The role of the vagus nerve and parasympathetic innervation in the body has been a topic of scientific interest for many years. This intricate network of nerves plays a crucial role in regulating various bodily functions, including the function of the respiratory system. Understanding the impact of parasympathetic innervation from the vagus nerve on the airways is essential for comprehending the complex relationship between this nerve and respiratory health.
Understanding the Vagus Nerve and Parasympathetic Innervation
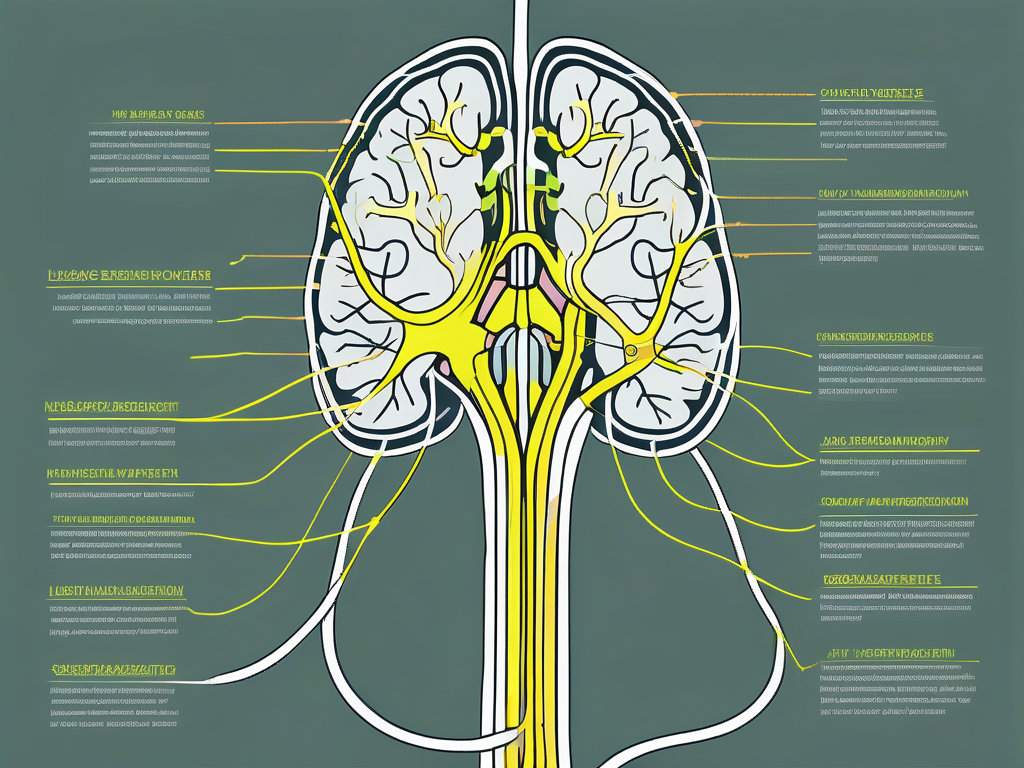
Before delving into the specifics of how the vagus nerve affects the airways, it is important to understand what the vagus nerve is and its role in the parasympathetic nervous system. The vagus nerve is the longest cranial nerve in the body and is composed of both sensory and motor fibers. It originates in the brainstem and branches out to innervate various organs in the body, including the heart, lungs, and digestive system.
The vagus nerve consists of two main branches, the left and right vagus nerves, which wrap around either side of the esophagus and descend into the chest and abdomen. It is responsible for transmitting signals between the brain and organs, allowing for the regulation of bodily functions. The motor fibers of the vagus nerve control involuntary muscle movements, while the sensory fibers carry information from the organs back to the brain.
The vagus nerve plays a crucial role in maintaining homeostasis within the body. It is involved in regulating heart rate, blood pressure, gastrointestinal motility, and respiratory function. When the body is in a state of rest and relaxation, the parasympathetic nervous system, under the control of the vagus nerve, takes over and promotes digestion, slows down the heart rate, and facilitates normal breathing.
One fascinating aspect of the vagus nerve is its ability to communicate bidirectionally between the brain and the gut. This means that the gut can send signals to the brain, influencing mood, emotions, and even cognitive function. The vagus nerve acts as a vital link in the gut-brain axis, allowing for constant communication and feedback between the two.
In addition to its role in regulating bodily functions, the vagus nerve has been found to play a role in various health conditions. Researchers have discovered that vagus nerve stimulation can be an effective treatment for epilepsy, depression, and even inflammatory diseases such as rheumatoid arthritis. By modulating the activity of the vagus nerve, it is possible to influence the body’s immune response and reduce inflammation.
Understanding the intricate workings of the vagus nerve and its role in parasympathetic innervation is crucial for comprehending how it affects the airways. The next section will explore the specific mechanisms through which the vagus nerve influences respiratory function.
Anatomy and Function of the Vagus Nerve
The vagus nerve consists of two main branches, the left and right vagus nerves, which wrap around either side of the esophagus and descend into the chest and abdomen. It is responsible for transmitting signals between the brain and organs, allowing for the regulation of bodily functions. The motor fibers of the vagus nerve control involuntary muscle movements, while the sensory fibers carry information from the organs back to the brain.
The vagus nerve plays a crucial role in maintaining homeostasis within the body. It is involved in regulating heart rate, blood pressure, gastrointestinal motility, and respiratory function. When the body is in a state of rest and relaxation, the parasympathetic nervous system, under the control of the vagus nerve, takes over and promotes digestion, slows down the heart rate, and facilitates normal breathing.
One fascinating aspect of the vagus nerve is its ability to communicate bidirectionally between the brain and the gut. This means that the gut can send signals to the brain, influencing mood, emotions, and even cognitive function. The vagus nerve acts as a vital link in the gut-brain axis, allowing for constant communication and feedback between the two.
In addition to its role in regulating bodily functions, the vagus nerve has been found to play a role in various health conditions. Researchers have discovered that vagus nerve stimulation can be an effective treatment for epilepsy, depression, and even inflammatory diseases such as rheumatoid arthritis. By modulating the activity of the vagus nerve, it is possible to influence the body’s immune response and reduce inflammation.
Understanding the intricate workings of the vagus nerve and its role in parasympathetic innervation is crucial for comprehending how it affects the airways. The next section will explore the specific mechanisms through which the vagus nerve influences respiratory function.
The Role of Parasympathetic Innervation in the Body
The parasympathetic nervous system, which is under the control of the vagus nerve, is often referred to as the “rest and digest” system. It counterbalances the sympathetic nervous system, which is responsible for the “fight or flight” response. The parasympathetic nervous system helps regulate bodily functions during periods of relaxation and rest, including digestion, heart rate, and respiratory function.
When the body is in a state of rest, the parasympathetic nervous system is activated, and the vagus nerve plays a crucial role in this process. The vagus nerve releases acetylcholine, a neurotransmitter that acts on receptors in various organs, including the airways. This activation leads to bronchoconstriction, which is the narrowing of the airways.
While bronchoconstriction may seem counterintuitive, it serves an important purpose. During periods of rest and relaxation, the body’s oxygen demands are lower, and the focus shifts towards conserving energy. By constricting the airways, the body reduces the amount of air that enters the lungs, effectively slowing down the respiratory rate. This allows for a more efficient exchange of oxygen and carbon dioxide, ensuring that the body receives an adequate supply of oxygen while minimizing energy expenditure.
In addition to bronchoconstriction, the parasympathetic nervous system also stimulates the production of mucus in the airways. This mucus helps to trap foreign particles, such as dust and bacteria, preventing them from entering the lungs. It also acts as a lubricant, facilitating the smooth passage of air through the airways.
Overall, the vagus nerve and parasympathetic innervation play a vital role in maintaining respiratory function. By regulating bronchoconstriction and mucus production, they ensure that the airways remain clear and functional. Understanding the intricate interplay between the vagus nerve and the respiratory system is crucial for comprehending the impact of vagal tone on respiratory health.
The Vagus Nerve’s Influence on the Airways
When it comes to respiratory health, the vagus nerve’s influence on the airways cannot be underestimated. The vagus nerve exerts control over the smooth muscles that line the bronchial tubes in the lungs, which play a vital role in regulating airflow. Its parasympathetic fibers release acetylcholine, a neurotransmitter that causes bronchoconstriction, leading to a decrease in the diameter of the airways.
Mechanism of Vagus Nerve’s Action on Airways
The mechanism by which the vagus nerve affects the airways is complex and still not fully understood. It is known that the activation of vagal efferent fibers leads to the release of acetylcholine, which binds to specific receptors on the smooth muscle cells of the bronchial tubes. This binding triggers a series of intracellular events that ultimately result in the contraction of the smooth muscles, leading to bronchoconstriction.
However, the influence of the vagus nerve on the airways goes beyond bronchoconstriction. The nerve also plays a crucial role in regulating mucus production, ciliary movement, and inflammatory responses in the airways. Mucus production helps to trap foreign particles and pathogens, preventing them from reaching the deeper parts of the lungs. Ciliary movement, which is the coordinated beating of tiny hair-like structures called cilia, helps to move mucus and trapped particles out of the airways. Inflammatory responses, on the other hand, are important for the body’s defense against infections and other harmful stimuli.
Parasympathetic Innervation and Airways: A Complex Relationship
The parasympathetic innervation of the airways is a finely balanced system. While bronchoconstriction is an essential physiological response to certain stimuli, excessive or prolonged activation of the vagus nerve can lead to undesirable effects such as airway hyperresponsiveness and bronchoconstriction in individuals with respiratory disorders.
For example, in conditions like asthma, where the airways are already inflamed and hyperresponsive, the vagus nerve’s overactivity can exacerbate symptoms. Increased bronchoconstriction and mucus production can further narrow the airways, making breathing difficult. This is why medications that block the action of acetylcholine, such as anticholinergic drugs, are commonly used in the treatment of respiratory disorders to counteract the vagus nerve’s effects.
Understanding the complex relationship between the vagus nerve and the airways is crucial for developing effective treatments for respiratory conditions. Researchers continue to investigate the intricate mechanisms involved in order to find new therapeutic targets and improve the quality of life for individuals with respiratory disorders.
Potential Health Implications of Vagus Nerve Activity on Airways
The intricate connection between the vagus nerve and the airways has significant implications for respiratory health. Understanding how vagus nerve activity can affect the airways may shed light on the development and management of various respiratory disorders.
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It extends from the brainstem to various organs in the body, including the heart, lungs, and gastrointestinal tract. Its role in regulating autonomic functions, such as heart rate, digestion, and respiration, is well-established.
Abnormal vagus nerve activity has been implicated in several respiratory disorders, including asthma, chronic obstructive pulmonary disease (COPD), and bronchitis. Excessive vagal tone can lead to airway hyperresponsiveness, leading to increased sensitivity to environmental triggers and heightened bronchoconstriction.
Asthma, a chronic inflammatory disease of the airways, is characterized by recurrent episodes of wheezing, breathlessness, chest tightness, and coughing. It affects people of all ages and can be triggered by various factors, such as allergens, exercise, and respiratory infections. The vagus nerve’s influence on the airways plays a significant role in asthma pathophysiology, contributing to bronchoconstriction and airway inflammation.
COPD, a progressive lung disease that includes chronic bronchitis and emphysema, is primarily caused by long-term exposure to irritants, such as cigarette smoke. Vagus nerve activity can exacerbate the symptoms of COPD by promoting airway constriction and mucus production. This can lead to persistent coughing, shortness of breath, and reduced lung function.
Bronchitis, an inflammation of the bronchial tubes, can be acute or chronic. In both cases, the vagus nerve’s influence on the airways can contribute to increased bronchial tone and excessive mucus production. This can result in coughing, wheezing, and difficulty breathing.
While the exact mechanisms underlying these conditions are complex and multifactorial, it is clear that the vagus nerve’s influence on the airways plays a significant role. Understanding and potentially modulating vagus nerve activity may open new avenues for the development of innovative therapeutic approaches for these respiratory disorders.
It is worth noting that while these potential implications highlight the importance of vagus nerve activity in respiratory health, individual circumstances may vary. If you have any concerns or are experiencing respiratory symptoms, it is essential to seek professional medical advice and consult with your healthcare provider.
In addition to its impact on respiratory health, the vagus nerve also has a profound influence on cardiovascular function. It plays a crucial role in regulating heart rate, blood pressure, and cardiac output.
Studies have shown that increasing vagal activity through techniques like deep breathing exercises or vagus nerve stimulation can have beneficial effects on cardiovascular health. Vagus nerve stimulation, a therapeutic approach involving the use of electrical impulses to activate the nerve, has been explored as a potential treatment for conditions such as heart failure and arrhythmias.
By modulating vagus nerve activity, it is possible to influence heart rate variability, which is an important indicator of cardiovascular health. Higher heart rate variability is associated with better cardiovascular outcomes, including reduced risk of heart disease and improved overall cardiac function.
However, it is crucial to approach these interventions under the guidance of a healthcare professional to ensure their safety and appropriateness for individual circumstances. Vagus nerve stimulation, for example, is a specialized procedure that requires careful evaluation and monitoring to optimize its effectiveness and minimize potential risks.
In conclusion, the intricate connection between the vagus nerve and the airways has significant implications for respiratory and cardiovascular health. Abnormal vagus nerve activity can contribute to the development and progression of respiratory disorders, while modulating vagus nerve activity may offer new therapeutic possibilities. Further research is needed to fully understand the complex mechanisms underlying these interactions and to develop targeted interventions that can improve respiratory and cardiovascular outcomes.
Therapeutic Approaches Involving the Vagus Nerve and Airways
The complex relationship between the vagus nerve and the airways has prompted researchers to explore therapeutic approaches that target vagus nerve activity. One such approach that shows promise is vagus nerve stimulation (VNS).
Vagus nerve stimulation involves the use of electrical impulses to stimulate the vagus nerve, aiming to modulate its activity. This technique has been approved for use in the treatment of various conditions, including epilepsy and depression. Emerging research suggests that VNS may also have potential applications in respiratory disorders by modulating the vagus nerve’s influence on the airways.
Studies have shown that the vagus nerve plays a crucial role in regulating airway function. It is involved in controlling bronchoconstriction, mucus production, and inflammation in the respiratory system. By targeting the vagus nerve, it is possible to modulate these processes and potentially alleviate symptoms associated with respiratory disorders such as asthma, chronic obstructive pulmonary disease (COPD), and bronchitis.
While VNS holds promise as a potential therapy, further research is needed to determine its safety, efficacy, and optimal clinical applications in the context of respiratory disorders. Clinical trials are underway to evaluate the effectiveness of VNS in improving lung function, reducing airway inflammation, and enhancing overall respiratory health.
Vagus Nerve Stimulation: A Potential Therapy
Vagus nerve stimulation has shown promising results in various medical fields, leading researchers to explore its potential as a therapy for respiratory disorders. By delivering controlled electrical impulses to the vagus nerve, VNS can modulate its activity and influence the airways.
One of the mechanisms through which VNS may benefit respiratory health is by reducing airway hyperresponsiveness. Studies have demonstrated that VNS can decrease the sensitivity of the airways to various triggers, such as allergens or irritants, thereby reducing the frequency and severity of asthma attacks.
Furthermore, VNS has been found to have anti-inflammatory effects in the respiratory system. By modulating the vagus nerve, it is possible to suppress the release of pro-inflammatory molecules and promote the production of anti-inflammatory substances, leading to a reduction in airway inflammation and improved lung function.
It is important to note that VNS is a minimally invasive procedure that involves the implantation of a small device, typically in the chest, which delivers electrical impulses to the vagus nerve. The device can be programmed and adjusted according to the individual’s specific needs and response to therapy.
While VNS holds promise as a potential therapy, it is not without limitations. The long-term effects of VNS on respiratory disorders are still being investigated, and the optimal parameters for stimulation need to be determined. Additionally, the cost and accessibility of VNS devices may pose challenges for widespread adoption.
As always, it is recommended to consult with healthcare professionals to assess the individual suitability and potential benefits of any therapeutic approach. They can provide personalized guidance based on the specific respiratory condition, medical history, and overall health of the patient.
Challenges and Future Directions in Vagus Nerve Therapies
Despite the potential therapeutic benefits of targeting vagus nerve activity in respiratory disorders, there are several challenges that need to be overcome. One of the primary challenges is developing precise and targeted interventions that modulate vagus nerve activity without causing unwanted side effects or disrupting other physiological processes in the body.
Researchers are actively working on improving the precision and specificity of VNS techniques to ensure that the electrical impulses are delivered only to the vagus nerve and do not affect neighboring structures. This involves refining the electrode placement and optimizing the stimulation parameters to achieve the desired therapeutic effects while minimizing potential risks.
Another challenge is understanding the complex interplay between the vagus nerve and the immune system in respiratory disorders. The immune response plays a crucial role in the development and progression of respiratory diseases, and modulating the vagus nerve activity may have implications for immune function. Further research is needed to elucidate these interactions and identify potential targets for therapeutic interventions.
Future research efforts are focused on refining our understanding of the vagus nerve’s role in respiratory health and developing novel therapeutic strategies that harness its potential benefits. These efforts hold promise for improving the management and treatment of respiratory disorders in the future.
Conclusion: The Vagus Nerve and Airways – A Vital Connection
The impact of parasympathetic innervation from the vagus nerve on the airways is an essential aspect of respiratory health. The complex relationship between the vagus nerve and the airways underscores the importance of understanding this connection when it comes to respiratory disorders and potential therapeutic interventions.
While scientific advancements continue to shed light on the intricacies of the vagus nerve’s influence on the airways, it is important to approach any potential therapies or interventions under the guidance of healthcare professionals. They can provide tailored advice and recommendations based on an individual’s specific circumstances.
As researchers continue to unravel the mysteries of the vagus nerve and its impact on the airways, we can look forward to new insights and innovative approaches that may ultimately improve respiratory health for individuals around the world.
If you’re fascinated by the vital role the vagus nerve plays in your respiratory health and are eager to delve deeper into its functions and impact on your overall well-being, “My Vagus Nerve & Me Book” is the perfect resource. Discover the secrets of this remarkable system that regulates everything from your heart rate to your digestion, and learn how to harness its power through natural and artificial stimulation. Embark on a journey to better health and a deeper understanding of your body’s inner workings. Get My Vagus Nerve & Me eBook today and take the first step towards optimizing your vagus nerve’s potential for a healthier, more balanced life.