The vagus nerve is a crucial component of the body’s nervous system, playing a significant role in regulating various bodily functions, including bowel movements. Understanding the intricate relationship between the vagus nerve and bowel movements can provide valuable insights into digestive health and potential treatment options for related disorders. In this article, we will explore the anatomy and function of the vagus nerve, its role in digestion, its impact on bowel movements, disorders associated with the vagus nerve, current therapies targeting the vagus nerve, and future research directions.
Understanding the Vagus Nerve
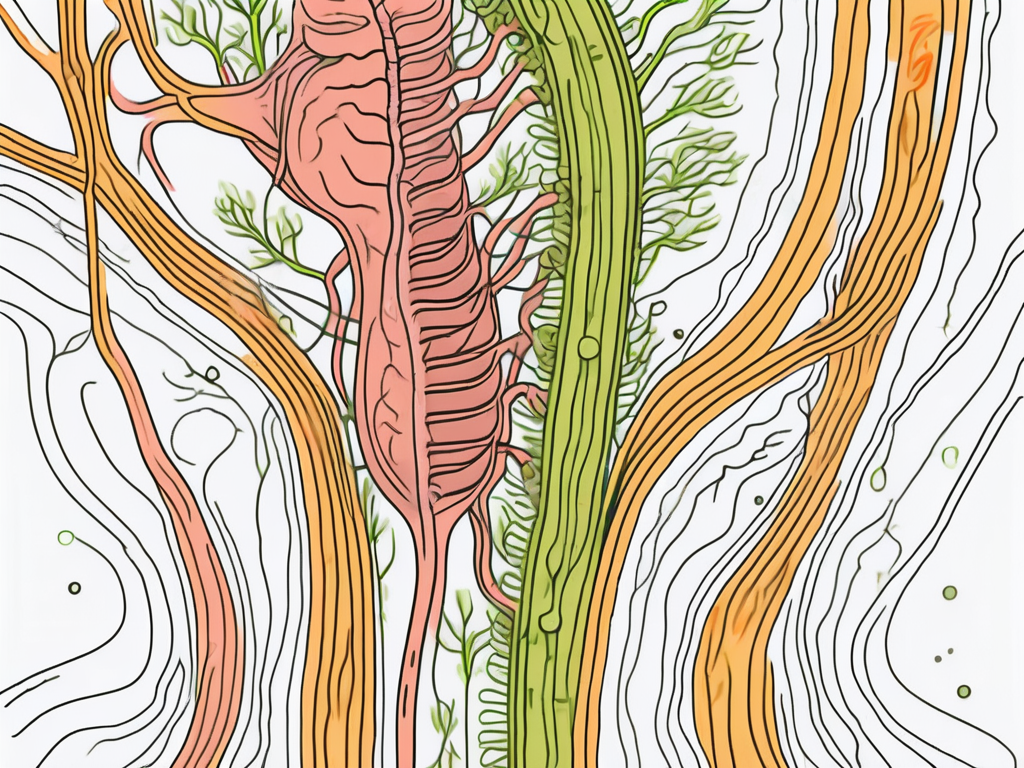
The vagus nerve, also known as the tenth cranial nerve, is one of the most extensive and complex nerves in the body. It connects the brainstem to various organs, including the heart, lungs, stomach, and intestines. This cranial nerve consists of thousands of nerve fibers that transmit signals between these organs and the brain, facilitating communication and coordination of their functions.
Anatomy and Function of the Vagus Nerve
The vagus nerve originates in the medulla oblongata, which is a part of the brainstem. It then branches out into multiple fibers that travel throughout the body. These fibers are responsible for transmitting both sensory and motor signals.
On the sensory side, the vagus nerve carries information about the body’s internal state, including sensations from the digestive organs. This feedback helps the brain monitor and regulate various physiological processes, such as heart rate, breathing, and digestion.
In terms of motor function, the vagus nerve controls the parasympathetic division of the autonomic nervous system. This division is responsible for promoting rest and digestion, which includes regulating bowel movements.
The vagus nerve plays a crucial role in maintaining homeostasis within the body. It acts as a communication highway, allowing the brain to receive constant updates on the state of the organs it connects to. This information is essential for the brain to make adjustments and ensure that the body functions optimally.
For example, when the body is in a state of rest, the vagus nerve helps stimulate the release of digestive enzymes, preparing the gastrointestinal tract for the digestion of food. It also increases blood flow to the digestive organs, ensuring that they receive the necessary oxygen and nutrients to carry out their functions effectively.
Furthermore, the vagus nerve enhances intestinal contractions, which are essential for the movement of food through the digestive system. These contractions, known as peristalsis, help propel food along the digestive tract, allowing for efficient absorption of nutrients and elimination of waste.
The Vagus Nerve and the Autonomic Nervous System
The autonomic nervous system consists of two branches: the sympathetic and the parasympathetic. While the sympathetic division prepares the body for “fight or flight” responses, the parasympathetic division activates the rest and digest mode.
The vagus nerve primarily controls the parasympathetic division, which stimulates digestive processes, including bowel movements. When the vagus nerve is activated, it prompts the release of digestive enzymes, increases blood flow to the gastrointestinal tract, and enhances intestinal contractions, facilitating the movement of food through the digestive system.
In addition to its role in digestion, the vagus nerve also influences other bodily functions. It helps regulate heart rate, promoting a steady and regular rhythm. It also plays a role in controlling blood pressure, ensuring that it remains within a healthy range.
Furthermore, the vagus nerve is involved in the regulation of breathing. It helps coordinate the muscles involved in respiration, ensuring that oxygen is efficiently delivered to the body’s tissues and carbon dioxide is effectively eliminated.
Overall, the vagus nerve is a vital component of the autonomic nervous system, contributing to the maintenance of various physiological processes. Its extensive reach and intricate connections make it a fascinating and essential part of the human body.
The Vagus Nerve’s Role in Digestion
Bowel movements are a crucial part of the digestive process, allowing the body to eliminate waste and maintain its overall health. The vagus nerve influences digestion through its interactions with the enteric nervous system, a network of nerves embedded in the gut wall, and its ability to regulate gut motility.
The Vagus Nerve and the Enteric Nervous System
The enteric nervous system operates independently of the central nervous system but still communicates with it through the vagus nerve. It controls various facets of gut function, including digestion, absorption, and bowel movements.
Embedded within the gut wall, the enteric nervous system consists of a vast network of neurons that work together to ensure the smooth functioning of the digestive system. These neurons communicate with each other and with the vagus nerve, allowing for coordinated and efficient digestion.
One fascinating aspect of the enteric nervous system is its ability to function autonomously. It can carry out its tasks without constant input from the brain, relying instead on local reflexes and feedback loops. However, it still maintains a line of communication with the central nervous system through the vagus nerve, allowing for coordination and regulation.
Through its connections with the enteric nervous system, the vagus nerve helps coordinate the complex choreography of gut motility, ensuring that food moves through the digestive tract at an appropriate pace for optimal digestion and absorption.
How the Vagus Nerve Influences Gut Motility
Gut motility refers to the rhythmic contractions of the intestines that propel food through the digestive system. The vagus nerve plays a vital role in regulating these contractions, keeping them in sync and preventing issues such as constipation or diarrhea.
Within the intestines, the smooth muscle tissue contracts and relaxes in a coordinated pattern to push food along the digestive tract. This process, known as peristalsis, is controlled by the enteric nervous system under the influence of the vagus nerve.
When the vagus nerve detects food in the stomach, it signals the enteric nervous system to increase gut motility. This stimulates smooth muscle contractions that propel the food forward. The vagus nerve also coordinates the release of digestive enzymes and hormones that aid in the breakdown and absorption of nutrients.
Conversely, when the stomach is empty or digestion is complete, the vagus nerve reduces the stimulation, allowing the intestines to rest. This regulation prevents excessive contractions and ensures that the digestive system operates efficiently without unnecessary strain.
Furthermore, the vagus nerve also plays a role in the sensation of fullness or satiety. It relays signals from the gut to the brain, informing it of the stomach’s contents and triggering feelings of satisfaction and the cessation of hunger.
Overall, the vagus nerve’s involvement in digestion and gut motility highlights its crucial role in maintaining the proper functioning of the digestive system. Its intricate connections with the enteric nervous system allow for coordinated movements and efficient digestion, ensuring that nutrients are absorbed, waste is eliminated, and overall health is maintained.
The Vagus Nerve and Bowel Movements
The vagus nerve’s impact on bowel movements extends beyond regulating gut motility. It also influences bowel frequency and can play a role in conditions such as constipation and diarrhea.
The Vagus Nerve’s Impact on Bowel Frequency
Bowel frequency varies among individuals, but the vagus nerve helps maintain a healthy balance. When the vagus nerve functions optimally, it promotes regular and predictable bowel movements, ensuring that waste is efficiently eliminated from the body.
In addition to regulating gut motility, the vagus nerve also communicates with the enteric nervous system, which is responsible for coordinating various aspects of digestion, including bowel frequency. This intricate network of nerves helps ensure that the digestive process runs smoothly.
However, disruptions in vagus nerve signaling can lead to alterations in bowel frequency, such as increased or decreased bowel movements. Conditions like irritable bowel syndrome (IBS) or gastroparesis can affect vagus nerve function and result in abnormal bowel patterns.
For example, in individuals with IBS, the vagus nerve may be hypersensitive, leading to exaggerated responses in the intestines and irregular bowel movements. On the other hand, gastroparesis, a condition characterized by delayed stomach emptying, can also impact the vagus nerve’s ability to regulate bowel frequency.
The Vagus Nerve and Constipation
Constipation occurs when stool moves too slowly through the colon, leading to infrequent or difficult bowel movements. The vagus nerve’s role in stimulating gut motility is crucial to prevent constipation. Dysfunction or impaired signaling of the vagus nerve can contribute to constipation by reducing the frequency or strength of intestinal contractions.
In addition to its role in gut motility, the vagus nerve also influences the secretion of digestive enzymes and the release of substances that promote bowel movements. These coordinated actions ensure that waste is efficiently propelled through the digestive tract.
If you experience chronic constipation, it is essential to consult with a healthcare professional for a proper diagnosis and personalized treatment plan. They can help identify the underlying cause and recommend appropriate interventions.
Treatment options for constipation may include dietary modifications, increased physical activity, and medications that help regulate bowel movements. In some cases, addressing underlying conditions that affect vagus nerve function, such as diabetes or hypothyroidism, may also be necessary.
The Vagus Nerve and Diarrhea
Diarrhea, on the other hand, refers to loose or watery stools and increased bowel movements. In some cases, the vagus nerve can also play a role in diarrhea. When the vagus nerve is overstimulated, it can lead to excessive contractions in the intestines, causing rapid transit of stool and resulting in diarrhea.
In addition to its role in regulating gut motility, the vagus nerve also communicates with the immune system and helps modulate inflammation in the gut. Imbalances in this communication can lead to increased intestinal permeability and alterations in fluid balance, contributing to diarrhea.
If you are experiencing persistent diarrhea, it is advisable to seek medical advice for a thorough evaluation. A healthcare professional can assess your symptoms and determine the most appropriate course of action.
Treatment for diarrhea may involve addressing the underlying cause, such as infections, food intolerances, or medication side effects. In some cases, medications that regulate gut motility or manage inflammation may be prescribed to alleviate symptoms.
It is important to note that while the vagus nerve plays a significant role in bowel movements, it is just one component of a complex system involving various nerves, hormones, and muscles. Understanding the intricate interplay between these factors is crucial for maintaining optimal digestive health.
Disorders Related to the Vagus Nerve and Bowel Movements
Several disorders are associated with dysfunction or abnormalities in the vagus nerve, which can impact bowel movements and overall digestive health.
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions, including digestion. It is responsible for transmitting signals between the brain and the gastrointestinal tract, ensuring the proper functioning of the digestive system.
Irritable Bowel Syndrome and the Vagus Nerve
Irritable bowel syndrome (IBS) is a prevalent gastrointestinal disorder characterized by abdominal pain, bloating, and changes in bowel habits. Emerging research suggests that dysregulation of the vagus nerve may contribute to the development and symptom severity of IBS.
The vagus nerve helps regulate the movement of food through the digestive tract by controlling the contraction and relaxation of the muscles in the intestines. When the vagus nerve is not functioning correctly, it can lead to abnormal bowel movements, such as diarrhea or constipation, which are common symptoms of IBS.
It is crucial to consult with a healthcare professional if you experience persistent gastrointestinal symptoms consistent with IBS. They can perform a thorough evaluation and provide appropriate guidance to help manage your symptoms effectively.
In addition to seeking medical advice, lifestyle modifications can also play a significant role in managing IBS symptoms. These may include dietary changes, stress management techniques, and regular exercise.
Gastroparesis and the Vagus Nerve
Gastroparesis is a disorder in which the stomach takes longer than usual to empty its contents into the small intestine. This delay in gastric emptying can result from vagus nerve damage or dysfunction, disrupting the coordination of stomach contractions necessary for proper digestion.
The vagus nerve controls the movement of food from the stomach to the small intestine by signaling the muscles in the stomach to contract and push the food forward. When the vagus nerve is impaired, these contractions may be weakened or absent, leading to delayed gastric emptying and symptoms of gastroparesis.
If you suspect you may have gastroparesis, it is essential to seek medical advice. A healthcare professional can conduct tests to diagnose the condition and suggest suitable management strategies to alleviate symptoms and improve gastric emptying.
Treatment options for gastroparesis may include dietary changes, medications to stimulate stomach contractions, and in severe cases, surgical interventions. It is important to work closely with a healthcare team to develop an individualized treatment plan based on your specific needs.
In conclusion, disorders related to the vagus nerve can significantly impact bowel movements and overall digestive health. Understanding the role of the vagus nerve in regulating digestion and seeking appropriate medical guidance are essential steps in managing these conditions effectively.
Therapies Targeting the Vagus Nerve
Given the critical role of the vagus nerve in regulating bowel movements and digestive health, researchers have explored various therapeutic approaches targeting this nerve to manage related conditions.
The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body. It extends from the brainstem to various organs, including the heart, lungs, and digestive system. This nerve plays a crucial role in the parasympathetic nervous system, which is responsible for rest and digest functions.
One therapeutic approach that has gained attention is vagus nerve stimulation (VNS) therapy. This innovative treatment involves the use of an implanted device that delivers regular electrical impulses to the vagus nerve. VNS therapy has been approved for the treatment of certain neurological conditions, such as epilepsy and depression. The electrical impulses sent to the vagus nerve can help regulate brain activity and mood, but they can also have an impact on digestive health.
While VNS has shown promise in managing certain gastrointestinal disorders, such as gastroparesis and inflammatory bowel disease, further research is needed to establish its efficacy and safety in these specific contexts. Scientists are conducting clinical trials to better understand how VNS therapy can be optimized for digestive health conditions.
Vagus Nerve Stimulation Therapy
Vagus nerve stimulation therapy involves the use of an implanted device that delivers regular electrical impulses to the vagus nerve. This therapy has been approved for the treatment of certain neurological conditions, such as epilepsy and depression. The device, typically implanted in the chest, is connected to the vagus nerve through a wire. It delivers mild electrical pulses to the nerve, helping to regulate its activity.
When it comes to digestive health, VNS therapy has shown promising results in managing conditions like gastroparesis, a disorder that affects the stomach’s ability to empty properly. By stimulating the vagus nerve, this therapy can help improve gastric motility and alleviate symptoms such as nausea, vomiting, and bloating.
Additionally, VNS therapy has been explored as a potential treatment for inflammatory bowel disease (IBD), including Crohn’s disease and ulcerative colitis. These chronic conditions involve inflammation of the digestive tract, leading to symptoms like abdominal pain, diarrhea, and weight loss. By modulating the vagus nerve, VNS therapy may help regulate the immune response and reduce inflammation in the gut, providing relief for individuals with IBD.
Lifestyle Changes to Improve Vagus Nerve Function
In addition to medical interventions, adopting healthy lifestyle habits may help optimize vagus nerve function and promote optimal bowel movements. Engaging in stress-reducing activities like meditation and deep breathing exercises can activate the parasympathetic nervous system, stimulating the vagus nerve and promoting relaxation.
Furthermore, maintaining a balanced diet is crucial for supporting vagus nerve health and overall digestive well-being. Consuming a variety of fiber-rich foods, such as fruits, vegetables, and whole grains, can help regulate bowel movements and prevent constipation. Probiotic-rich foods, like yogurt and fermented vegetables, can also support a healthy gut microbiome, which plays a vital role in digestive health.
Staying physically active is another lifestyle change that can positively impact vagus nerve function. Regular exercise promotes blood circulation and stimulates the release of endorphins, which can help reduce stress and improve overall well-being. Whether it’s going for a brisk walk, practicing yoga, or engaging in strength training, finding an exercise routine that suits individual preferences can contribute to a healthy vagus nerve and digestive system.
Future Research on the Vagus Nerve and Bowel Movements
As our understanding of the vagus nerve’s intricate connections and functions continues to evolve, ongoing research aims to uncover new insights and potential treatments for conditions affecting bowel movements and digestive health.
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions, including digestion. It serves as a vital communication pathway between the brain and the gastrointestinal system, transmitting signals that influence the movement of food through the digestive tract.
Recent studies have highlighted the potential therapeutic applications of targeting the vagus nerve to address gastrointestinal disorders. Researchers have discovered that stimulating the vagus nerve can modulate the activity of the enteric nervous system, a complex network of nerves within the gastrointestinal tract that controls digestion. By manipulating the vagus nerve, scientists hope to develop innovative treatments for conditions such as irritable bowel syndrome (IBS), gastroparesis, and inflammatory bowel disease (IBD).
Potential Developments in Vagus Nerve Treatments
Scientists are actively investigating innovative approaches, such as non-invasive vagus nerve stimulation techniques, to broaden the scope of potential vagus nerve treatments. These non-invasive methods aim to stimulate the nerve externally, without the need for surgical implantation, potentially expanding access to vagus nerve treatment options.
One such technique currently being explored is transcutaneous vagus nerve stimulation (tVNS). This involves the application of low-intensity electrical currents to specific areas of the skin, which can activate the vagus nerve and trigger a cascade of physiological responses. Preliminary studies have shown promising results, suggesting that tVNS may alleviate symptoms associated with gastrointestinal disorders and improve bowel movements.
Another area of research focuses on bioelectronic devices that can selectively target and stimulate specific branches of the vagus nerve. These devices, often implanted near the nerve pathway, can deliver precise electrical impulses to modulate nerve activity. By fine-tuning the stimulation parameters, researchers hope to optimize treatment outcomes and minimize potential side effects.
The Future of Neurogastroenterology
Neurogastroenterology, the branch of medicine that focuses on the interaction between the nervous system and the gastrointestinal system, holds great promise for advancing our understanding of the vagus nerve’s impact on bowel movements and digestive health. Ongoing research in this field may pave the way for novel diagnostic tools, targeted therapies, and a deeper comprehension of the intricate neural mechanisms underlying gastrointestinal disorders.
Researchers are exploring advanced imaging techniques, such as functional magnetic resonance imaging (fMRI) and positron emission tomography (PET), to visualize the activity of the vagus nerve in real-time. These imaging modalities provide valuable insights into the neural pathways involved in gastrointestinal regulation and can help identify potential abnormalities or dysfunctions.
Furthermore, advancements in neurogastroenterology may lead to the development of personalized medicine approaches for individuals with gastrointestinal disorders. By understanding the unique characteristics of a patient’s vagus nerve and its interactions with the gastrointestinal system, healthcare providers can tailor treatment plans to address specific underlying causes and optimize therapeutic outcomes.
Ultimately, the ongoing research on the vagus nerve and its relationship to bowel movements holds immense potential for improving the lives of individuals with gastrointestinal disorders. By unraveling the complexities of this intricate neural network, scientists are paving the way for innovative treatments and a deeper understanding of the vital role the vagus nerve plays in digestive health.
In Conclusion
The vagus nerve plays a pivotal role in regulating bowel movements through its impact on gut motility and coordination with the enteric nervous system. Dysfunction or abnormalities in the vagus nerve can contribute to digestive disorders such as constipation, diarrhea, IBS, or gastroparesis. While therapies targeting the vagus nerve, such as VNS, show promise, it is crucial to consult with a healthcare professional for an accurate diagnosis and tailored treatment plan. As research on the vagus nerve and its relationship with bowel movements progresses, our understanding of these complex interactions will continue to expand, potentially leading to improved strategies for managing gastrointestinal disorders and enhancing digestive health.
If you’re fascinated by the critical role the vagus nerve plays in your overall health and are eager to delve deeper into its functions and capabilities, “My Vagus Nerve & Me Book” is the perfect resource for you. Discover the secrets of one of the most sophisticated systems in the human body, and learn how to harness its power for better immune function, digestion, heart rate, and mental health. Whether you’re interested in natural or artificial ways to stimulate the vagus nerve, this book covers it all. Take the first step towards understanding and optimizing your well-being. Get My Vagus Nerve & Me eBook today and embark on a journey to unlock the full potential of your body’s innate intelligence.