that ultimately results in symptoms of nausea. The exact pathways involved are complex and involve interactions between the brain, gut, and immune system.
One theory is that when the vagus nerve is activated, it sends signals to the brain, specifically the area known as the vomiting center, which triggers the sensation of nausea. Additionally, the vagus nerve also stimulates the release of certain neurotransmitters, such as serotonin, which have been implicated in nausea and vomiting.
Furthermore, recent research has suggested that the vagus nerve may also play a role in the regulation of gastrointestinal motility. It is thought that the nerve’s activity can influence the movement of food through the digestive system, potentially contributing to the development of nausea.
The Science Behind Vagus Nerve Stimulation and Nausea
Vagus nerve stimulation (VNS) is a therapeutic technique that involves applying electrical impulses to the vagus nerve. It has been used successfully in the treatment of various conditions, including epilepsy and depression. More recently, researchers have explored the potential of VNS in managing nausea.
Studies have shown that VNS can help alleviate symptoms of nausea by modulating the activity of the vagus nerve. By delivering electrical impulses to the nerve, it can interrupt the signal transmission related to nausea and reduce its intensity. This modulation of the vagus nerve’s activity may also have an impact on other aspects of gastrointestinal function, potentially providing additional benefits in the management of nausea.
Furthermore, researchers are investigating the potential of non-invasive methods of vagus nerve stimulation, such as transcutaneous vagus nerve stimulation (tVNS). This technique involves the application of electrical impulses to the skin overlying the vagus nerve, without the need for invasive procedures. Preliminary studies have shown promising results in the reduction of nausea symptoms using tVNS, highlighting its potential as a non-pharmacological approach to managing this discomfort.
It is important to note that while VNS and tVNS show promise in the management of nausea, further research is needed to fully understand their effectiveness and potential side effects. These techniques should only be considered under the guidance of a healthcare professional, who can assess the individual’s specific condition and determine the most appropriate course of treatment.
Potential Therapies Involving the Vagus Nerve
Given the significant role of the vagus nerve in the development of nausea, researchers have been exploring various therapies that target this nerve to provide relief to those who suffer from this unpleasant symptom.
Nausea, often accompanied by vomiting, is a common symptom experienced by individuals with various medical conditions, including migraines, gastrointestinal disorders, and chemotherapy-induced nausea. It can significantly impact a person’s quality of life and may require effective treatment options.
Non-Invasive Vagus Nerve Stimulation
Non-invasive vagus nerve stimulation (nVNS) is a technique that involves stimulating the vagus nerve using external devices, such as handheld devices or patches placed on the skin. This approach offers a safer and more accessible alternative to invasive procedures, such as surgical interventions.
nVNS works by delivering low-intensity electrical impulses to the vagus nerve, similar to VNS. These impulses can help regulate the nerve’s activity and modulate the symptoms of nausea. The electrical stimulation of the vagus nerve has been found to have a positive impact on various conditions, including epilepsy, depression, and cluster headaches.
Studies have shown that nVNS can effectively reduce the intensity and frequency of nausea episodes in individuals with different underlying causes. The convenience and ease of use of nVNS devices make them a promising option for those seeking non-pharmacological approaches to manage their symptoms.
However, it is important to note that nVNS should be used under medical supervision, and consultation with a healthcare provider is necessary before initiating any treatment. They can provide guidance on the appropriate device to use, the optimal stimulation parameters, and the expected outcomes.
Surgical Interventions and the Vagus Nerve
In certain cases where other treatments have failed, surgical interventions involving the vagus nerve may be considered. These procedures aim to modify the activity of the nerve or implant devices that can stimulate or block its signals.
One such procedure is vagus nerve decompression, where a surgeon places a small cuff around the nerve to reduce its activity. This technique has shown promising results in alleviating symptoms of various conditions, including nausea. By reducing the excessive signaling of the vagus nerve, the sensation of nausea can be significantly reduced or even eliminated.
Another surgical intervention is vagus nerve stimulation (VNS), which involves implanting a device under the skin that delivers electrical impulses to the vagus nerve. VNS has been used successfully in the treatment of epilepsy and depression, and its potential benefits in managing nausea are being explored.
While surgical interventions can offer long-term relief for individuals with severe and treatment-resistant nausea, they are not without risks. Complications such as infection, device malfunction, or nerve damage may occur. Therefore, these procedures should only be considered after a thorough evaluation and discussion with a healthcare professional.
In conclusion, therapies involving the vagus nerve, both non-invasive and surgical, hold promise in providing relief to individuals suffering from nausea. The advancements in technology and our understanding of the vagus nerve’s role in regulating various bodily functions have opened up new avenues for treatment. However, further research is needed to optimize these therapies and determine their long-term efficacy and safety.
The Future of Vagus Nerve Research
The field of vagus nerve research is rapidly evolving, and scientists are continually uncovering new insights into its role in various bodily functions, including nausea. Ongoing studies are exploring the potential of novel therapies and expanding our understanding of this fascinating connection.
Emerging Studies on the Vagus Nerve and Nausea
Recent research has shed light on specific mechanisms by which the vagus nerve influences nausea. For example, studies have identified specific receptors in the gut that are activated by vagal signals and play a role in nausea development. These receptors, known as 5-HT3 receptors, are found on the surface of cells in the gastrointestinal tract and are involved in transmitting signals related to nausea to the brain.
Furthermore, researchers have discovered that the vagus nerve communicates with the brain through a complex network of neurons and neurotransmitters. This intricate system allows the vagus nerve to transmit signals related to nausea and other bodily functions, influencing our overall well-being.
Moreover, recent studies have also explored the impact of inflammation on the vagus nerve and its role in nausea. Inflammation, which can be caused by various factors such as infection or injury, can affect the sensitivity of the vagus nerve and contribute to the development of nausea. Understanding these underlying mechanisms is crucial for developing targeted therapies that can effectively alleviate nausea.
Potential Implications for Nausea Treatment
By gaining a deeper understanding of the vagus nerve’s role in nausea, researchers are hopeful that this knowledge will translate into improved treatment options. Therapies that directly target the vagus nerve, such as Vagus Nerve Stimulation (VNS) and non-invasive Vagus Nerve Stimulation (nVNS), may provide relief to individuals who experience chronic or treatment-resistant nausea.
Additionally, researchers are exploring the potential of bioelectronic devices that can modulate the activity of the vagus nerve. These devices, which can be implanted or worn externally, deliver electrical impulses to the vagus nerve, helping to regulate its activity and potentially reduce nausea symptoms.
However, it is important to highlight that each individual is unique, and what works for one person may not work for another. Consulting with a healthcare professional is essential to determine the underlying cause of nausea and develop a tailored treatment plan. Healthcare providers can consider various factors such as the individual’s medical history, severity of symptoms, and overall health to determine the most appropriate treatment approach.
In conclusion, the link between the vagus nerve and nausea is an intriguing area of research. The vagus nerve, with its widespread connections and intricate functions, plays a substantial role in the development and regulation of nausea. Understanding the mechanisms involved and exploring innovative therapies targeting this nerve hold promise for improving the management of nausea in the future. If you are experiencing persistent or severe nausea, it is crucial to consult with a healthcare provider to receive proper evaluation and guidance.
If you’re fascinated by the role of the vagus nerve in health and want to delve deeper into its functions and how to harness its power, “My Vagus Nerve & Me Book” is the perfect resource. Discover the secrets of one of the most sophisticated systems in the human body and learn practical ways to stimulate your vagus nerve for improved well-being. From understanding its impact on your immune system to exploring its influence on digestion, heart rate, and mental health, this book covers it all. Ready to unlock the potential of your vagus nerve and enhance your quality of life? Get My Vagus Nerve & Me eBook today and embark on a journey to optimal health.