Constipation is a common gastrointestinal issue that affects millions of people worldwide. It can cause discomfort, pain, and disrupt daily life. While there are various causes of constipation, one vital factor that often goes unnoticed is the impact of the vagus nerve. Understanding the role of the vagus nerve in constipation can provide valuable insights into potential treatments and management strategies.
Understanding the Vagus Nerve
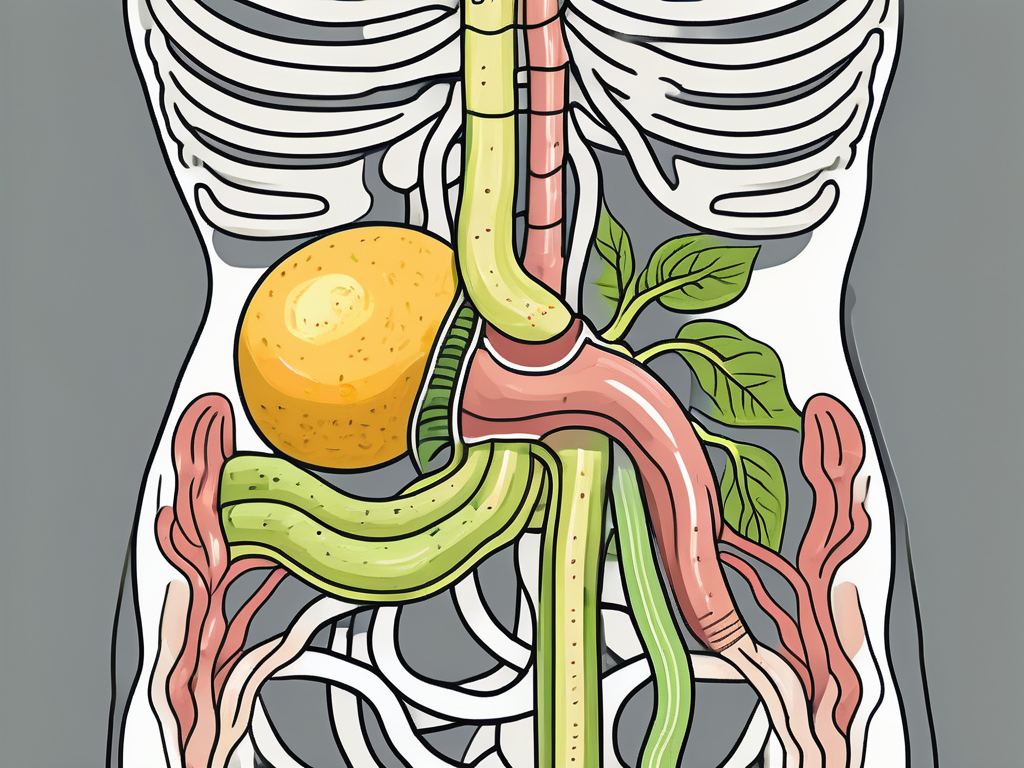
The vagus nerve, also known as the tenth cranial nerve, is an essential part of the autonomic nervous system. It is the longest cranial nerve in the body and plays a crucial role in regulating various bodily functions. Named after the Latin word for “wandering,” the vagus nerve extends from the brainstem through the neck and chest to the abdomen.
But what exactly does the vagus nerve do? Let’s dive deeper into the anatomy and function of this fascinating nerve.
The Anatomy and Function of the Vagus Nerve
The vagus nerve is responsible for transmitting vital information between the brain and different organs in the body, including the heart, lungs, stomach, and intestines. It consists of motor and sensory fibers that control both voluntary and involuntary actions.
The motor fibers of the vagus nerve help regulate various muscles, including those involved in swallowing, speech, and digestion. These fibers ensure that our bodies can perform essential functions, such as breaking down food and absorbing nutrients.
On the other hand, the sensory fibers of the vagus nerve transmit information about the state of the body’s internal organs back to the brain. This feedback loop allows our brain to monitor and adjust various bodily functions, ensuring that everything is running smoothly.
The Vagus Nerve’s Role in the Digestive System
When it comes to the digestive system, the vagus nerve plays a significant role in orchestrating the entire process. It regulates the production and release of stomach acid, digestive enzymes, and controls the rhythmic muscle contractions that move food through the digestive tract.
Imagine enjoying a delicious meal. As you take your first bite, the vagus nerve immediately gets to work. It signals the stomach to start producing stomach acid and digestive enzymes, preparing your body to break down the food into smaller, more manageable pieces.
But the vagus nerve’s involvement doesn’t stop there. It also controls the rhythmic muscle contractions, known as peristalsis, that move food through the digestive tract. These contractions ensure that the food is properly mixed with digestive enzymes and pushed along the gastrointestinal tract, allowing for efficient absorption of nutrients.
Furthermore, the vagus nerve communicates with the brain to stimulate the sensation of fullness, allowing us to recognize when we are satiated and prevent overeating. This communication between the gut and the brain is crucial for maintaining a healthy balance in our eating habits.
So, the next time you enjoy a meal, take a moment to appreciate the intricate dance between your vagus nerve and your digestive system. It’s a remarkable partnership that ensures our bodies can break down and absorb the nutrients we need to thrive.
The Connection Between the Vagus Nerve and Constipation
Constipation occurs when bowel movements become infrequent or difficult to pass. While multiple factors contribute to constipation, dysfunction or impairment of the vagus nerve can significantly impact the normal functioning of the digestive system.
Constipation is a common gastrointestinal issue that affects millions of people worldwide. It can cause discomfort, bloating, and even pain. Understanding the role of the vagus nerve in bowel movements can shed light on the potential causes of constipation and help develop effective treatment strategies.
How the Vagus Nerve Influences Bowel Movements
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions, including digestion. It controls the movement of the muscles in the intestines that propel waste through the digestive tract. This peristaltic movement is necessary for regular bowel movements.
When the vagus nerve functions optimally, it sends signals to the intestines, triggering muscle contractions that propel stool forward. These contractions create a wave-like motion, allowing for the efficient movement of waste through the digestive system. Dysfunction of the vagus nerve can disrupt this process, resulting in inadequate muscle contractions and leading to sluggish or inefficient bowel movements.
Furthermore, the vagus nerve also regulates the relaxation of the muscles in the rectum, allowing for the timely and effortless passage of stool. When this function is disrupted, individuals may experience difficulty passing stool, contributing to constipation.
Vagus Nerve Dysfunction and Constipation
Vagus nerve dysfunction can occur due to various factors, such as damage to the nerve or underlying health conditions. Conditions like diabetes, multiple sclerosis, and autonomic neuropathy can compromise the normal functioning of the vagus nerve and contribute to constipation.
Diabetes, for example, can lead to neuropathy, a condition characterized by nerve damage. When the vagus nerve is affected by neuropathy, its ability to regulate bowel movements may be impaired, resulting in constipation.
Similarly, multiple sclerosis, an autoimmune disease that affects the central nervous system, can cause damage to the nerves, including the vagus nerve. This damage can disrupt the communication between the brain and the intestines, leading to constipation.
It is important to note that while vagus nerve dysfunction may play a role in some cases of constipation, it is not the sole cause. Other factors, such as dietary choices, lack of physical activity, and certain medications, can also contribute to constipation. Consulting with a healthcare professional is essential to determine the underlying cause of constipation accurately and develop an appropriate treatment plan.
In conclusion, the vagus nerve plays a vital role in regulating bowel movements. Dysfunction or impairment of this nerve can significantly impact the normal functioning of the digestive system, potentially leading to constipation. Understanding the connection between the vagus nerve and constipation can help healthcare professionals develop targeted treatment plans to alleviate this common gastrointestinal issue.
Diagnosing Vagus Nerve-Related Constipation
If vagus nerve dysfunction is suspected as a contributing factor to constipation, a comprehensive diagnosis is necessary to confirm the condition and guide treatment decisions.
Symptoms and Signs of Vagus Nerve Dysfunction
Identifying the symptoms of vagus nerve dysfunction can help healthcare providers assess its potential impact on constipation. Symptoms may include difficulty swallowing, heartburn, bloating, and a sense of fullness despite eating small amounts. Additionally, individuals may experience changes in heart rate and blood pressure.
Difficulty swallowing, known as dysphagia, is a common symptom of vagus nerve dysfunction. It can manifest as a feeling of food getting stuck in the throat or chest, making it challenging to eat or drink. This symptom can significantly impact an individual’s quality of life and nutritional intake.
Heartburn, also known as acid reflux, is another symptom associated with vagus nerve dysfunction. It occurs when stomach acid flows back into the esophagus, causing a burning sensation in the chest. This discomfort can be exacerbated by certain foods, stress, or lying down after a meal.
Bloating is a common complaint among individuals with vagus nerve dysfunction. It refers to the feeling of fullness and tightness in the abdomen, often accompanied by increased gas production. This symptom can cause discomfort and affect a person’s self-confidence and daily activities.
A sense of fullness despite eating small amounts, known as early satiety, is another indicator of vagus nerve dysfunction. This feeling can occur shortly after starting a meal, leading to reduced food intake and potential weight loss. Early satiety can be frustrating and may require dietary modifications to ensure adequate nutrition.
In addition to these gastrointestinal symptoms, vagus nerve dysfunction can also affect cardiovascular function. Changes in heart rate and blood pressure may occur, leading to episodes of dizziness, lightheadedness, or even fainting. These cardiovascular symptoms should not be ignored and should be evaluated by a healthcare professional.
Medical Tests and Procedures for Diagnosis
Various medical tests and procedures can aid in diagnosing vagus nerve dysfunction. These may include imaging tests, such as magnetic resonance imaging (MRI), to visualize the nerve’s structure and identify any abnormalities. Additionally, nerve conduction studies and specialized tests assessing gastrointestinal function may be recommended.
Magnetic resonance imaging (MRI) is a non-invasive imaging technique that uses powerful magnets and radio waves to create detailed images of the body’s internal structures. In the case of vagus nerve dysfunction, an MRI can help identify any structural abnormalities or compression that may be affecting the nerve’s function.
Nerve conduction studies involve the placement of electrodes on the skin to measure the electrical activity of the nerves. This test can assess the conduction speed and integrity of the vagus nerve, providing valuable information about its functionality.
Specialized tests assessing gastrointestinal function may also be performed to evaluate the impact of vagus nerve dysfunction on the digestive system. These tests can include gastric emptying studies, esophageal manometry, and anorectal manometry, among others. They help assess the movement and coordination of the digestive tract, providing insights into any abnormalities that may contribute to constipation.
It is crucial to consult with a healthcare professional who can guide you through the appropriate diagnostic process based on your specific symptoms and medical history. They will consider your individual case and may recommend additional tests or procedures to ensure an accurate diagnosis.
Treatment Options for Vagus Nerve-Related Constipation
Managing constipation related to vagus nerve dysfunction involves addressing the underlying cause and implementing various treatment strategies to promote regular bowel movements.
Constipation can be a frustrating and uncomfortable condition, but there are several treatment options available to help alleviate symptoms and improve bowel function. In addition to the lifestyle changes and home remedies mentioned earlier, there are other approaches that healthcare professionals may recommend based on the severity and underlying cause of the constipation.
Lifestyle Changes and Home Remedies
Simple lifestyle changes can often help alleviate constipation symptoms. Increasing fiber intake, drinking an adequate amount of water, and engaging in regular physical activity can promote healthy bowel movements. Additionally, establishing a regular toilet routine and allowing ample time for bowel movements can be beneficial.
It is crucial to consult with a healthcare professional before making any significant lifestyle changes, as they can provide personalized guidance based on your individual needs and medical history. They may also recommend specific dietary modifications or additional home remedies that can further support bowel regularity.
Medications and Supplements
When lifestyle modifications alone are insufficient, healthcare providers may recommend medications or supplements to address vagus nerve-related constipation. These may include laxatives, stool softeners, or medications that target specific receptors in the digestive system to stimulate bowel movements.
It is important to note that self-medicating is not advisable, as certain medications may have side effects or interactions with other medications you may be taking. Always consult with a healthcare professional before starting any new medications or supplements. They can evaluate your specific situation and prescribe the most appropriate treatment option for you.
Surgical and Non-Surgical Procedures
In severe cases, surgical or non-surgical procedures may be considered to manage constipation caused by vagus nerve dysfunction. These procedures aim to alleviate obstruction or improve the movement of stool through the digestive system.
One example of a surgical procedure is a colectomy, which involves removing a portion of the colon to improve bowel function. Non-surgical procedures, such as sacral nerve stimulation or biofeedback therapy, may also be recommended to help regulate bowel movements.
However, these interventions are typically reserved for cases where conservative measures have proven ineffective and should be thoroughly discussed with a healthcare professional to weigh the potential risks and benefits. They can provide detailed information about the specific procedures, their success rates, and any potential complications that may arise.
Remember, each person’s experience with vagus nerve-related constipation is unique, and the most effective treatment plan may vary from individual to individual. It is essential to work closely with a healthcare professional to determine the most appropriate treatment options for your specific needs and to ensure the best possible outcome.
The Future of Vagus Nerve Research in Constipation Management
Researchers and healthcare professionals continue to explore innovative therapies and interventions to address constipation related to vagus nerve dysfunction.
The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body. It plays a crucial role in regulating various bodily functions, including digestion. When the vagus nerve is not functioning properly, it can lead to constipation, a condition characterized by infrequent bowel movements and difficulty passing stool.
Emerging Therapies and Interventions
One promising area of research involves neuromodulation techniques aiming to restore vagus nerve function. These techniques include vagus nerve stimulation, which involves low-level electrical impulses being delivered to the nerve to improve its functioning.
Neuromodulation therapies, such as vagus nerve stimulation, have shown significant potential in various medical conditions. They work by altering the electrical activity of the nervous system, thereby influencing the function of specific nerves. In the case of constipation management, vagus nerve stimulation aims to enhance the communication between the brain and the digestive system, promoting regular bowel movements.
While these emerging therapies show potential, it is essential to understand that they are still in the investigational stage. Further research and clinical trials are needed to confirm their efficacy and safety.
The Potential of Vagus Nerve Stimulation
Vagus nerve stimulation is a technique that has shown promise in various medical conditions. It involves the use of a small device implanted under the skin to deliver electrical impulses to the vagus nerve. Although primarily used for epilepsy and depression, researchers are investigating its potential in managing constipation by targeting vagus nerve dysfunction.
Studies have shown that vagus nerve stimulation can have a positive impact on gastrointestinal motility, the movement of food through the digestive system. By stimulating the vagus nerve, researchers hope to regulate and improve the coordination of muscle contractions in the intestines, ultimately alleviating constipation symptoms.
It is important to note that while these emerging therapies hold promise, they are not widely available and must be approached cautiously. Consultation with healthcare professionals specializing in neuromodulation therapies can provide valuable guidance and insights.
In addition to neuromodulation techniques, other avenues of vagus nerve research in constipation management include the exploration of pharmacological interventions and lifestyle modifications. Researchers are investigating the potential of certain medications that target vagus nerve receptors to enhance bowel movements and alleviate constipation symptoms.
Furthermore, lifestyle modifications, such as dietary changes and regular exercise, can also have a positive impact on vagus nerve function and overall digestive health. Consuming a diet rich in fiber and staying hydrated can promote regular bowel movements, while physical activity can stimulate the vagus nerve and improve gastrointestinal motility.
As the understanding of the vagus nerve and its role in constipation management continues to evolve, healthcare professionals and researchers are optimistic about the potential for more targeted and effective interventions. By exploring the intricate connection between the brain and the digestive system, new therapies may emerge that provide relief and improve the quality of life for individuals experiencing constipation related to vagus nerve dysfunction.
Conclusion
The vagus nerve plays a pivotal role in regulating the digestive system, and dysfunction in this nerve can significantly impact bowel movements, potentially leading to constipation. While vagus nerve-related constipation is complex and requires a comprehensive approach to diagnosis and treatment, it is important to consult with a healthcare professional for an accurate assessment of individual symptoms and appropriate management strategies. Ongoing research into emerging therapies and interventions gives hope for improved treatment options in the future, ultimately enhancing the quality of life for individuals experiencing constipation related to vagus nerve dysfunction.
If you’re fascinated by the critical role the vagus nerve plays in your health and are eager to dive deeper into its functions and the ways to optimize its performance, “My Vagus Nerve & Me Book” is the perfect resource for you. Discover the secrets of one of the most sophisticated systems in the human body, and learn practical tips for stimulating your vagus nerve to enhance your immune system, digestion, heart rate, and mental health. Don’t miss out on the opportunity to unlock the full potential of your well-being. Get My Vagus Nerve & Me eBook today and take the first step towards a healthier, more balanced life.