Panic attacks can be overwhelming and debilitating experiences, causing individuals to feel intense fear and a sense of losing control. While panic attacks are often related to anxiety disorders, recent research has shed light on the potential role of the vagus nerve in their occurrence. The vagus nerve, also known as the “wandering nerve,” is one of the longest and most important nerves in the body. Understanding its anatomy and function is crucial to unraveling its connection to panic attacks.
Understanding the Vagus Nerve
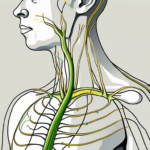
The vagus nerve is a complex network of fibers that originates in the brainstem and extends throughout the body. It is a major part of the autonomic nervous system, which controls involuntary bodily functions such as heart rate, digestion, and respiration. Divided into sensory and motor fibers, the vagus nerve plays a vital role in regulating both physical and emotional well-being.
Anatomy and Function of the Vagus Nerve
The vagus nerve consists of multiple branches that innervate various organs and tissues. It has both sensory and motor functions, relaying information from the body to the brain and vice versa. The sensory fibers of the vagus nerve transmit signals related to touch, temperature, pain, and other bodily sensations, while the motor fibers regulate the function of internal organs, such as the heart, lungs, and digestive system.
Additionally, the vagus nerve is not just a simple nerve, but rather a complex system that interacts with various regions of the brain, including the limbic system, which is responsible for emotions and memory. This intricate connection allows the vagus nerve to influence mood, stress levels, and overall mental well-being.
Furthermore, recent research has shown that the vagus nerve plays a crucial role in the body’s immune response. It has been found to communicate with immune cells, releasing anti-inflammatory substances that help regulate the body’s inflammatory processes. This connection between the vagus nerve and the immune system highlights the importance of this nerve in maintaining overall health and well-being.
The Vagus Nerve and the Autonomic Nervous System
The autonomic nervous system is divided into two branches: the sympathetic nervous system, which prepares the body for action in response to perceived threats, and the parasympathetic nervous system, which promotes relaxation and restoration. The vagus nerve is an essential component of the parasympathetic branch, responsible for maintaining homeostasis and reducing stress.
When the vagus nerve is properly functioning, it helps to regulate heart rate, blood pressure, and the digestive system. However, if its normal functioning is disrupted, it can potentially contribute to the development of panic attacks and anxiety disorders. Understanding the intricate relationship between the vagus nerve and mental health is an area of ongoing research, with potential implications for the development of new treatments for anxiety and mood disorders.
Moreover, the vagus nerve is not only involved in regulating bodily functions but also plays a role in social interactions. It has been found to be involved in the process of bonding and connecting with others. Studies have shown that stimulating the vagus nerve can enhance feelings of empathy and compassion, highlighting its importance in fostering social connections and promoting positive relationships.
In conclusion, the vagus nerve is a fascinating and multifaceted part of the human body. Its intricate network of fibers and its connection to various organs and systems make it a crucial player in maintaining overall health and well-being. Understanding the functions and complexities of the vagus nerve opens up new avenues for research and potential treatments for a wide range of physical and mental health conditions.
The Connection Between the Vagus Nerve and Panic Attacks
Research has indicated a significant interplay between the vagus nerve and panic attacks, providing valuable insights into the potential mechanisms underlying these episodes.
The Role of the Vagus Nerve in Anxiety Disorders
Anxiety disorders, including panic disorder, have been associated with dysregulation of the autonomic nervous system, particularly the vagus nerve. Studies have shown that individuals with anxiety disorders may exhibit increased vagal activity at rest, leading to heightened physiological responses to stressors.
In addition to its role in anxiety disorders, the vagus nerve is also involved in regulating various bodily functions, such as heart rate, digestion, and inflammation. This nerve acts as a communication highway between the brain and the body, transmitting signals and influencing the overall state of the body’s internal environment.
When the vagus nerve is functioning optimally, it helps maintain a state of calm and relaxation. However, in individuals with anxiety disorders, this delicate balance can be disrupted, leading to an overactive vagus nerve.
It is important to note that the vagus nerve is not solely responsible for the development of panic attacks. Panic attacks are complex and multifaceted, with various psychological, genetic, and environmental factors contributing to their occurrence.
How Panic Attacks Affect the Vagus Nerve
Panic attacks themselves can impact the vagus nerve, further exacerbating symptoms and perpetuating a cycle of anxiety. During a panic attack, the sympathetic nervous system becomes overactivated, leading to a surge of stress hormones such as adrenaline.
This hormonal response can affect the function of the vagus nerve, resulting in increased heart rate, palpitations, shortness of breath, and gastrointestinal discomfort. These physical symptoms, in turn, can intensify the feelings of fear and anxiety, potentially triggering a vicious cycle of panic.
Furthermore, research has shown that chronic stress and anxiety can lead to long-term alterations in vagal tone, which refers to the activity level of the vagus nerve. Prolonged periods of heightened vagal activity can contribute to a state of hyperarousal, making individuals more susceptible to experiencing panic attacks.
Understanding the intricate relationship between the vagus nerve and panic attacks is crucial for developing effective treatment strategies. By targeting the dysregulation of the vagus nerve, healthcare professionals can help individuals manage their anxiety symptoms and reduce the frequency and intensity of panic attacks.
Therapeutic approaches such as vagus nerve stimulation, cognitive-behavioral therapy, and relaxation techniques have shown promise in modulating vagal activity and improving overall well-being in individuals with panic disorder.
It is important to consult with a healthcare professional for a comprehensive evaluation and personalized treatment plan if you or someone you know is struggling with panic attacks or anxiety disorders.
The Influence of Cold Exposure on the Vagus Nerve
Cold exposure has long been recognized for its various physiological effects on the body, including its potential influence on the vagus nerve.
The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body. It plays a crucial role in regulating many bodily functions, including heart rate, digestion, and respiratory rate. The vagus nerve is part of the parasympathetic branch of the autonomic nervous system, which is responsible for promoting relaxation and maintaining homeostasis.
Physiological Responses to Cold
When exposed to cold temperatures, the body undergoes several adaptive responses. Blood vessels constrict, redirecting blood flow to vital organs to maintain core body temperature. This vasoconstriction helps to conserve heat and prevent excessive heat loss from the body’s surface.
In addition to vasoconstriction, the body’s heart rate and blood pressure may increase temporarily in response to cold exposure. This physiological response is a natural mechanism to ensure that enough oxygen and nutrients are delivered to the body’s tissues and organs. The increased heart rate and blood pressure help to compensate for the reduced blood flow caused by vasoconstriction.
Furthermore, cold exposure stimulates the sympathetic nervous system, which is responsible for activating the body’s fight-or-flight response. This response prepares the body for potential danger by increasing alertness, sharpening focus, and releasing stress hormones such as adrenaline and cortisol.
It is important to note that while the sympathetic nervous system is essential for survival in threatening situations, chronic activation of this system can have detrimental effects on overall health and well-being. This is where the influence of cold exposure on the vagus nerve becomes particularly interesting.
Cold Stimulation and the Vagus Nerve
Recent studies have suggested that cold stimulation, such as applying ice to specific areas of the body, may influence the vagus nerve and potentially mitigate panic symptoms.
It is hypothesized that the cold sensation triggers a physiological response that can help override the sympathetic overactivation associated with panic attacks. By stimulating the vagus nerve, cold exposure may activate the parasympathetic branch of the autonomic nervous system, promoting relaxation and a sense of calm.
Furthermore, cold exposure has been found to increase the production of certain neurotransmitters, such as norepinephrine and dopamine, which are involved in mood regulation. These neurotransmitters play a crucial role in modulating the activity of the vagus nerve and can contribute to the overall calming effect of cold stimulation.
Moreover, cold exposure has also been shown to have anti-inflammatory effects on the body. Inflammation is a natural immune response that helps the body fight off infections and heal injuries. However, chronic inflammation can lead to various health conditions, including cardiovascular disease and autoimmune disorders. Cold exposure has been found to reduce inflammation by suppressing the production of pro-inflammatory cytokines, which are signaling molecules involved in the inflammatory response.
Overall, the influence of cold exposure on the vagus nerve is a fascinating area of research that has the potential to provide insights into the development of new therapeutic approaches for various conditions, including anxiety disorders, depression, and chronic inflammation. Further studies are needed to fully understand the mechanisms underlying this influence and to explore its potential clinical applications.
Ice as a Tool in Panic Attack Management
The use of ice as a tool in panic attack management has gained attention in recent years, with proponents suggesting its potential benefits in reducing panic symptoms.
Panic attacks can be debilitating, causing intense fear and physical symptoms such as rapid heartbeat, shortness of breath, and dizziness. Finding effective strategies to manage panic attacks is crucial for individuals who experience them.
The Science Behind Ice and Panic Attacks
While the exact mechanisms behind the use of ice in panic attack management remain unclear, many individuals report a subjective reduction in panic symptoms when applying ice to specific areas such as the face, back of the neck, or wrists.
It is believed that the ice may act as a sensory distraction, diverting attention away from the panic symptoms and potentially triggering a parasympathetic response through vagal stimulation. The vagus nerve, which runs from the brain to various organs in the body, plays a role in regulating heart rate, digestion, and other bodily functions. By stimulating the vagus nerve, ice may help activate the body’s relaxation response, counteracting the heightened physiological arousal associated with panic attacks.
However, further research is needed to fully understand the physiological effects of ice on the vagus nerve and its role in panic attack management. Scientists are exploring the potential benefits of cold therapy, including ice, in various areas of mental health, but more studies are required to establish its efficacy and safety.
Practical Applications of Ice in Panic Attack Treatment
While ice may provide temporary relief for some individuals experiencing panic attacks, it is important to emphasize that it is not a substitute for professional medical care. Panic attacks can have underlying causes that require comprehensive evaluation and treatment.
If you experience recurrent panic attacks or anxiety symptoms, it is crucial to consult with a healthcare professional who can provide an accurate diagnosis and develop an appropriate treatment plan. They can help address the root causes of panic attacks and guide you towards evidence-based interventions that may include cognitive-behavioral therapies, medications, and lifestyle modifications.
In addition to seeking professional help, individuals may find it beneficial to explore various self-help strategies to manage panic attacks. These can include deep breathing exercises, progressive muscle relaxation, mindfulness meditation, and engaging in activities that promote relaxation and stress reduction.
It is also important to create a supportive network of friends, family, or support groups who can provide understanding and encouragement during panic attacks. Having someone to talk to and lean on during difficult moments can make a significant difference in managing panic symptoms.
Furthermore, maintaining a healthy lifestyle can contribute to overall well-being and potentially reduce the frequency and intensity of panic attacks. Regular exercise, adequate sleep, a balanced diet, and avoiding excessive caffeine and alcohol consumption are all factors that can positively impact mental health.
While ice may offer a temporary respite from panic symptoms for some individuals, it is crucial to approach panic attack management holistically. By combining professional guidance, self-help strategies, and a healthy lifestyle, individuals can work towards effectively managing panic attacks and improving their overall quality of life.
Future Research and Potential Implications
The emerging research exploring the interplay between the vagus nerve, cold exposure, and panic attacks opens up exciting possibilities for future investigations.
Understanding the intricate connections between the vagus nerve and panic attacks is crucial for developing effective treatments and improving the lives of individuals affected by panic disorder. By delving deeper into this area of research, scientists hope to uncover new insights into the underlying mechanisms and potential therapeutic interventions.
Unanswered Questions in the Field
Despite the advances in our understanding, there are still many unanswered questions regarding the precise mechanisms through which the vagus nerve influences panic attacks and how cold exposure may modulate its activity. Further research is needed to unravel these complexities and shed light on the potential role of the vagus nerve in panic disorder.
One of the key questions that researchers are grappling with is how the vagus nerve communicates with the brain to trigger panic attacks. Is there a specific pathway or set of neurotransmitters involved in this process? Additionally, scientists are interested in exploring the potential genetic and environmental factors that may interact with the vagus nerve to increase the risk of panic disorder.
Moreover, the relationship between cold exposure and the vagus nerve remains a topic of ongoing investigation. While some studies have suggested that cold exposure may activate the vagus nerve and potentially reduce the frequency or severity of panic attacks, the underlying mechanisms are not yet fully understood. Researchers are keen to explore the physiological changes that occur during cold exposure and how they may impact the vagus nerve’s activity.
The Potential for New Treatment Approaches
As more research is conducted, new treatment approaches targeting the vagus nerve may emerge. These approaches could potentially harness the modulation of the vagus nerve activity through techniques such as cold exposure or other non-invasive interventions.
One potential avenue for intervention is the use of transcutaneous vagus nerve stimulation (tVNS), a non-invasive technique that involves applying electrical stimulation to the skin overlying the vagus nerve. Preliminary studies have shown promising results in reducing panic symptoms and improving overall well-being. However, further research is needed to determine the optimal parameters and long-term effects of tVNS.
Another area of interest is the potential use of biofeedback techniques to train individuals to regulate their vagus nerve activity. By providing real-time feedback on physiological markers associated with vagal tone, such as heart rate variability, individuals may learn to modulate their own nervous system and reduce the occurrence of panic attacks.
However, until more evidence is available, it is crucial to approach these potential treatments with caution and under the guidance of healthcare professionals. Individual experiences and responses to different interventions may vary, and what works for one person may not work for another.
Furthermore, it is important to consider the potential ethical implications and long-term effects of interventions targeting the vagus nerve. As with any medical intervention, a comprehensive understanding of the risks and benefits is necessary to ensure the well-being of patients.
The impact of the vagus nerve on panic attacks and the potential influence of cold exposure is an exciting area of research that holds promise for understanding and managing this debilitating condition. By continuing to investigate the intricate connections between the vagus nerve, panic attacks, and therapeutic interventions, we hope to develop more effective treatments and improve the lives of individuals affected by panic disorder.
If you’re intrigued by the profound impact the vagus nerve has on your health and are seeking to deepen your understanding, “My Vagus Nerve & Me Book” is an essential resource. This comprehensive guide will take you on a journey through the complexities of one of the most vital systems in your body. Discover how to naturally and artificially stimulate your vagus nerve, enhancing your immune system, digestion, heart rate, and mental health. Embrace the opportunity to learn about its role in liver detoxification, bile production, blood sugar regulation, and much more. Ready to unlock the secrets of your well-being? Get My Vagus Nerve & Me eBook today and take the first step towards harnessing the power of your vagus nerve.