Multiple sclerosis (MS) is a complex autoimmune disease that affects the central nervous system. While the exact cause of MS remains unknown, research has increasingly focused on the role of the vagus nerve in this debilitating condition. Understanding the connection between the vagus nerve and multiple sclerosis may provide new insights into disease mechanisms and potential therapeutic approaches. In this article, we will explore the anatomy and function of the vagus nerve, its relationship with multiple sclerosis, and the broader implications of this research.
Understanding the Vagus Nerve
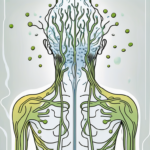
The vagus nerve, also known as cranial nerve X, is one of the longest nerves in the body. It originates in the brainstem and extends throughout the body, connecting various organs and systems. This crucial nerve plays a significant role in regulating essential bodily functions, including heart rate, digestion, and immune response.
The vagus nerve is a complex network of fibers that innervate multiple organs, allowing for bidirectional communication between the brain and these organs. It consists of both sensory and motor fibers, making it a crucial component of the autonomic nervous system. This intricate network enables constant feedback and regulation, ensuring proper functionality.
Anatomy and Function of the Vagus Nerve
The vagus nerve branches out to innervate numerous organs, such as the heart, lungs, stomach, pancreas, and intestines. Its primary function involves maintaining homeostasis by transmitting signals between these organs and the brain.
For example, when you eat a meal, the vagus nerve sends signals to the brain to initiate digestion. It stimulates the release of digestive enzymes and increases blood flow to the stomach and intestines, promoting efficient nutrient absorption.
Furthermore, the vagus nerve plays a crucial role in regulating heart rate. It acts as a brake on the heart, slowing it down when necessary. This mechanism helps maintain a steady heart rate and prevents irregularities that could lead to conditions like arrhythmia.
The Vagus Nerve and the Nervous System
Aside from its role in organ regulation, the vagus nerve also influences the overall state of the nervous system. Research suggests that it may impact neuroinflammation, the immune response within the central nervous system, and brain plasticity.
Specifically, the vagus nerve contains specialized immune cells called lymphocytes. These immune cells, along with other mediators, can modulate inflammation levels and potentially affect the progression of diseases like multiple sclerosis.
Furthermore, the vagus nerve has been linked to brain plasticity, which refers to the brain’s ability to change and adapt. Studies have shown that stimulating the vagus nerve can enhance neuroplasticity, leading to improved learning and memory abilities.
Additionally, the vagus nerve has been found to play a role in emotional regulation. It is connected to areas of the brain responsible for processing emotions, such as the amygdala and prefrontal cortex. Activation of the vagus nerve has been shown to reduce anxiety and improve mood.
In conclusion, the vagus nerve is a remarkable component of the nervous system that regulates essential bodily functions and influences overall well-being. Its intricate network of fibers connects the brain to various organs, allowing for bidirectional communication and constant regulation. Understanding the vagus nerve’s anatomy and function provides valuable insights into the complexities of the human body.
The Connection Between the Vagus Nerve and Multiple Sclerosis
Multiple sclerosis is classified as an autoimmune disease, where the immune system mistakenly attacks the protective covering of nerve fibers in the central nervous system. The exact triggers for this autoimmune response are still unclear, but emerging evidence suggests a potential role for the vagus nerve.
Multiple sclerosis affects millions of people worldwide, causing a wide range of symptoms such as fatigue, difficulty walking, numbness or weakness in limbs, and problems with coordination and balance. The disease can be unpredictable, with symptoms varying in severity and duration.
The Role of the Vagus Nerve in Autoimmune Diseases
Recent studies indicate that the vagus nerve is involved in controlling the immune system’s response to foreign substances and self-antigens. Through its communication with various organs, it can help regulate the production of pro-inflammatory and anti-inflammatory cytokines, molecules that influence immune responses.
The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body. It extends from the brainstem to various organs, including the heart, lungs, and digestive system. This extensive network allows the vagus nerve to play a crucial role in maintaining homeostasis and regulating bodily functions.
However, in cases of dysregulation, the vagus nerve may fail to adequately suppress inflammation, leading to an autoimmune response. This dysregulation can potentially contribute to the development and progression of autoimmune diseases, including multiple sclerosis.
Vagus Nerve Dysfunction in Multiple Sclerosis Patients
Researchers have found evidence of vagus nerve dysfunction in individuals with multiple sclerosis. Dysfunction can manifest as impaired vagal tone, altered signaling between the nerve and immune cells, or disruption of the bidirectional communication mentioned earlier.
Studies have shown that multiple sclerosis patients often exhibit reduced vagal tone, which refers to the activity and responsiveness of the vagus nerve. This reduced tone may result in an imbalance between pro-inflammatory and anti-inflammatory cytokines, leading to chronic inflammation and damage to nerve fibers.
Furthermore, the signaling between the vagus nerve and immune cells may be altered in multiple sclerosis patients. This disruption can affect the immune system’s ability to properly regulate inflammation and may contribute to the progression of the disease.
These vagus nerve abnormalities may contribute to the exacerbation of neuroinflammation and subsequent damage to nerve fibers seen in multiple sclerosis patients. Understanding these dysfunctions could open avenues for targeted therapeutic interventions.
Researchers are actively investigating the potential of vagus nerve stimulation as a therapeutic approach for multiple sclerosis. By modulating the activity of the vagus nerve, it may be possible to restore balance to the immune system and reduce neuroinflammation.
While the connection between the vagus nerve and multiple sclerosis is still being explored, the emerging evidence highlights the importance of understanding the intricate relationship between the nervous and immune systems. Further research in this field may lead to novel treatment strategies and improved outcomes for individuals living with multiple sclerosis.
Potential Therapeutic Approaches
The role of the vagus nerve in multiple sclerosis has prompted explorations of potential therapeutic approaches. One such approach gaining attention is vagus nerve stimulation (VNS) therapy.
The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body. It plays a crucial role in regulating various bodily functions, including heart rate, digestion, and immune response. In multiple sclerosis, the immune system mistakenly attacks the protective covering of nerve fibers, leading to communication breakdown between the brain and the rest of the body.
VNS therapy involves electrical stimulation of the vagus nerve to modulate its activity. By targeting the abnormal vagus nerve signaling observed in multiple sclerosis, this therapy aims to restore balance and regulate the immune response.
Although VNS therapy has shown promise in other conditions like epilepsy and depression, its effectiveness in multiple sclerosis is still being studied. Researchers are conducting clinical trials to evaluate its safety and efficacy in reducing disease activity and improving quality of life for individuals with multiple sclerosis. It’s important to note that VNS therapy is a medical intervention and should only be considered under the guidance and recommendation of a healthcare professional.
Vagus Nerve Stimulation Therapy: A Potential Breakthrough
VNS therapy has the potential to revolutionize the treatment landscape for multiple sclerosis. By directly influencing the vagus nerve, this therapy offers a novel approach to managing the disease.
During VNS therapy, a small device is implanted in the chest or neck, delivering electrical impulses to the vagus nerve. These impulses help regulate the immune response, reducing inflammation and preventing further damage to the central nervous system.
Early studies have shown promising results, with some individuals experiencing a decrease in relapses and a slowing of disease progression. However, more research is needed to fully understand the long-term effects and optimal parameters for VNS therapy in multiple sclerosis.
Future Directions in Vagus Nerve Research
As our understanding of the vagus nerve and its impact on multiple sclerosis deepens, ongoing research continues to explore new avenues for potential therapies. Scientists are investigating novel approaches to modulate vagal function, such as pharmacological interventions and non-invasive nerve stimulation techniques.
Pharmacological interventions aim to enhance vagal activity or target specific receptors involved in immune regulation. Researchers are exploring the potential of drugs that can selectively activate or inhibit certain vagal pathways, providing a more targeted and personalized approach to treatment.
Non-invasive nerve stimulation techniques, such as transcutaneous vagus nerve stimulation (tVNS), offer a less invasive alternative to implantable devices. These techniques involve the application of electrical currents to specific areas of the body, stimulating the vagus nerve indirectly. Early studies have shown promising results in improving symptoms and reducing disease activity in multiple sclerosis.
Additionally, advancements in neuroimaging and biomarkers may provide valuable insight into vagus nerve dysfunction and its correlation with disease progression. By identifying specific markers of vagal activity, researchers can better understand the underlying mechanisms of multiple sclerosis and develop targeted interventions.
These research efforts have the potential to pave the way for personalized treatment strategies tailored to the unique needs of individuals with multiple sclerosis. By harnessing the power of the vagus nerve, we may unlock new possibilities in managing this complex and debilitating disease.
The Broader Implications
The impact of the vagus nerve extends beyond multiple sclerosis and autoimmune diseases. Researchers are increasingly exploring the relationship between the vagus nerve and other neurological disorders.
The Vagus Nerve and Other Neurological Disorders
Emerging evidence suggests that vagus nerve dysfunction may contribute to the development or progression of conditions such as Parkinson’s disease, Alzheimer’s disease, and depression. Understanding the role of the vagus nerve in these disorders could provide novel insights and potential therapeutic targets.
For instance, studies have found that individuals with Parkinson’s disease often exhibit impaired vagal function, which may contribute to the motor symptoms associated with the condition. The vagus nerve, responsible for regulating the parasympathetic nervous system, plays a crucial role in modulating movement and coordination. Dysfunction in this nerve can disrupt the delicate balance of neurotransmitters involved in motor control, leading to the characteristic tremors and rigidity seen in Parkinson’s disease.
Similarly, research has shown a link between vagus nerve dysfunction and Alzheimer’s disease. The vagus nerve is responsible for transmitting signals between the brain and various organs, including the gut. It has been discovered that dysfunction in the vagus nerve can disrupt the communication between the brain and the gut microbiota, leading to an imbalance in gut bacteria. This imbalance, in turn, can trigger inflammation and neurodegeneration, contributing to the development and progression of Alzheimer’s disease.
In the case of depression, studies have found that individuals with depression often exhibit reduced vagal tone, indicating impaired vagus nerve function. The vagus nerve plays a crucial role in regulating the body’s stress response and emotional well-being. Dysfunction in this nerve can disrupt the release of neurotransmitters involved in mood regulation, leading to depressive symptoms.
The Vagus Nerve’s Impact on Overall Health and Well-being
Beyond its specific contributions to neurological conditions, the vagus nerve’s influence on homeostasis and immune system regulation highlights its impact on overall health and well-being. Maintaining optimal vagal function through lifestyle factors like stress management, exercise, and sleep may have broader implications for disease prevention and management.
Research has shown that chronic stress can negatively impact vagal function, leading to increased inflammation and a higher risk of developing various health conditions. On the other hand, engaging in regular physical exercise has been found to enhance vagal tone, promoting better immune function and overall well-being. Additionally, quality sleep has been associated with improved vagal function, allowing for better regulation of bodily processes and a reduced risk of developing chronic diseases.
Furthermore, the vagus nerve’s role in regulating the body’s inflammatory response is crucial for maintaining a healthy immune system. Dysfunction in the vagus nerve can lead to an overactive immune response, resulting in chronic inflammation and an increased risk of autoimmune diseases. By understanding the mechanisms through which the vagus nerve modulates inflammation, researchers can develop targeted interventions to regulate the immune system and potentially prevent or manage various diseases.
In conclusion, the vagus nerve represents a fascinating area of research regarding its impact on multiple sclerosis and other neurological conditions. Understanding the intricate connections between the vagus nerve, the immune system, and disease mechanisms is crucial for developing new therapeutic approaches. However, it’s important to note that while scientific advancements pave the way for potential treatments, seeking guidance from healthcare professionals is essential for managing individual conditions effectively.
If you’re intrigued by the profound impact of the vagus nerve on conditions like multiple sclerosis and overall health, our “My Vagus Nerve & Me Book” offers a treasure trove of information. Delve into the complexities of this remarkable nerve system that orchestrates functions from heart rate to digestion, and discover both natural and artificial methods to stimulate it for better health. Learn how to harness the power of your vagus nerve to improve immune function, mental health, and more. Get My Vagus Nerve & Me eBook today and embark on a journey to unlock the secrets of one of the body’s most essential nerves.