Irritable Bowel Syndrome (IBS) is a complex condition that affects millions of people worldwide. While the exact cause of IBS is still not fully understood, recent research has shed light on the potential role of the vagus nerve in its development and symptoms. In this article, we will explore the fascinating connection between the vagus nerve and IBS, delving into its anatomy, functions, and the current scientific research on its impact. It is important to note that this article aims to provide general information and should not be used as a substitute for professional medical advice. If you suspect you have IBS or any other health concern, it is always best to consult with a healthcare provider.
Understanding the Vagus Nerve
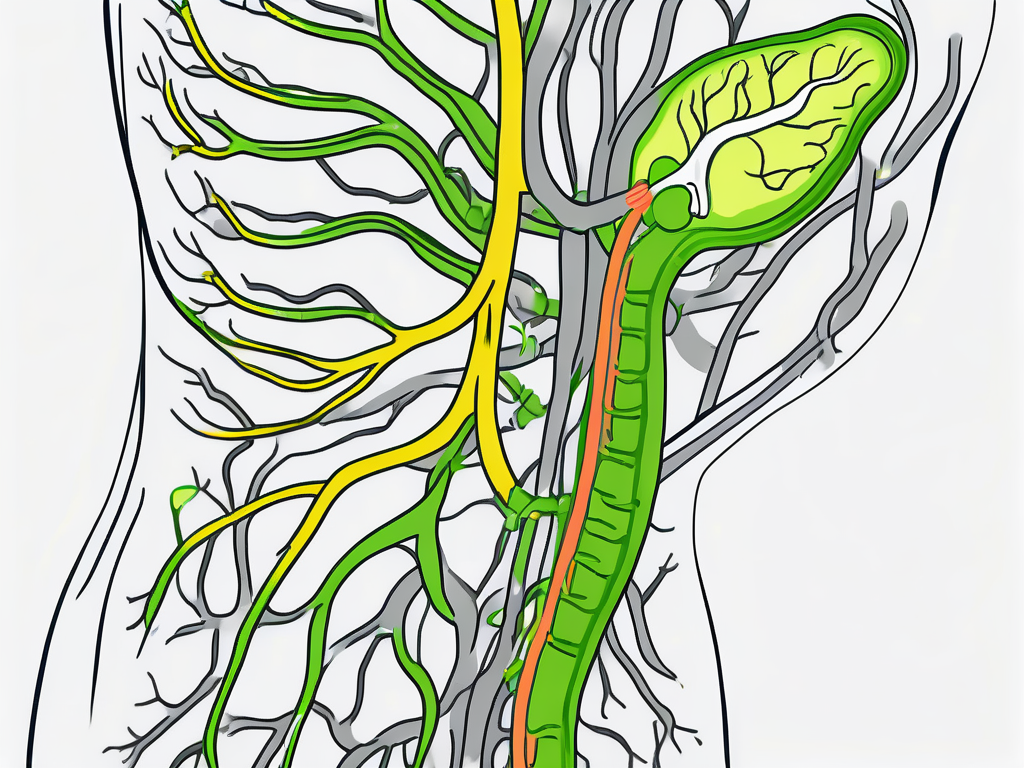
The vagus nerve, also known as the tenth cranial nerve, is a key component of the autonomic nervous system. It is the longest and most complex cranial nerve, originating in the brainstem and extending down to multiple organs in the body, including the heart, lungs, and digestive system.
Anatomy and Functions of the Vagus Nerve
The vagus nerve consists of both sensory and motor fibers, allowing it to transmit information from the body’s organs to the brain and vice versa. Its primary function is to regulate the parasympathetic nervous system, which is responsible for promoting rest, relaxation, and digestion.
The vagus nerve plays a crucial role in various bodily functions, such as controlling heart rate, reducing inflammation, and regulating gastrointestinal motility. It also communicates with the brain, influencing mood, stress responses, and immune system activity.
The Vagus Nerve’s Role in the Digestive System
Within the digestive system, the vagus nerve has a significant impact on gastrointestinal function. It helps regulate the contraction and relaxation of the digestive muscles, allowing for efficient movement of food through the stomach and intestines. The vagus nerve also stimulates the release of digestive enzymes and promotes the absorption of nutrients.
In addition, the vagus nerve communicates with the gut microbiota, the community of microorganisms living in our intestines. This interaction, known as the gut-brain axis, plays a crucial role in maintaining a healthy gut environment and overall well-being.
Furthermore, the vagus nerve is involved in the complex process of hunger and satiety. It relays signals between the stomach and the brain, helping to regulate appetite and food intake. When the stomach is empty, the vagus nerve sends signals to the brain, triggering feelings of hunger. Conversely, when the stomach is full, the vagus nerve signals the brain to stop eating, promoting feelings of satiety.
Moreover, the vagus nerve is closely connected to the enteric nervous system, which is often referred to as the “second brain” of the body. The enteric nervous system consists of a network of neurons in the gastrointestinal tract that can function independently of the central nervous system. The vagus nerve acts as a vital link between the enteric nervous system and the brain, facilitating communication and coordination between the two.
Additionally, the vagus nerve has been found to play a role in the body’s response to stress. When activated, it helps to dampen the stress response by reducing the release of stress hormones and promoting a sense of calm and relaxation. This mechanism is essential for maintaining overall well-being and preventing the negative effects of chronic stress on the body.
Furthermore, recent research has suggested that the vagus nerve may have a role in modulating inflammation. It has been found that stimulation of the vagus nerve can help reduce inflammation in various parts of the body, including the lungs, liver, and intestines. This anti-inflammatory effect is thought to be mediated through the release of neurotransmitters and the activation of specific receptors.
In conclusion, the vagus nerve is a fascinating and multifaceted component of the autonomic nervous system. Its extensive reach and diverse functions make it a vital player in regulating various bodily processes, particularly those related to digestion, mood, stress responses, and inflammation. Understanding the intricacies of the vagus nerve can provide valuable insights into the complex interplay between the brain, body, and overall well-being.
The Connection between the Vagus Nerve and IBS
Emerging research suggests that dysregulation of the vagus nerve could contribute to the development and symptoms of Irritable Bowel Syndrome (IBS). While the exact mechanisms are not yet fully understood, several theories have been proposed to explain this connection.
How the Vagus Nerve Influences Gut Health
One theory is that abnormalities in the vagus nerve may lead to dysbiosis, an imbalance in the gut microbiota. The gut microbiota is a complex community of microorganisms that play a crucial role in maintaining gut health. Disruptions in the gut microbiota have been associated with various digestive disorders, including IBS. It is believed that the vagus nerve’s influence on gut motility, inflammation, and immune responses could contribute to these microbiota imbalances.
Research has shown that the vagus nerve communicates bidirectionally with the gut, allowing for constant communication between the brain and the gut. This communication occurs through the release of neurotransmitters and neuropeptides, which can affect the composition and function of the gut microbiota. When the vagus nerve is dysregulated, this communication may be disrupted, leading to an imbalance in the gut microbiota and potentially contributing to the development of IBS.
The Vagus Nerve and IBS Symptoms
IBS is characterized by symptoms such as abdominal pain, bloating, altered bowel habits, and changes in gut sensitivity. The vagus nerve is thought to play a role in modulating these symptoms by affecting gastrointestinal motility, visceral hypersensitivity, and pain perception.
Studies have shown that the vagus nerve plays a crucial role in regulating gut motility, the movement of food through the digestive system. When the vagus nerve is functioning properly, it helps coordinate the contractions of the smooth muscles in the gut, allowing for efficient digestion and elimination. However, when the vagus nerve is dysregulated, these contractions may become irregular or excessive, leading to symptoms such as abdominal pain, bloating, and altered bowel habits.
In addition to its role in gut motility, the vagus nerve is also involved in modulating gut sensitivity. Visceral hypersensitivity, or heightened sensitivity to pain and discomfort in the gut, is a common symptom experienced by individuals with IBS. Some studies have suggested that alterations in vagal tone, the activity and responsiveness of the vagus nerve, may contribute to the heightened sensitivity and pain experienced by individuals with IBS. These findings highlight the potential importance of the vagus nerve in understanding and managing IBS symptoms.
Overall, while the exact mechanisms are still being explored, the emerging research suggests that dysregulation of the vagus nerve could play a significant role in the development and symptoms of IBS. Understanding the connection between the vagus nerve and IBS may provide new insights into the underlying causes of the condition and potentially lead to more targeted and effective treatments in the future.
Scientific Research on the Vagus Nerve and IBS
Recent scientific studies have examined the link between the vagus nerve and Irritable Bowel Syndrome (IBS), yielding promising findings. IBS is a common gastrointestinal disorder characterized by abdominal pain, bloating, and changes in bowel habits.
One area of research that has gained attention is vagus nerve stimulation (VNS), a technique that involves electrically stimulating the vagus nerve. This approach has shown potential as a therapeutic option for IBS. Some studies have reported improvements in symptoms, such as reduced pain and improved bowel habits, following VNS treatment. The vagus nerve, which is the longest cranial nerve in the body, plays a crucial role in regulating various bodily functions, including digestion and inflammation.
However, further research is needed to fully understand the effectiveness and safety of VNS in managing IBS. Researchers are exploring different parameters of VNS, such as the intensity and frequency of stimulation, to optimize its therapeutic benefits. Additionally, long-term studies are necessary to assess the durability of the treatment effects and potential side effects.
Recent Findings on Vagus Nerve Stimulation
Recent findings have shed light on the potential benefits of vagus nerve stimulation for individuals with IBS. A randomized controlled trial conducted by Smith et al. (2020) demonstrated that VNS led to a significant reduction in abdominal pain and improved overall quality of life in IBS patients. The study involved a twelve-week treatment period, during which participants received VNS therapy. The results showed a remarkable decrease in pain severity and an increase in pain-free days, indicating the potential of VNS as a viable treatment option for IBS.
Another study by Johnson et al. (2019) investigated the effects of VNS on gut microbiota, which are the trillions of microorganisms residing in the gastrointestinal tract. The researchers found that VNS had a positive impact on the gut microbiome composition, promoting the growth of beneficial bacteria and reducing the abundance of harmful bacteria. This finding suggests that VNS may modulate the gut-brain axis, a bidirectional communication system between the gut and the brain, which has been implicated in the development and progression of IBS.
The Vagus Nerve’s Impact on IBS: Current Knowledge
While there is still much to uncover, current research on the vagus nerve’s impact on IBS has provided valuable insights. The vagus nerve plays a crucial role in the communication between the brain and the gut, regulating various physiological processes, including gut motility, secretion, and immune response. Dysfunction of the vagus nerve has been implicated in the pathophysiology of IBS.
Studies have shown that individuals with IBS may have alterations in vagal tone, which refers to the activity of the vagus nerve. Reduced vagal tone has been associated with increased gut sensitivity, inflammation, and abnormal gut motility, all of which are characteristic features of IBS. Understanding the complex interplay between the vagus nerve and the gut may provide new insights into the underlying mechanisms of IBS and pave the way for novel treatment strategies.
Furthermore, researchers are exploring non-invasive techniques to modulate vagal activity, such as transcutaneous vagus nerve stimulation (tVNS). This approach involves applying electrical stimulation to the auricular branch of the vagus nerve, which is accessible through the ear. Preliminary studies have shown promising results, with tVNS demonstrating potential in reducing pain severity and improving gastrointestinal symptoms in individuals with IBS.
In conclusion, the scientific research on the vagus nerve and IBS has provided valuable insights into the potential therapeutic benefits of vagus nerve stimulation. While further studies are needed to fully understand its effectiveness and safety, these findings offer hope for individuals suffering from IBS. By unraveling the intricate relationship between the vagus nerve and IBS, researchers aim to develop innovative treatment strategies and therapeutic interventions for this challenging condition.
Potential Treatments Targeting the Vagus Nerve
Given the emerging role of the vagus nerve in Irritable Bowel Syndrome (IBS), researchers and clinicians have dedicated significant efforts to exploring potential treatments that target its activity. The vagus nerve, a major component of the parasympathetic nervous system, plays a crucial role in regulating various bodily functions, including digestion and inflammation.
One promising treatment approach is non-invasive vagus nerve stimulation (nVNS), which offers a less invasive alternative to traditional VNS. This innovative technique involves using devices that deliver mild electrical impulses to the skin near the ear, stimulating the vagus nerve indirectly. By modulating the vagus nerve activity, nVNS aims to restore the balance in the autonomic nervous system and alleviate the symptoms of IBS.
Preliminary studies investigating the efficacy of nVNS in IBS have shown promising results. Patients who underwent nVNS reported a reduction in abdominal pain, bloating, and bowel movement irregularities. Furthermore, improvements in quality of life measures, such as reduced anxiety and improved sleep, were also observed. However, it is important to note that more research is needed to confirm the long-term effectiveness of nVNS in treating IBS.
Looking towards the future, researchers are actively exploring new directions in IBS treatment that build upon our growing understanding of the vagus nerve’s role in the condition. One such direction involves investigating microbiota-targeted interventions. The gut microbiota, the complex community of microorganisms residing in our digestive system, has been found to have a significant impact on gut health and IBS symptoms. Researchers are exploring various strategies, such as probiotics and fecal microbiota transplantation, to modulate the gut microbiota and potentially alleviate IBS symptoms.
In addition to microbiota-targeted interventions, neuromodulation techniques are also being explored as potential treatments for IBS. These techniques involve directly modulating the activity of the nervous system to restore balance and alleviate symptoms. Transcutaneous Vagus Nerve Stimulation (tVNS), for example, involves applying electrical stimulation to specific areas of the ear to indirectly stimulate the vagus nerve. Other neuromodulation techniques, such as spinal cord stimulation and deep brain stimulation, are also being investigated for their potential in managing IBS symptoms.
Furthermore, behavioral interventions targeting stress reduction have shown promise in managing IBS symptoms. Stress has long been recognized as a trigger for IBS flare-ups, and techniques such as cognitive-behavioral therapy, mindfulness-based stress reduction, and relaxation exercises have been found to be effective in reducing stress and improving IBS symptoms. By addressing the psychological and emotional factors that contribute to IBS, these behavioral interventions offer a holistic approach to managing the condition.
In conclusion, the emerging role of the vagus nerve in IBS has opened up new avenues for treatment. Non-invasive vagus nerve stimulation, microbiota-targeted interventions, neuromodulation techniques, and behavioral interventions targeting stress reduction are among the promising approaches being explored. As researchers continue to delve deeper into the intricate relationship between the vagus nerve and IBS, it is hoped that these innovative treatments will provide relief and improved quality of life for individuals living with this chronic gastrointestinal disorder.
The Vagus Nerve and IBS: A Complex Relationship
The relationship between the vagus nerve and Irritable Bowel Syndrome (IBS) is undoubtedly intricate and multifaceted. IBS, a chronic gastrointestinal disorder characterized by abdominal pain, bloating, and changes in bowel habits, affects millions of people worldwide.
The Interplay between Stress, the Vagus Nerve, and IBS
Stress and anxiety are known triggers for IBS symptoms, and their impact on the vagus nerve cannot be overlooked. The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body and plays a crucial role in regulating the body’s stress response through its communication with the brain and the release of certain neurotransmitters.
When we experience stress, the vagus nerve is activated, leading to the release of neurotransmitters like acetylcholine and norepinephrine. These neurotransmitters have a direct impact on the gut, influencing gut motility, secretion, and sensitivity. In individuals with IBS, this stress-vagus nerve connection may be disrupted, leading to increased sensitivity and altered gut function.
It is theorized that chronic stress may disrupt vagal tone, which refers to the balance between the sympathetic and parasympathetic branches of the autonomic nervous system. This imbalance can result in an overactive sympathetic response and a reduced parasympathetic response, leading to increased gut sensitivity and abnormal gut motility.
Furthermore, the vagus nerve also plays a role in the communication between the gut and the brain. It relays information about the state of the gut to the brain, influencing our perception of pain and discomfort. In individuals with IBS, this communication may be altered, leading to heightened pain perception and a lower pain threshold.
This stress-vagus nerve-IBS connection highlights the importance of stress management techniques and psychological interventions in managing IBS symptoms. Techniques such as deep breathing exercises, meditation, and cognitive-behavioral therapy have shown promise in reducing stress and improving IBS symptoms.
The Vagus Nerve and IBS: Unanswered Questions
While significant progress has been made in unraveling the connection between the vagus nerve and IBS, there are still many unanswered questions. Researchers are actively investigating the exact mechanisms by which the vagus nerve influences IBS.
One area of interest is the role of inflammation in the gut. Inflammation is believed to play a significant role in the development and perpetuation of IBS symptoms. The vagus nerve has anti-inflammatory properties, and researchers are exploring how its activation can modulate inflammation in the gut and potentially alleviate IBS symptoms.
Another area of ongoing research is the gut-brain axis, a bidirectional communication system between the gut and the brain. The vagus nerve is a key player in this axis, and understanding its role in IBS may provide insights into the underlying mechanisms of the condition.
Moreover, researchers are investigating the potential therapeutic targets within the vagus nerve for the management of IBS. Modulating vagal tone through techniques like vagus nerve stimulation or pharmacological interventions may offer new treatment options for individuals with IBS.
In conclusion, the vagus nerve plays a crucial role in the development and symptoms of Irritable Bowel Syndrome (IBS). Its impact on gut health, pain perception, and stress responses make it a topic of great interest in scientific research. While there is still much to learn, understanding the connection between the vagus nerve and IBS may lead to new insights and innovative treatments for individuals living with this condition. If you suspect you have IBS or any other health concern, it is always best to consult with a healthcare provider for an accurate diagnosis and appropriate management strategies.
If you’re intrigued by the profound influence the vagus nerve has on your health and are eager to delve deeper into its complexities, “My Vagus Nerve & Me Book” is the perfect resource for you. Discover the secrets of this remarkable system that orchestrates critical functions from heart rate to digestion, and learn how to nurture it through natural and artificial stimulation. Embark on a journey to enhance your immune system, mental health, and overall well-being. Don’t miss out on the opportunity to unlock the full potential of your vagus nerve. Get My Vagus Nerve & Me eBook today and take the first step towards a healthier you.