The Vagus Nerve is a crucial component of our autonomic nervous system, with far-reaching effects on various bodily functions, including digestion and bowel movements. Understanding the intricate relationship between the Vagus Nerve and bowel movements is essential to shed light on the underlying mechanisms and potential implications for individuals experiencing gastrointestinal issues. In this article, we will delve into the anatomy and functions of the Vagus Nerve, explore its role in digestion, examine its impact on bowel movements, discuss disorders related to the Vagus Nerve, and explore current and future treatments targeting this vital nerve.
Understanding the Vagus Nerve
Anatomy and Functions of the Vagus Nerve
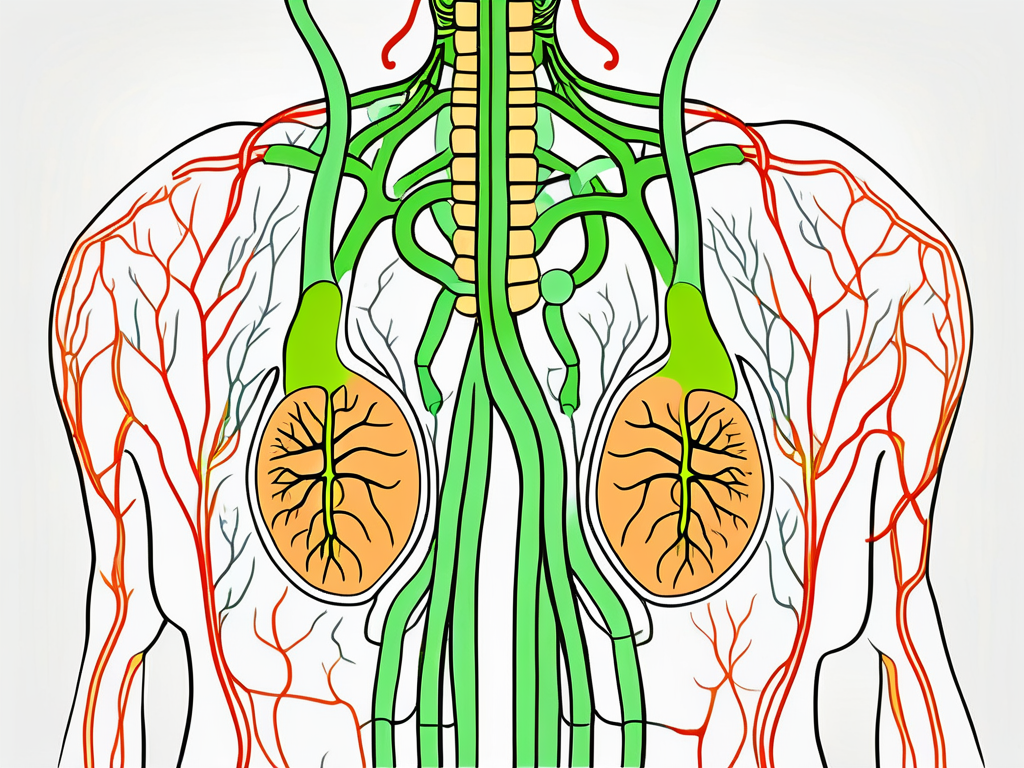
The Vagus Nerve, also known as the tenth cranial nerve, is the longest and most complex nerve in the body. It originates in the brainstem and extends down to various organs throughout the body, including the heart, lungs, and gastrointestinal tract. The Vagus Nerve is responsible for regulating many essential bodily functions, including heart rate, breathing, and digestion.
As part of the autonomic nervous system, the Vagus Nerve plays a crucial role in the parasympathetic division, which is responsible for promoting relaxation, rest, and digestion. It acts as a communication highway between the brain and various organs, transmitting signals that control and coordinate gastrointestinal processes.
The Vagus Nerve consists of both sensory and motor fibers. The sensory fibers carry information from the organs back to the brain, providing feedback on their status and allowing the brain to make necessary adjustments. The motor fibers, on the other hand, carry signals from the brain to the organs, instructing them on how to function optimally.
One of the key functions of the Vagus Nerve is to regulate heart rate. It helps to slow down the heart rate during periods of relaxation and rest, promoting a state of calmness. Additionally, the Vagus Nerve plays a role in controlling blood pressure, helping to maintain it within a healthy range.
The Vagus Nerve and the Autonomic Nervous System
The Vagus Nerve is closely intertwined with the autonomic nervous system, which consists of both the sympathetic and parasympathetic divisions. While the sympathetic division prepares the body for “fight or flight” responses, the parasympathetic division, in which the Vagus Nerve is heavily involved, promotes relaxation, digestion, and other functions that occur during restful states.
When we eat a meal, the parasympathetic division, through the Vagus Nerve, aids in the secretion of digestive enzymes, stimulates peristalsis (the contraction of muscles in the digestive tract), and increases blood flow to the digestive organs. These actions help to break down food, move it through the digestive tract, and absorb essential nutrients.
Furthermore, the Vagus Nerve is not only responsible for regulating digestion but also plays a role in the communication between the gut and the brain. It is involved in the gut-brain axis, a bidirectional communication system that influences various aspects of our health, including mood, appetite, and immune function.
Research has shown that the Vagus Nerve is connected to the enteric nervous system, which is often referred to as the “second brain.” This intricate network of neurons in the gut communicates with the central nervous system, including the brain, through the Vagus Nerve. This communication allows the gut to send signals to the brain, influencing our emotions and overall well-being.
Moreover, the Vagus Nerve has been found to play a role in inflammation regulation. It can help to reduce inflammation in the body by releasing anti-inflammatory molecules and inhibiting the release of pro-inflammatory substances. This anti-inflammatory effect of the Vagus Nerve has important implications for various health conditions, including autoimmune diseases and chronic inflammation.
Overall, the Vagus Nerve is a fascinating and vital component of our nervous system. Its extensive reach and multifaceted functions make it an essential player in regulating various bodily processes, from digestion to heart rate. Understanding the intricate workings of the Vagus Nerve can provide valuable insights into the mind-body connection and open up new avenues for therapeutic interventions.
The Vagus Nerve and Digestion
Role of the Vagus Nerve in Digestive Processes
The Vagus Nerve plays a vital role in regulating digestive processes throughout the entire gastrointestinal system. It stimulates the secretion of digestive juices, such as stomach acid, bile, and enzymes, which are necessary for proper digestion and nutrient absorption.
Furthermore, the Vagus Nerve is involved in the complex process of nutrient sensing. It detects the presence of nutrients in the digestive system and sends signals to the brain, which in turn regulates the release of hormones that control hunger, satiety, and metabolism. This intricate feedback loop ensures that the body receives the necessary nutrients and maintains energy balance.
Additionally, the Vagus Nerve helps coordinate the movement of food through the digestive tract. It controls the rhythmic contractions of the esophagus, stomach, and intestines, ensuring that food is properly propelled and broken down as it progresses through the digestive system.
How the Vagus Nerve Influences Gut Motility
Gut motility refers to the coordinated movement and contraction of muscles in the digestive tract, facilitating the digestion and elimination processes. The Vagus Nerve plays a significant role in regulating gut motility.
By stimulating the smooth muscles in the gastrointestinal tract, the Vagus Nerve promotes the rhythmic contractions necessary for food to move through the intestines. This peristaltic movement ensures that food is thoroughly mixed with digestive enzymes and absorbed efficiently. Without the proper functioning of the Vagus Nerve, the motility of the digestive system may be compromised, leading to issues such as slow transit time or impaired nutrient absorption.
Moreover, the Vagus Nerve acts as a communication highway between the gut and the brain. It relays important information about the state of the digestive system to the brain, allowing for the coordination of various physiological processes. This bidirectional communication is crucial for maintaining gut health and overall well-being.
In addition to its role in gut motility, the Vagus Nerve also influences the release of various neurotransmitters in the digestive system. For example, it stimulates the release of acetylcholine, a neurotransmitter that enhances the contraction of smooth muscles in the intestines. This ensures proper movement of food and waste products through the digestive tract.
Furthermore, the Vagus Nerve has been found to have a modulatory effect on the gut microbiota, the complex community of microorganisms residing in the digestive system. It helps regulate the balance of beneficial and harmful bacteria, promoting a healthy gut microbiome. This symbiotic relationship between the Vagus Nerve and the gut microbiota has far-reaching implications for overall health, including immune function, mental well-being, and even weight regulation.
The Vagus Nerve and Bowel Movements
The Vagus Nerve’s Impact on Bowel Regularity
Having regular bowel movements is essential for overall digestive health. The Vagus Nerve contributes to bowel regularity by ensuring the proper functioning of the digestive system.
When the Vagus Nerve is functioning optimally, it helps to regulate the speed and efficiency at which food is processed and waste is eliminated. A healthy Vagus Nerve helps maintain the balance between gut motility and adequate absorption of nutrients, promoting regular and healthy bowel movements.
The Vagus Nerve is a crucial component of the parasympathetic nervous system, which is responsible for controlling the body’s rest and digest functions. It originates in the brainstem and extends down to various organs, including the digestive tract. This nerve acts as a communication highway, transmitting signals between the brain and the gut.
Within the digestive system, the Vagus Nerve plays a vital role in coordinating the complex processes involved in digestion. It sends signals to the stomach, intestines, and other digestive organs, influencing their activities. These signals help regulate the secretion of digestive enzymes, the movement of food through the intestines, and the absorption of nutrients.
Moreover, the Vagus Nerve also interacts with the enteric nervous system, often referred to as the “second brain” of the body. This intricate network of neurons within the gastrointestinal tract works in tandem with the Vagus Nerve to ensure optimal digestion and bowel function.
The Vagus Nerve and Constipation
Constipation is a common gastrointestinal issue characterized by infrequent or difficulty in passing stools. While there can be various causes for constipation, disruptions in Vagus Nerve function can play a role in its development.
When the Vagus Nerve is not functioning properly, it can lead to slowed gut motility and impaired coordination of muscle contractions in the intestines, making it harder for stool to move through the digestive system. This can result in constipation. However, it’s essential to note that constipation can have many other causes, and consulting with a healthcare professional is advised for an accurate diagnosis and appropriate treatment.
In addition to its role in gut motility, the Vagus Nerve also influences the secretion of fluids in the digestive tract. Adequate hydration of the intestines is crucial for maintaining soft and easily passable stools. When the Vagus Nerve is functioning optimally, it helps stimulate the secretion of fluids that lubricate the intestines, facilitating smooth bowel movements.
Furthermore, the Vagus Nerve’s impact on constipation extends beyond its direct effects on gut motility. This nerve also plays a role in regulating the body’s stress response. Chronic stress can contribute to constipation by disrupting the balance of hormones and neurotransmitters involved in digestion. The Vagus Nerve helps counteract the effects of stress by activating the parasympathetic nervous system, promoting relaxation and optimal digestive function.
The Vagus Nerve and Diarrhea
Diarrhea is a gastrointestinal condition characterized by loose or watery stools. While the Vagus Nerve generally contributes to maintaining regular bowel movements, certain conditions or disruptions in Vagus Nerve function can lead to diarrhea.
In some cases, overstimulation of the Vagus Nerve can lead to increased intestinal contractions and accelerated gut motility, resulting in diarrhea. Additionally, certain gastrointestinal disorders or infections can affect the Vagus Nerve’s function, leading to diarrhea. It is important to speak with a healthcare professional to determine the underlying cause of diarrhea and receive appropriate treatment.
Moreover, the Vagus Nerve’s role in diarrhea extends beyond its effects on gut motility. This nerve is involved in regulating the immune response within the gastrointestinal tract. When the Vagus Nerve is functioning optimally, it helps maintain a balance between immune activation and regulation, preventing excessive inflammation in the gut. Disruptions in Vagus Nerve function can lead to an overactive immune response, resulting in diarrhea.
Furthermore, the Vagus Nerve also interacts with the gut microbiota, the trillions of microorganisms residing in the digestive tract. This complex ecosystem of bacteria, viruses, and fungi plays a crucial role in maintaining gut health. The Vagus Nerve helps regulate the composition and activity of the gut microbiota, influencing various aspects of digestion and bowel function. Imbalances in the gut microbiota, often referred to as dysbiosis, can contribute to diarrhea.
Understanding the intricate relationship between the Vagus Nerve and bowel movements is essential for maintaining optimal digestive health. By promoting a healthy Vagus Nerve function through lifestyle modifications, stress management, and appropriate medical interventions, individuals can support regular and healthy bowel movements.
Disorders Related to the Vagus Nerve and Bowel Movements
Irritable Bowel Syndrome and the Vagus Nerve
Irritable Bowel Syndrome (IBS) is a chronic gastrointestinal disorder characterized by abdominal pain, bloating, and changes in bowel habits. While the exact cause of IBS remains unclear, disruptions in Vagus Nerve function have been linked to the development and symptomatology of this condition.
The Vagus Nerve, also known as the tenth cranial nerve, is a long and complex nerve that plays a crucial role in the communication between the gut and the brain. It is responsible for regulating various sensations, such as pain, and signaling the brain to coordinate normal bowel movements. In individuals with IBS, alterations in Vagus Nerve signaling and sensitivity can contribute to the symptoms experienced.
Research suggests that the Vagus Nerve may be involved in the regulation of gut motility, secretion, and immune response. Dysfunction of the Vagus Nerve can disrupt the delicate balance of these processes, leading to the development of IBS symptoms. However, it’s important to note that IBS is a multifactorial disorder, and the involvement of the Vagus Nerve is just one piece of the puzzle.
Diagnosing IBS can be challenging, as there is no specific test to confirm the condition. Healthcare professionals rely on a combination of symptoms, medical history, and exclusion of other potential causes to make an accurate diagnosis. Treatment for IBS often involves a multidisciplinary approach, including dietary modifications, stress management techniques, and medications to alleviate symptoms.
Gastroparesis and the Vagus Nerve
Gastroparesis is a condition characterized by delayed emptying of the stomach, leading to symptoms such as nausea, vomiting, and a feeling of fullness. The Vagus Nerve plays a crucial role in controlling gastric emptying by coordinating the rhythmic contractions of the stomach muscles.
When the Vagus Nerve is functioning properly, it sends signals to the stomach muscles to contract and push food through the digestive system. However, in individuals with gastroparesis, the Vagus Nerve’s function may be impaired, leading to disrupted coordination of stomach contractions and delayed gastric emptying.
Gastroparesis can have various causes, including diabetes, surgery, and certain medications. In some cases, the exact cause remains unknown, and the condition is referred to as idiopathic gastroparesis. Regardless of the underlying cause, consulting with a healthcare professional is crucial for proper diagnosis and management of gastroparesis.
Treatment options for gastroparesis may include dietary modifications, such as consuming smaller and more frequent meals, avoiding high-fat and high-fiber foods, and staying hydrated. Medications that stimulate stomach contractions or manage symptoms like nausea and vomiting may also be prescribed. In severe cases, surgical interventions or implantation of a gastric electrical stimulator may be considered.
It’s important to remember that the Vagus Nerve’s involvement in these disorders is just one aspect of their complex nature. Further research is needed to fully understand the mechanisms underlying the relationship between the Vagus Nerve and bowel movements, as well as to develop more targeted and effective treatments for these conditions.
Therapies and Treatments Targeting the Vagus Nerve
Vagus Nerve Stimulation for Bowel Disorders
Vagus Nerve Stimulation (VNS) is an innovative therapy that involves the use of a device implanted in the chest to deliver electrical impulses to the Vagus Nerve. This nerve, also known as the “wandering nerve,” is a major player in the body’s parasympathetic nervous system, which controls various bodily functions, including digestion. While VNS has primarily been studied and approved for the treatment of certain neurological conditions, ongoing research is exploring its potential efficacy in managing bowel disorders.
Studies have shown that the Vagus Nerve plays a crucial role in regulating gut motility, secretion, and inflammation. By stimulating this nerve, VNS aims to modulate these processes and restore normal bowel function. The device used in VNS consists of a small generator implanted under the skin, usually in the chest area, and one or more leads that deliver electrical impulses to the Vagus Nerve.
It is important to note that VNS for bowel disorders is still an area of active research, and its specific applications and long-term effects are being investigated. While some studies have shown promising results in improving symptoms such as constipation and diarrhea, more research is needed to fully understand the potential benefits and risks of this therapy. Consultation with a healthcare professional specializing in this field is crucial to determine whether VNS may be a suitable treatment option.
Lifestyle Changes to Improve Vagus Nerve Function
In addition to medical interventions, certain lifestyle modifications can potentially support optimal Vagus Nerve function and promote healthy bowel movements. While these lifestyle changes may not be applicable to all individuals, they are worth considering in consultation with a healthcare professional.
Engaging in stress-reducing activities, such as meditation, yoga, or deep breathing exercises, can help promote a healthy balance between the sympathetic and parasympathetic nervous systems, with potential beneficial effects on Vagus Nerve function. Chronic stress has been shown to negatively impact the Vagus Nerve, leading to gastrointestinal issues. By incorporating relaxation techniques into daily life, individuals may be able to improve their overall gut health.
Maintaining a balanced diet rich in fiber and staying hydrated can also support regular bowel movements. Fiber acts as a prebiotic, providing nourishment for the beneficial bacteria in the gut. These bacteria play a crucial role in maintaining gut health and promoting proper digestion. Additionally, staying hydrated helps to soften the stool and prevent constipation, which can be especially beneficial for individuals with bowel disorders.
Furthermore, regular exercise has been shown to have positive effects on Vagus Nerve function. Physical activity stimulates the Vagus Nerve, promoting the release of neurotransmitters that help regulate digestion. Incorporating moderate exercise into daily routines, such as brisk walking or cycling, can potentially improve bowel function and overall gut health.
It is important to note that while lifestyle changes can be beneficial, they may not be sufficient as standalone treatments for bowel disorders. Consulting with a healthcare professional is essential to develop a comprehensive treatment plan that addresses individual needs and incorporates both medical interventions and lifestyle modifications.
Future Research Directions
The study of the Vagus Nerve and its intricate relationship with bowel movements has opened up exciting possibilities for the development of novel treatments targeting Vagus Nerve function in various gastrointestinal conditions. Researchers are actively exploring different avenues to harness the potential of this nerve for therapeutic purposes.
One area of ongoing research focuses on pharmacological interventions that aim to modulate Vagus Nerve activity and restore its optimal function. Scientists are investigating the use of specific drugs that can selectively target the Vagus Nerve, with the goal of improving bowel movement regulation. These investigational treatments hold promise but are still in the early stages of development.
Another avenue being explored is the use of targeted therapies. Researchers are investigating various techniques to specifically stimulate or inhibit the Vagus Nerve, such as electrical stimulation or optogenetics. By manipulating the activity of this nerve, scientists hope to uncover new ways to manage gastrointestinal conditions and enhance bowel movement control.
While these potential treatments are exciting, it is important to note that they are not yet widely available. As research progresses, it will be crucial to consult with healthcare professionals who are knowledgeable about the latest developments in this field. These experts can provide valuable insights and guidance regarding potential future treatment options.
Unanswered Questions about the Vagus Nerve and Bowel Movements
Despite significant progress in understanding the relationship between the Vagus Nerve and bowel movements, there are still many unanswered questions in this fascinating area of research.
One key area of interest is further exploration of the intricacies of Vagus Nerve signaling. Scientists are working to unravel the complex mechanisms by which this nerve communicates with the gastrointestinal system and influences bowel movements. Understanding these signaling pathways in greater detail could pave the way for more targeted interventions and therapies.
Additionally, researchers are seeking to uncover the underlying mechanisms that contribute to the effects of the Vagus Nerve on bowel movements. By elucidating the molecular and cellular processes involved, scientists hope to gain a deeper understanding of how the Vagus Nerve can be harnessed to manage bowel disorders effectively.
Continued research in this field will also address the question of whether there are specific subpopulations of individuals who may benefit more from Vagus Nerve-targeted treatments. By identifying potential biomarkers or genetic factors that influence the response to Vagus Nerve interventions, researchers aim to personalize treatment approaches and optimize outcomes for patients.
Overall, the ongoing investigation into the Vagus Nerve and its role in bowel movements holds great promise for the development of more effective treatments for individuals experiencing gastrointestinal disorders. Through rigorous scientific inquiry, researchers are striving to unlock the full potential of this nerve and improve the lives of those affected.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered medical advice. If you have concerns about your bowel movements or gastrointestinal health, it is important to consult with a qualified healthcare professional for an accurate diagnosis and appropriate treatment.
Ready to embark on a journey through the wonders of the vagus nerve and its profound impact on your health? Discover the secrets of one of the most sophisticated systems within the human body with the “My Vagus Nerve & Me Book.” Delve into the complexities of this remarkable nerve, from its role in digestion and heart rate to its influence on mental health and immune function. Learn how to nurture and stimulate your vagus nerve, both naturally and artificially, to enhance your overall well-being. Embrace the opportunity to unlock the full potential of your vagus nerve and transform your health. Get My Vagus Nerve & Me eBook today and take the first step towards a deeper understanding of your body’s inner workings.