Gastroesophageal reflux disease (GERD) affects millions of people worldwide, causing uncomfortable symptoms and impacting their quality of life. In recent years, researchers have been exploring the connection between GERD and the vagus nerve, a crucial component of our autonomic nervous system. Understanding the role of the vagus nerve in GERD could potentially lead to new and effective treatments for this prevalent condition.
Understanding the Vagus Nerve
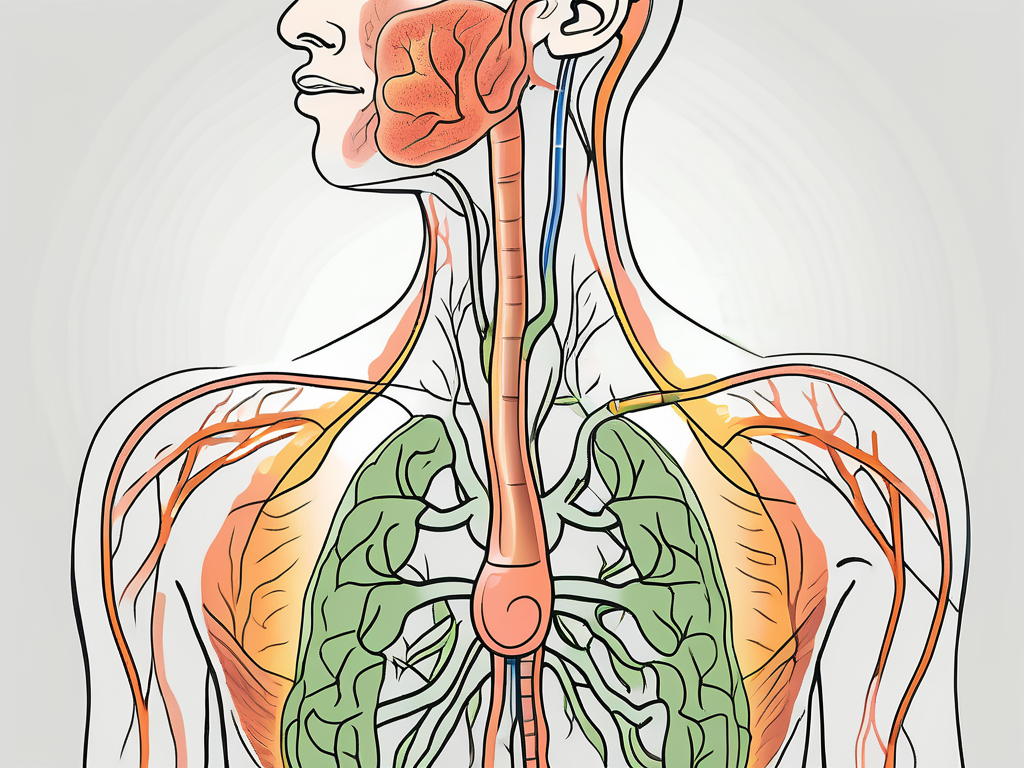
The vagus nerve, also known as the 10th cranial nerve, is a long and complex nerve that extends from the brainstem down into the abdomen, innervating multiple organs along the way. It is responsible for regulating various bodily functions, including heart rate, digestion, and even mood. To comprehend the connection between the vagus nerve and GERD, it is essential to grasp the anatomy and function of this intriguing nerve.
Anatomy and Function of the Vagus Nerve
The vagus nerve consists of afferent and efferent fibers, meaning it carries both sensory information from the body to the brain and motor commands from the brain to the body. The afferent fibers transmit signals from organs such as the heart, lungs, and gastrointestinal tract to the brain, while the efferent fibers relay instructions from the brain to the muscles and organs.
But what exactly does this mean for the vagus nerve’s role in regulating bodily functions? Let’s dive deeper into its anatomy and function.
First, let’s explore the afferent fibers of the vagus nerve. These fibers are responsible for transmitting sensory information from various organs to the brain. For example, when you eat a delicious meal, the vagus nerve’s afferent fibers send signals to the brain, letting it know that you are satisfied and full. This communication helps regulate your appetite and prevents overeating.
Now, let’s shift our focus to the efferent fibers of the vagus nerve. These fibers carry motor commands from the brain to the muscles and organs, allowing the brain to control bodily functions. One of the most crucial functions regulated by the vagus nerve is heart rate. Through its efferent fibers, the vagus nerve can slow down or speed up the heart rate, maintaining a steady rhythm and ensuring optimal cardiovascular health.
Additionally, the vagus nerve plays a vital role in maintaining balance within the body, known as homeostasis. It helps regulate heart rate, blood pressure, and breathing, ensuring that these essential functions remain within optimal parameters. Moreover, the vagus nerve influences digestion, another area where its impact on GERD becomes evident.
The Vagus Nerve’s Role in Digestion
When it comes to digestion, the vagus nerve acts as a crucial communicator between the brain and the gastrointestinal system. It regulates the release of digestive enzymes, controls the movement of food through the intestinal tract, and even influences the perception of hunger and fullness.
Imagine sitting down to a delicious meal. As you take your first bite, the vagus nerve sends signals to your brain, triggering the release of digestive enzymes in your stomach. These enzymes help break down the food, allowing for proper absorption of nutrients. The vagus nerve also controls the movement of food through the intestinal tract, ensuring that it progresses smoothly and efficiently.
But what happens if the vagus nerve’s regulation of digestion goes awry? This is where the connection between the vagus nerve and GERD becomes significant.
One aspect of digestion that the vagus nerve influences is the lower esophageal sphincter (LES), a muscle that separates the esophagus from the stomach. Normally, the LES acts as a valve, opening to allow food and fluids to pass into the stomach and closing to prevent stomach acid from flowing back up into the esophagus. If the vagus nerve fails to regulate the LES properly, it may result in the development of GERD.
GERD, or gastroesophageal reflux disease, occurs when stomach acid flows back into the esophagus, causing symptoms such as heartburn, regurgitation, and chest pain. The vagus nerve’s role in controlling the LES’s function is crucial in preventing this backflow of stomach acid. When the vagus nerve fails to properly regulate the LES, it can lead to the weakening of the muscle, allowing stomach acid to escape into the esophagus and causing the uncomfortable symptoms associated with GERD.
Understanding the intricate relationship between the vagus nerve and GERD highlights the importance of maintaining optimal vagal tone and function. By supporting the health of the vagus nerve through various lifestyle choices, such as stress management techniques, regular exercise, and a balanced diet, individuals can potentially reduce their risk of developing GERD and other digestive disorders.
Gastroesophageal Reflux Disease (GERD) Explained
Gastroesophageal reflux disease, more commonly known as GERD, occurs when stomach acid flows back up into the esophagus, causing symptoms such as heartburn, regurgitation, and chest pain. It is a chronic condition that can significantly impact an individual’s daily life, leading to discomfort and reduced quality of life. Exploring the causes, symptoms, and treatment options for GERD is crucial for effective management of this condition.
GERD can have numerous causes, including a weak lower esophageal sphincter (LES), obesity, hiatal hernia, and certain lifestyle factors such as smoking and consuming fatty or acidic foods. The lower esophageal sphincter is a ring of muscle that acts as a valve between the esophagus and the stomach. When it weakens or relaxes inappropriately, stomach acid can flow back up into the esophagus, causing irritation and discomfort.
Symptoms of GERD vary but commonly include a burning sensation in the chest (heartburn), an unpleasant taste in the mouth, difficulty swallowing, and excessive salivation. The burning sensation is often described as a feeling of acid rising up from the stomach into the chest, causing discomfort and pain. This can be particularly bothersome after meals or when lying down.
It is important to note that experiencing occasional heartburn does not necessarily indicate GERD. Many people experience occasional heartburn due to factors such as overeating or consuming spicy foods. The diagnosis of GERD is typically made when symptoms occur at least twice a week and significantly impact an individual’s quality of life.
Fortunately, several effective treatments are available to manage GERD symptoms and prevent complications. Lifestyle modifications play a crucial role in managing GERD. These can include dietary changes, such as avoiding trigger foods like citrus fruits, tomatoes, and chocolate, as well as reducing portion sizes and eating smaller, more frequent meals. Weight loss, if necessary, can also help alleviate symptoms by reducing pressure on the stomach.
In addition to lifestyle modifications, over-the-counter antacids and acid-reducing medications can provide temporary relief from GERD symptoms. Antacids work by neutralizing stomach acid, while acid-reducing medications, such as H2 blockers and proton pump inhibitors, reduce the production of stomach acid. These medications can be effective in managing mild to moderate GERD symptoms.
In more severe cases, prescription medications or even surgical interventions may be necessary to alleviate symptoms and improve overall well-being. Prescription medications, such as stronger proton pump inhibitors, can provide more potent acid suppression. Surgical interventions, such as fundoplication, involve wrapping the upper part of the stomach around the lower esophagus to strengthen the LES and prevent acid reflux.
Regular follow-up with a healthcare provider is essential for individuals with GERD to monitor symptoms, adjust treatment plans if necessary, and prevent complications. With proper management, individuals with GERD can lead a comfortable and fulfilling life, free from the discomfort and limitations imposed by this chronic condition.
The Vagus Nerve-GERD Connection
Understanding the relationship between the vagus nerve and GERD opens up new insights into the development and treatment of this condition. The vagus nerve’s influence on GERD is multi-faceted, involving various mechanisms that researchers are still unraveling. Exploring how the vagus nerve influences GERD can potentially pave the way for innovative therapies targeting this connection.
How the Vagus Nerve Influences GERD
One hypothesis suggests that an overactive vagus nerve may lead to increased LES relaxation, allowing stomach acid to flow back into the esophagus more easily. This can result in the characteristic symptoms of GERD, such as heartburn and regurgitation. However, the vagus nerve’s influence on GERD extends beyond just the physical aspect.
Recent studies have shown that the vagus nerve also plays a role in the perception of pain and sensitivity. Individuals with GERD often experience discomfort and a burning sensation in the chest, known as heartburn. The vagus nerve’s involvement in pain perception may contribute to the intensity of these symptoms, making them more pronounced in individuals with an overactive vagus nerve.
Furthermore, the vagus nerve is responsible for regulating the movement of food through the digestive system. When the vagus nerve is not functioning optimally, it can disrupt the normal flow of digestion, leading to issues such as delayed gastric emptying. This delay can result in the accumulation of stomach acid, increasing the likelihood of acid reflux and GERD symptoms.
While research is ongoing, it is crucial to consult with a healthcare professional to determine the most suitable treatment options for GERD. Self-diagnosis and self-medication can lead to suboptimal outcomes and potentially exacerbate symptoms. Healthcare professionals can provide personalized guidance based on an individual’s specific condition and medical history.
Scientific Research on the Vagus Nerve and GERD
Scientists and medical professionals around the world are currently investigating the vagus nerve-GERD connection through various research studies and clinical trials. Their findings could help shed light on the underlying mechanisms that contribute to GERD and pave the way for targeted therapies that address this specific aspect of the condition.
One area of research focuses on understanding the signaling pathways involved in vagus nerve activation and how they relate to GERD symptoms. By deciphering these complex pathways, researchers hope to identify potential targets for therapeutic interventions. This could lead to the development of medications or procedures that specifically target the vagus nerve, providing relief for individuals with GERD.
Other studies are exploring the potential of neuromodulation techniques to regulate vagus nerve activity in individuals with GERD. Neuromodulation involves the use of electrical or magnetic stimulation to modulate the activity of nerves. By applying these techniques to the vagus nerve, researchers aim to restore its balance and alleviate GERD symptoms.
Additionally, researchers are investigating the role of lifestyle factors in vagus nerve function and GERD. Factors such as stress, diet, and exercise have been found to influence vagus nerve activity. Understanding how these lifestyle factors interact with the vagus nerve could provide valuable insights into the prevention and management of GERD.
Overall, the ongoing scientific research on the vagus nerve-GERD connection holds promise for the future of GERD treatment. By unraveling the intricate relationship between the vagus nerve and GERD, researchers are paving the way for innovative therapies that target this specific aspect of the condition. As our understanding deepens, individuals with GERD can look forward to more effective and personalized treatment options that address the root causes of their symptoms.
Potential Therapies Targeting the Vagus Nerve
Given the vagus nerve’s significant role in regulating digestion and GERD, researchers are exploring different therapies that directly target this nerve. Vagus nerve stimulation techniques have emerged as a potential avenue for treating GERD and improving symptoms in individuals who do not respond to traditional therapies.
The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body. It plays a crucial role in the parasympathetic nervous system, which is responsible for regulating various bodily functions, including digestion, heart rate, and breathing. By stimulating the vagus nerve, researchers hope to restore balance and alleviate symptoms associated with GERD.
Vagus Nerve Stimulation Techniques
Vagus nerve stimulation involves the delivery of low-level electrical impulses to the vagus nerve, aiming to modulate its activity and restore balance in the body. This technique has been used successfully in the treatment of epilepsy and depression, and now researchers are exploring its potential in managing GERD.
One technique being studied is transcutaneous vagus nerve stimulation (tVNS), which involves applying electrical impulses to the skin overlying the vagus nerve. This non-invasive approach shows promise in reducing GERD symptoms and improving quality of life for patients. Another technique is implanted vagus nerve stimulation (iVNS), where a small device is surgically implanted to deliver electrical impulses directly to the vagus nerve.
Both tVNS and iVNS have shown positive results in early studies, with patients experiencing a reduction in GERD symptoms such as heartburn, regurgitation, and difficulty swallowing. These therapies offer hope for individuals who have not found relief with traditional treatments like medication or lifestyle modifications.
Pros and Cons of Vagus Nerve Therapies
While vagus nerve therapies show promising results, it is crucial to weigh their benefits and potential drawbacks. Like any medical intervention, these therapies come with their own set of risks and considerations.
One potential benefit of vagus nerve stimulation is its long-lasting effects. Unlike medication, which may require continuous use, vagus nerve therapies have the potential to provide sustained relief from GERD symptoms. Additionally, these therapies may reduce the need for other medications or invasive procedures, improving the overall quality of life for patients.
However, there are also potential drawbacks to consider. Vagus nerve stimulation techniques may require ongoing maintenance, such as adjusting the stimulation parameters or replacing the implanted device. Additionally, there is a risk of side effects, including hoarseness, cough, and shortness of breath, which should be carefully monitored and managed by healthcare professionals.
Consulting with a healthcare professional who specializes in treating GERD can help individuals make informed decisions and explore the suitability of vagus nerve therapies for their specific circumstances. With ongoing research and advancements in medical technology, the potential for targeted therapies that directly modulate the vagus nerve holds promise for improving the lives of those affected by GERD.
Future Directions in GERD Treatment
As the understanding of the vagus nerve’s impact on GERD continues to evolve, future directions for treatment are being explored. It is an exciting time in the field of gastroenterology, as researchers delve deeper into the complexities of this condition and seek novel solutions for those affected by GERD.
The Role of the Vagus Nerve in New GERD Treatments
Scientists are actively investigating how the vagus nerve can be leveraged to develop targeted therapies for GERD. The vagus nerve, also known as the “wandering nerve,” is a crucial component of the parasympathetic nervous system. It plays a significant role in regulating various bodily functions, including digestion. In recent years, researchers have discovered that the vagus nerve also influences the function of the lower esophageal sphincter (LES), which is a key factor in the development of GERD.
By focusing on modulating the vagus nerve’s activity, new treatment options may provide relief for individuals who do not respond to current standard treatments. This approach involves stimulating or inhibiting the vagus nerve to restore the proper functioning of the LES. Researchers are exploring various techniques, such as vagal nerve stimulation and selective vagotomy, to achieve this goal.
Early studies have shown promising results. For example, vagal nerve stimulation has been found to reduce the frequency and severity of GERD symptoms in some patients. This technique involves the use of a small device that delivers electrical impulses to the vagus nerve, helping to regulate its activity. By modulating the vagus nerve, researchers hope to improve LES function and reduce the occurrence of acid reflux episodes.
Predictions for Future GERD Therapies
Although it is difficult to predict the future of GERD therapies precisely, advancements in understanding the vagus nerve’s role offer promising possibilities. Innovative approaches, such as personalized medicine and neurostimulation techniques, may revolutionize the treatment landscape, providing tailored solutions for individuals with GERD.
Personalized medicine, also known as precision medicine, aims to customize treatment plans based on an individual’s unique characteristics, including genetic makeup, lifestyle factors, and disease progression. By analyzing these factors, doctors may be able to identify specific subtypes of GERD and develop targeted therapies that address the underlying causes of the condition. This approach holds great potential for improving treatment outcomes and reducing the burden of GERD on patients’ lives.
Neurostimulation techniques, such as transcutaneous electrical nerve stimulation (TENS) and transcranial magnetic stimulation (TMS), are also being explored as potential future therapies for GERD. These techniques involve the application of electrical or magnetic impulses to specific nerves or brain regions to modulate their activity. By targeting the vagus nerve or other neural pathways involved in GERD, researchers hope to provide long-lasting relief from symptoms and improve patients’ quality of life.
Furthermore, ongoing research is uncovering new insights into the gut-brain axis, which refers to the bidirectional communication between the gastrointestinal system and the central nervous system. This intricate network of connections plays a vital role in regulating digestive processes, including the function of the LES. By understanding the complex interplay between the gut and the brain, scientists may discover novel therapeutic targets for GERD and develop innovative treatment approaches.
In conclusion, the future of GERD treatment looks promising as researchers continue to explore the role of the vagus nerve and other neural pathways in the development of targeted therapies. With advancements in personalized medicine, neurostimulation techniques, and our understanding of the gut-brain axis, individuals with GERD may soon have access to more effective and tailored treatment options that provide long-lasting relief from symptoms.
Conclusion
The intricate connection between the vagus nerve and GERD highlights the complexity of this condition. Understanding the vagus nerve’s role in regulating digestion and its potential impact on GERD opens up new avenues for research and treatment development. As scientific discoveries continue to unfold, individuals with GERD can find solace in the fact that medical professionals are committed to finding innovative solutions. If you are experiencing symptoms of GERD, it is essential to seek medical advice to determine the most appropriate course of action for your specific situation. By collaborating with healthcare professionals, we can navigate the complexities of GERD and strive for improved outcomes and a better quality of life.
If you’re intrigued by the vital role the vagus nerve plays in managing conditions like GERD and are eager to delve deeper into its fascinating functions, “My Vagus Nerve & Me Book” is your essential guide. Discover the secrets of one of the most sophisticated systems in the human body and learn practical ways to stimulate your vagus nerve for optimal health. From enhancing your immune system to supporting vital organ functions, this book is packed with valuable insights. Ready to unlock the full potential of your vagus nerve? Get My Vagus Nerve & Me eBook today and embark on a journey to better health and well-being.