Hiatal hernia is a medical condition that affects the upper part of the stomach, causing it to move up into the chest through the diaphragm. This can have various impacts on the surrounding organs and systems, including the vagus nerve. In this comprehensive guide, we will explore the connection between hiatal hernia and the vagus nerve, as well as understanding the condition, treatment options, and prevention methods.
Understanding Hiatal Hernia
Hiatal hernia occurs when the stomach bulges through the diaphragm, a large muscle that separates the chest cavity from the abdomen. This condition can be classified into two types: sliding hiatal hernia, where the stomach and the junction of the esophagus slide up into the chest, and paraesophageal hiatal hernia, where a part of the stomach pushes alongside the esophagus, remaining in the chest.
Hiatal hernia is a fascinating medical condition that affects many individuals worldwide. It is important to delve deeper into the definition, causes, symptoms, and diagnosis of this condition to gain a comprehensive understanding.
Definition and Causes of Hiatal Hernia
Hiatal hernia is a condition that occurs when the upper part of the stomach protrudes through the diaphragm into the chest cavity. This abnormality can be caused by a combination of factors, making it a complex condition to fully comprehend.
One of the primary causes of hiatal hernia is weak supporting tissues in the diaphragm. These tissues may become weakened over time due to factors such as aging, genetic predisposition, or connective tissue disorders. Additionally, excessive pressure on the abdomen can contribute to the development of hiatal hernia. This pressure can be a result of obesity, pregnancy, or certain lifestyle choices like smoking or heavy lifting.
Understanding the causes of hiatal hernia is crucial in order to prevent its occurrence or manage its symptoms effectively. By addressing the underlying factors that contribute to this condition, individuals can take proactive steps towards their well-being.
Symptoms and Diagnosis of Hiatal Hernia
The symptoms of hiatal hernia can vary from person to person, making it essential to recognize the signs and seek appropriate medical attention. While some individuals may experience mild discomfort, others may face more severe symptoms that significantly impact their quality of life.
One of the most common symptoms of hiatal hernia is heartburn or acid reflux. This occurs when stomach acid flows back into the esophagus, causing a burning sensation in the chest. Chest pain is another prevalent symptom, often mistaken for a heart attack due to its intensity.
Difficulty swallowing, known as dysphagia, is also a symptom of hiatal hernia. Individuals may find it challenging to pass food or liquids through the esophagus, leading to discomfort and frustration. Regurgitation of food or liquids, belching, and feeling fullness or bloating after eating are additional symptoms that can manifest in individuals with hiatal hernia.
Diagnosing hiatal hernia involves a thorough evaluation by a medical professional. A physical examination, combined with a review of the patient’s medical history, helps in identifying potential risk factors and symptoms. Diagnostic tests such as endoscopy, X-ray, or CT scan may also be recommended to visualize the hernia and determine its severity.
Overall, understanding the symptoms and diagnosis of hiatal hernia is crucial for early detection and appropriate treatment. By recognizing the signs and seeking medical guidance, individuals can embark on a path towards managing their condition effectively.
The Vagus Nerve Explained
The vagus nerve is a vital part of the nervous system. It is the longest cranial nerve and controls many essential functions such as heart rate, digestion, breathing, and even emotional state. This nerve serves as a communication pathway between the brain and various organs, including the stomach and intestines.
The vagus nerve, also known as the tenth cranial nerve, is a complex network of fibers that extends from the brainstem to various parts of the body. It is responsible for transmitting signals between the brain and the organs, allowing for the regulation of important bodily functions.
Role and Function of the Vagus Nerve
The vagus nerve plays a crucial role in regulating the digestive process. It helps stimulate the release of stomach acids and digestive enzymes, controls the movements of the gastrointestinal tract, and provides sensory information back to the brain regarding the state of the digestive system.
When we eat, the vagus nerve is responsible for sending signals to the brain, informing it about the amount of food consumed and the state of the digestive system. This feedback loop allows the brain to adjust the production of digestive enzymes and stomach acids accordingly, ensuring efficient digestion.
Furthermore, the vagus nerve also plays a role in controlling heart rate and blood pressure. It helps to regulate the parasympathetic nervous system, which is responsible for promoting rest and relaxation. When the vagus nerve is activated, it slows down the heart rate, allowing the body to conserve energy and maintain a state of calm.
Disorders Related to the Vagus Nerve
Various disorders can affect the vagus nerve, leading to disturbances in digestive function. These include gastroparesis, a condition where the stomach empties too slowly, and achalasia, a disorder that affects the ability of the esophagus to move food into the stomach. These conditions can cause symptoms similar to those experienced with hiatal hernia.
Gastroparesis occurs when the vagus nerve is damaged or doesn’t function properly. This can result in delayed emptying of the stomach, leading to symptoms such as nausea, vomiting, bloating, and a feeling of fullness even after eating small amounts of food. Treatment for gastroparesis may involve dietary changes, medications to stimulate stomach contractions, or in severe cases, surgical intervention.
Achalasia, on the other hand, is a rare disorder that affects the muscles of the esophagus and the lower esophageal sphincter. When the vagus nerve is not functioning correctly, the muscles in the esophagus can’t push food into the stomach effectively. This can cause difficulty swallowing, chest pain, regurgitation of food, and weight loss. Treatment for achalasia may involve medications to relax the esophageal muscles, balloon dilation to widen the esophagus, or surgery to remove or modify the lower esophageal sphincter.
It is important to note that while disorders related to the vagus nerve can be challenging to manage, there are treatment options available. Consulting with a healthcare professional is crucial for an accurate diagnosis and appropriate treatment plan.
The Connection between Hiatal Hernia and the Vagus Nerve
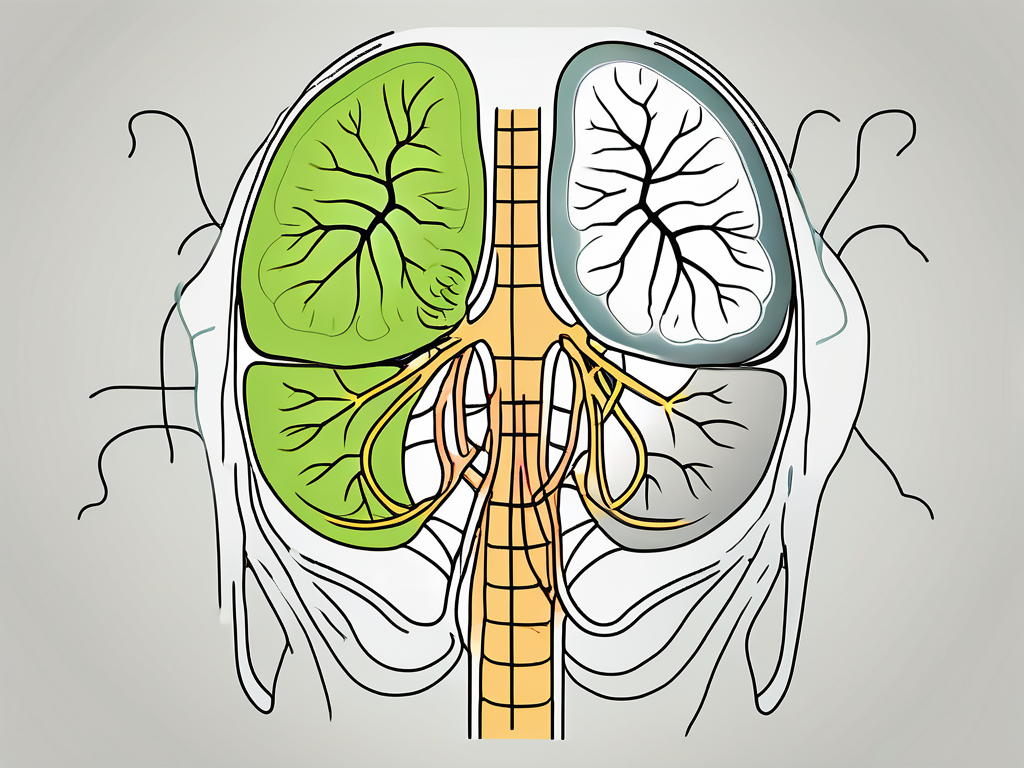
Hiatal hernia is a condition in which the stomach protrudes through the diaphragm, causing a variety of symptoms and complications. While hiatal hernia itself does not directly damage the vagus nerve, its presence can cause mechanical pressure or irritation on the nerve. This can disrupt the normal function of the vagus nerve and lead to a variety of symptoms and complications.
The vagus nerve, also known as the “wandering nerve,” is an important part of the autonomic nervous system. It plays a crucial role in regulating various bodily functions, including digestion, heart rate, and breathing. When the stomach moves upward through the diaphragm, it can put pressure on the vagus nerve, interfering with its ability to transmit signals properly.
This interference can result in a range of symptoms. One common symptom is heartburn, which occurs when stomach acid flows back into the esophagus due to the malfunctioning of the vagus nerve. Difficulty swallowing, known as dysphagia, is another symptom that can occur when the vagus nerve is affected by hiatal hernia. Abnormal gastric motility, characterized by delayed emptying of the stomach or irregular contractions, can also be a result of vagus nerve dysfunction caused by hiatal hernia.
Potential Complications and Risks
In some cases, hiatal hernia can lead to complications that further impact the vagus nerve and digestive function. One such complication is gastroesophageal reflux disease (GERD), a chronic condition in which stomach acid regularly flows back into the esophagus. The pressure exerted on the vagus nerve by the herniated stomach can contribute to the development or worsening of GERD symptoms.
Another potential complication is esophagitis, which is inflammation of the esophagus. When the vagus nerve is affected by hiatal hernia, it can disrupt the normal functioning of the lower esophageal sphincter, a muscular valve that prevents stomach acid from entering the esophagus. This can lead to irritation and inflammation of the esophageal lining, causing symptoms such as chest pain, difficulty swallowing, and a burning sensation in the throat.
In rare cases, hiatal hernia can contribute to the development of a condition called Barrett’s esophagus. This condition occurs when the lining of the esophagus undergoes changes, becoming more similar to the lining of the intestines. Barrett’s esophagus is associated with an increased risk of esophageal cancer, and the mechanical pressure on the vagus nerve caused by hiatal hernia may play a role in its development.
In conclusion, while hiatal hernia itself does not directly damage the vagus nerve, its presence can cause mechanical pressure or irritation on the nerve, leading to a variety of symptoms and complications. Understanding the connection between hiatal hernia and the vagus nerve is crucial in managing and treating this condition effectively.
Treatment Options for Hiatal Hernia Impacting the Vagus Nerve
Treatment for hiatal hernia aims to relieve symptoms, prevent complications, and improve overall quality of life. The approach may vary depending on the severity of the hernia and the specific symptoms experienced.
Hiatal hernia occurs when a portion of the stomach pushes through the diaphragm and into the chest cavity. This can put pressure on the vagus nerve, which is responsible for regulating various bodily functions, including digestion. When the vagus nerve is impacted by the hernia, it can lead to symptoms such as acid reflux, chest pain, difficulty swallowing, and even respiratory issues.
Medical Treatments and Surgical Procedures
Medical treatments for hiatal hernia often focus on managing associated symptoms. This may include medications to reduce acid reflux, relieve pain, or improve gastric motility. Proton pump inhibitors (PPIs) are commonly prescribed to reduce the production of stomach acid and alleviate symptoms of acid reflux. Pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), may also be recommended to manage discomfort.
In some cases, surgical intervention may be necessary to address the hiatal hernia and its impact on the vagus nerve. Hernia repair surgery involves pushing the stomach back into its proper position and reinforcing the weakened diaphragm muscles. This can help alleviate pressure on the vagus nerve and improve symptoms. Another surgical procedure called fundoplication may be performed, which involves wrapping the upper part of the stomach around the lower esophagus to strengthen the valve between the esophagus and the stomach, preventing acid reflux.
Lifestyle Changes and Home Remedies
For mild cases of hiatal hernia, lifestyle modifications can be effective in managing symptoms and reducing the impact on the vagus nerve. These may include maintaining a healthy weight, as excess weight can put additional pressure on the diaphragm and worsen the hernia. Avoiding trigger foods or beverages, such as spicy or fatty foods, caffeine, and alcohol, can help reduce the occurrence of acid reflux and alleviate symptoms.
Eating smaller, more frequent meals instead of large meals can also help prevent excessive pressure on the stomach and reduce the likelihood of acid reflux. It is also recommended to avoid lying down or going to bed immediately after eating, as this can contribute to acid reflux. Raising the head of the bed by using a wedge pillow or elevating the head of the bed can help keep stomach acid from flowing back into the esophagus during sleep.
In addition to dietary and positional changes, practicing stress management techniques can be beneficial for individuals with hiatal hernia impacting the vagus nerve. Stress and anxiety can exacerbate symptoms and increase the likelihood of acid reflux. Engaging in activities such as yoga, meditation, deep breathing exercises, or seeking therapy can help reduce stress levels and improve overall well-being.
However, it is important to consult with a healthcare professional before attempting any home remedies or making significant lifestyle changes. They can provide personalized recommendations based on the severity of the hiatal hernia and the individual’s overall health.
Preventing Hiatal Hernia and Protecting the Vagus Nerve
Hiatal hernia is a condition where a portion of the stomach pushes through the diaphragm into the chest cavity. While it may not be possible to completely prevent hiatal hernia, certain measures can help reduce the risk and protect the vagus nerve from potential complications.
The vagus nerve is an important part of the autonomic nervous system, responsible for controlling various bodily functions, including digestion. When a hiatal hernia occurs, it can put pressure on the vagus nerve, leading to symptoms such as heartburn, difficulty swallowing, and chest pain.
Diet and Exercise Recommendations
One of the key ways to reduce the risk of hiatal hernia is by making dietary and lifestyle changes. Avoiding large meals, spicy or fatty foods, and carbonated beverages can help prevent excessive pressure on the stomach and reduce the likelihood of a hernia occurring. These foods can cause the stomach to produce more acid, leading to heartburn and increasing the risk of herniation.
Staying physically active is also crucial for maintaining abdominal health. Regular exercise helps strengthen the muscles of the abdomen, including the diaphragm, which plays a significant role in preventing herniation. Engaging in activities such as walking, swimming, or yoga can contribute to overall abdominal strength and minimize the strain on the diaphragm.
In addition to exercise, maintaining a healthy weight is essential for preventing hiatal hernia. Excess weight can put additional pressure on the abdomen, increasing the risk of herniation. By adopting a balanced diet and engaging in regular physical activity, individuals can achieve and maintain a healthy weight, reducing the strain on the diaphragm and minimizing the chances of developing a hiatal hernia.
Practicing good posture is another important aspect of preventing hiatal hernia. Slouching or hunching over can compress the abdomen and increase the likelihood of herniation. Maintaining an upright posture while sitting and standing can help keep the organs in their proper position and reduce the risk of a hernia.
Regular Check-ups and Early Detection
While preventive measures can significantly reduce the risk of hiatal hernia, regular medical check-ups are crucial for early detection and management. During routine examinations, healthcare professionals can assess the overall health of the abdomen and identify any signs of herniation or related conditions.
If you experience persistent symptoms such as heartburn, difficulty swallowing, or chest pain, it is essential to consult with a healthcare professional for proper evaluation and diagnosis. These symptoms may indicate the presence of a hiatal hernia or other underlying conditions that require medical attention.
Early detection of hiatal hernia allows for timely intervention and appropriate treatment. Depending on the severity of the hernia, treatment options may include lifestyle modifications, medication, or, in severe cases, surgical intervention. Regular check-ups and open communication with healthcare professionals ensure that any potential issues are addressed promptly, minimizing the risk of complications and promoting overall abdominal health.
Conclusion: Living with Hiatal Hernia and Vagus Nerve Impact
Coping with hiatal hernia and its impact on the vagus nerve requires a multidimensional approach. While treatment options exist to manage symptoms and prevent complications, it is crucial to understand that each individual may experience the condition differently.
Coping Mechanisms and Support
Seeking support from healthcare professionals, joining support groups, and implementing stress reduction techniques can all aid in coping with the challenges presented by hiatal hernia. Additionally, maintaining a positive outlook, following the recommended treatment plan, and making necessary lifestyle adjustments can contribute to a better quality of life.
Future Research and Developments
Ongoing research continues to explore the relationship between hiatal hernia and the vagus nerve. As we deepen our understanding of how these conditions interact, we can expect advancements in diagnostic techniques, treatment options, and preventive measures. It is imperative for healthcare professionals and researchers to collaborate to improve the care and management of individuals affected by hiatal hernia.
In conclusion, hiatal hernia can impact the vagus nerve and disrupt various functions of the digestive system. Understanding the connection between these two components is essential for accurate diagnosis, effective treatment, and overall well-being. If you suspect you may have a hiatal hernia or are experiencing symptoms related to the condition, it is advisable to consult with a healthcare professional promptly. With proper care and management, individuals can maintain a good quality of life and minimize the impact of hiatal hernia on the vagus nerve.
If you’re intrigued by the vital role the vagus nerve plays in your health and are eager to learn more about how to nurture this critical nerve, “My Vagus Nerve & Me Book” is the perfect resource for you. Delve into the fascinating world of the vagus nerve with our comprehensive guide, where you’ll discover its intricate functions and the natural and artificial ways to stimulate it for optimal health. Whether you’re dealing with a hiatal hernia or simply want to enhance your well-being, understanding the vagus nerve is a step towards a healthier life. Get My Vagus Nerve & Me eBook today and embark on a journey to better health!