The Vagus Nerve, also known as the tenth cranial nerve, plays a crucial role in the function of our body. It extends from the brainstem to various organs, including the heart, lungs, and digestive system, making it a nerve with widespread connectivity. In recent times, there has been significant interest in understanding the role of the Vagus Nerve in Long COVID, a condition where individuals continue to experience symptoms long after recovering from the acute phase of the illness. This comprehensive analysis aims to explore the relationship between the Vagus Nerve and Long COVID, shedding light on its potential impact and therapeutic approaches.
Understanding the Vagus Nerve
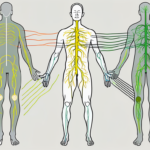
The Vagus Nerve, named after the Latin word for “wandering,” is so named because of its extensive network of branches that seem to wander throughout the body. It consists of both sensory and motor fibers that regulate various bodily functions, including heart rate, digestion, respiratory rate, and immune response. This nerve acts as a vital link between the brain and the internal organs, maintaining balance and homeostasis.
The Vagus Nerve is a fascinating and complex part of our nervous system. Let’s delve deeper into its anatomy and function to gain a better understanding of its role in our overall well-being.
Anatomy and Function of the Vagus Nerve
The Vagus Nerve originates in the medulla oblongata, the lower part of the brainstem. It extends downward and branches out into multiple smaller nerves, innervating various organs. This intricate network ensures that every organ receives the necessary signals for optimal functioning.
But what exactly do these sensory and motor fibers do? The sensory fibers transmit information from the organs to the brain, allowing us to perceive sensations such as pain, temperature, and pressure. On the other hand, the motor fibers carry signals from the brain to control organ function, ensuring that everything runs smoothly.
For example, when you eat a delicious meal, the Vagus Nerve communicates with your digestive system, triggering the release of digestive enzymes and stimulating peristalsis, the rhythmic contractions that propel food through your gastrointestinal tract. Without the Vagus Nerve, our digestive process would be disrupted, leading to various gastrointestinal issues.
Additionally, the Vagus Nerve plays a crucial role in regulating heart rate. It acts as a brake, slowing down the heart rate when it’s beating too fast. This mechanism helps maintain a steady and healthy heart rhythm, preventing conditions like tachycardia.
The Vagus Nerve and the Immune System
Beyond its involvement in maintaining organ function, the Vagus Nerve also interacts with the immune system. Research suggests that it plays a significant role in regulating the body’s inflammatory response, a vital defense mechanism against infections and injuries.
When activated, the Vagus Nerve can inhibit the production of pro-inflammatory molecules, thereby reducing inflammation. This modulation of the immune response may have broader implications for our health. For instance, in the context of Long COVID, where individuals experience persistent symptoms long after recovering from the initial infection, inflammation is known to play a role. Understanding the Vagus Nerve’s influence on inflammation could potentially lead to new therapeutic approaches for managing Long COVID and other chronic inflammatory conditions.
Furthermore, studies have shown that stimulating the Vagus Nerve through techniques like vagus nerve stimulation (VNS) can have anti-inflammatory effects. This finding opens up exciting possibilities for using VNS as a therapeutic intervention for conditions characterized by excessive inflammation, such as rheumatoid arthritis and inflammatory bowel disease.
In conclusion, the Vagus Nerve is a remarkable part of our nervous system that goes beyond its role in regulating organ function. Its influence extends to the immune system, where it modulates inflammation, opening up new avenues for medical research and potential treatments. Understanding the intricacies of the Vagus Nerve is an ongoing endeavor that promises to shed light on the complex interplay between our nervous and immune systems.
Long COVID: An Overview
Long COVID is a condition that affects individuals who have recovered from the acute phase of COVID-19 but continue to experience a range of diverse symptoms for an extended period, often lasting several months. The exact mechanisms behind Long COVID remain unclear, but its impact on individuals’ quality of life underscores the need for further investigation and understanding.
Long COVID is a complex and multifaceted condition that has garnered significant attention in recent months. As researchers and healthcare professionals delve deeper into understanding the long-term effects of COVID-19, it becomes increasingly evident that Long COVID is not a mere continuation of the acute illness, but a distinct entity with its own set of challenges and implications.
Defining Long COVID
Long COVID is characterized by persistent symptoms that go beyond the expected recovery timeframe. These symptoms can vary widely, affecting physical, cognitive, and mental health. Common manifestations include fatigue, shortness of breath, brain fog, joint pain, and depression. The heterogeneity of symptoms and their unpredictable nature present unique challenges in diagnosing and managing this condition.
While some individuals may experience a gradual improvement in their symptoms over time, others may find themselves grappling with a fluctuating pattern of symptoms that wax and wane without a clear pattern. This unpredictability can be frustrating and disheartening, as individuals struggle to regain their pre-COVID level of functioning.
Symptoms and Challenges of Long COVID
Individuals with Long COVID face numerous challenges, both physical and psychological. The persistence of symptoms can significantly impact daily life activities and overall well-being. Simple tasks that were once taken for granted, such as climbing a flight of stairs or concentrating on a task, can now become arduous and exhausting.
Moreover, the cognitive symptoms associated with Long COVID, often referred to as “brain fog,” can have a profound impact on an individual’s ability to think clearly and perform complex mental tasks. This can affect their professional life, making it difficult to return to work or maintain productivity.
The psychological toll of Long COVID should not be underestimated. Many individuals with Long COVID experience feelings of frustration, anxiety, and depression as they navigate the uncertainties of their condition. The lack of a standardized diagnostic criteria and treatment protocol poses additional hurdles in managing the condition effectively. It is essential for healthcare providers to carefully listen to patients, assess their symptoms, and provide appropriate support and guidance.
As the medical community continues to learn more about Long COVID, efforts are being made to establish comprehensive care pathways and support networks for individuals affected by this condition. Research studies are underway to investigate potential treatments and interventions that can alleviate symptoms and improve quality of life.
In conclusion, Long COVID is a complex and challenging condition that requires a multidisciplinary approach for effective management. By acknowledging the diverse range of symptoms and the impact they have on individuals’ lives, healthcare providers can offer the necessary support and guidance to help patients navigate the uncertainties of Long COVID.
The Vagus Nerve’s Role in Long COVID
In recent studies, the potential involvement of the Vagus Nerve in Long COVID has been explored. Given its extensive reach and influence over various bodily functions, it is plausible that dysregulation of the Vagus Nerve may contribute to the persistence of symptoms in some individuals.
The Vagus Nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It originates in the brainstem and branches out to innervate multiple organs, including the heart, lungs, digestive system, and immune system. This widespread distribution allows the Vagus Nerve to play a crucial role in regulating various physiological processes.
The Vagus Nerve and Inflammation
One possible mechanism through which the Vagus Nerve may affect Long COVID is by its modulation of inflammation. Inflammatory processes are integral in the body’s response to infection, but in some cases, this response can become dysregulated and lead to prolonged inflammation.
The Vagus Nerve possesses a unique ability to dampen inflammation through a process known as the cholinergic anti-inflammatory pathway. When activated, the Vagus Nerve releases neurotransmitters, such as acetylcholine, that inhibit the production of pro-inflammatory molecules. This anti-inflammatory effect helps restore balance and resolve the immune response.
In individuals with Long COVID, however, the Vagus Nerve’s ability to regulate inflammation may be compromised. This dysregulation could result in a persistent state of inflammation, contributing to the chronic nature of the condition. Further research is needed to elucidate the exact mechanisms and potential therapeutic implications of Vagus Nerve dysfunction in Long COVID.
Neurological Symptoms and the Vagus Nerve
Neurological symptoms, such as brain fog and cognitive impairment, are prevalent in Long COVID. These symptoms can significantly impact an individual’s quality of life and daily functioning.
The Vagus Nerve has connections with multiple brain regions involved in cognition and memory, including the hippocampus and prefrontal cortex. These connections suggest a possible link between Vagus Nerve dysfunction and the neurological symptoms observed in Long COVID.
Research has shown that the Vagus Nerve plays a role in regulating neuroinflammation, neurogenesis, and synaptic plasticity, all of which are crucial for cognitive function. Dysfunction of the Vagus Nerve may disrupt these processes, leading to cognitive impairments and the characteristic brain fog experienced by individuals with Long COVID.
Understanding the intricacies of the relationship between the Vagus Nerve and neurological symptoms in Long COVID is crucial for developing targeted interventions that address the cognitive manifestations of the condition. By targeting Vagus Nerve function, researchers and clinicians may be able to alleviate cognitive impairments and improve the overall well-being of individuals affected by Long COVID.
Therapeutic Approaches Targeting the Vagus Nerve
Given the potential involvement of the Vagus Nerve in Long COVID, researchers have explored various therapeutic approaches aimed at modulating its activity.
The Vagus Nerve, also known as the tenth cranial nerve, is a vital component of the autonomic nervous system. It plays a crucial role in regulating various bodily functions, including heart rate, digestion, and immune response. Dysfunction of the Vagus Nerve has been implicated in several health conditions, including Long COVID.
Vagus Nerve Stimulation Techniques
One approach involves the use of Vagus Nerve Stimulation (VNS) techniques. VNS involves the use of electrical impulses to stimulate the Vagus Nerve and regulate its activity. This technique has shown promise in various conditions, including epilepsy and depression.
During VNS, a small device is surgically implanted in the chest or neck area, and it delivers electrical impulses to the Vagus Nerve at regular intervals. These impulses help to restore the balance of the autonomic nervous system and promote overall well-being.
While studies exploring the application of VNS in Long COVID are limited, early results are encouraging, and further research is ongoing. Researchers are investigating the potential of VNS to alleviate the symptoms of Long COVID, such as fatigue, brain fog, and shortness of breath. Preliminary findings suggest that VNS may help improve these symptoms and enhance the overall quality of life for individuals with Long COVID.
Potential Benefits and Risks
It is important to note that any therapeutic intervention carries potential benefits and risks. While Vagus Nerve modulation techniques may offer relief to some individuals with Long COVID, it is essential to consult with a healthcare professional to thoroughly evaluate the potential benefits and risks on a case-by-case basis.
Medical guidance and monitoring are crucial to ensure safety and effectiveness. Healthcare professionals will assess the individual’s medical history, current health status, and specific symptoms to determine the suitability of Vagus Nerve stimulation techniques. They will also provide detailed information about the procedure, potential side effects, and long-term outcomes.
While VNS is generally considered safe, there are potential risks associated with the surgical implantation of the device and the delivery of electrical impulses. These risks include infection, bleeding, hoarseness, and difficulty swallowing. However, healthcare professionals will carefully evaluate the individual’s overall health and discuss the potential risks and benefits to make an informed decision.
Furthermore, it is crucial to understand that Vagus Nerve stimulation techniques are not a standalone treatment for Long COVID. They are part of a comprehensive approach that may include other therapies, such as medication, physical therapy, and lifestyle modifications.
In conclusion, therapeutic approaches targeting the Vagus Nerve, such as Vagus Nerve Stimulation techniques, hold promise in the management of Long COVID. However, it is essential to consult with healthcare professionals to determine the suitability of these techniques and to ensure comprehensive care and monitoring throughout the treatment process.
Future Research Directions
Despite the progress made in understanding Long COVID and the potential role of the Vagus Nerve, there are still many unanswered questions that need to be addressed through further research.
Unanswered Questions about the Vagus Nerve and Long COVID
Researchers are actively investigating various aspects concerning the relationship between the Vagus Nerve and Long COVID. Some questions that remain to be answered include the specific mechanisms linking Vagus Nerve dysfunction to Long COVID symptoms, the factors that determine individual susceptibility to Vagus Nerve dysregulation, and the effectiveness of different therapeutic interventions in managing Long COVID.
One area of interest is understanding the intricate connections between the Vagus Nerve and the immune response. While it is known that the Vagus Nerve plays a role in regulating inflammation, further research is needed to determine how this regulation is disrupted in individuals with Long COVID. By unraveling the specific mechanisms involved, researchers hope to develop targeted interventions that can modulate the Vagus Nerve and restore immune balance.
Another unanswered question is why certain individuals are more susceptible to Vagus Nerve dysregulation and subsequently develop Long COVID symptoms. Factors such as genetic predisposition, pre-existing health conditions, and environmental influences may all play a role. By identifying these factors, researchers can better understand individual susceptibility and develop personalized treatment approaches.
Additionally, the effectiveness of different therapeutic interventions in managing Long COVID remains uncertain. While some studies have shown promising results with Vagus Nerve stimulation techniques, such as transcutaneous vagus nerve stimulation (tVNS), more research is needed to determine the optimal parameters and protocols for these interventions. Furthermore, exploring other potential therapeutic targets within the domain of Vagus Nerve modulation may provide additional avenues for managing Long COVID symptoms.
The Path Forward for Vagus Nerve Research
As the understanding of Long COVID and the Vagus Nerve deepens, future research will focus on unraveling the intricate connections between the Vagus Nerve and immune response, further elucidating the role of Vagus Nerve modulation in managing Long COVID symptoms, and exploring potential novel therapeutic targets within this domain. Collaborative efforts across disciplines will be crucial in advancing our knowledge and developing effective interventions for individuals with Long COVID.
Researchers are also interested in exploring the bidirectional relationship between the Vagus Nerve and the central nervous system. The Vagus Nerve is known to communicate bidirectionally with various regions of the brain, including those involved in pain processing and emotional regulation. Understanding how Vagus Nerve dysfunction affects these brain regions in individuals with Long COVID may provide insights into the neurological symptoms experienced by some patients.
Furthermore, investigating the role of Vagus Nerve modulation in managing Long COVID symptoms is a priority for future research. By understanding how Vagus Nerve stimulation techniques, such as tVNS, can alleviate symptoms like fatigue, brain fog, and dysautonomia, researchers can develop evidence-based treatment protocols that improve the quality of life for individuals with Long COVID.
In conclusion, the impact of the Vagus Nerve on Long COVID is an area of ongoing investigation and continues to yield valuable insights. The bidirectional relationship between the Vagus Nerve and various bodily systems, including the immune system and the central nervous system, opens up avenues for potential therapeutic approaches. However, it is important to approach this information with caution and consult with healthcare professionals for guidance and support tailored to individual circumstances. With further research and collaboration, we can hope to provide better understanding and management strategies for individuals navigating the challenges posed by Long COVID.
If you’re fascinated by the crucial role the Vagus Nerve plays in your health and are eager to dive deeper into its functions and therapeutic potential, especially in the context of Long COVID, “My Vagus Nerve & Me Book” is an essential resource. This comprehensive guide will enlighten you on the intricacies of one of the most complex systems in the human body. You’ll discover natural and artificial ways to stimulate your Vagus Nerve, enhancing your well-being across various bodily systems. Don’t miss the opportunity to unlock the secrets of your Vagus Nerve and harness its power for your health. Get My Vagus Nerve & Me eBook today and take the first step towards understanding and optimizing this vital aspect of your physiology.