Gabapentin is a medication that has gained recognition for its potential impact on the vagus nerve. In this comprehensive analysis, we will delve into the various aspects of this topic to better understand the potential implications and therapeutic applications of gabapentin.
Understanding Gabapentin and Its Uses
Gabapentin is an anticonvulsant medication primarily used to treat seizures and certain types of nerve pain. It works by modulating the activity of certain neurotransmitters, particularly gamma-aminobutyric acid (GABA), in the brain. While primarily used as an antiepileptic drug, gabapentin has also shown promise in treating other conditions such as fibromyalgia and restless leg syndrome.
When it comes to the pharmacology of gabapentin, there is much to explore. The drug’s mechanism of action is intriguing and worth understanding in detail. Gabapentin is structurally similar to GABA, the major inhibitory neurotransmitter in the brain, but it does not bind to GABA receptors. Instead, it binds to the α2δ subunit of voltage-gated calcium channels in the central nervous system. This unique binding mechanism allows gabapentin to inhibit the release of various excitatory neurotransmitters, such as glutamate, thereby reducing neuronal excitability.
Furthermore, the medical applications of gabapentin extend beyond its primary uses for seizures and nerve pain. Researchers and healthcare professionals have discovered its potential in managing other medical conditions. For instance, gabapentin has been found to be effective in treating neuropathic pain associated with diabetes, postherpetic neuralgia, and chronic pain conditions. Its ability to modulate neurotransmitter release makes it a valuable tool in alleviating the discomfort and distress caused by these conditions.
Interestingly, gabapentin has also been explored as an adjunctive therapy for psychiatric disorders. Anxiety disorders, such as generalized anxiety disorder and social anxiety disorder, have been the focus of studies investigating the effectiveness of gabapentin. Preliminary findings suggest that gabapentin may help reduce anxiety symptoms and improve overall well-being in individuals with these disorders. Additionally, it has shown potential as a treatment option for bipolar disorder, a complex mood disorder characterized by alternating episodes of mania and depression. By targeting neuronal excitability, gabapentin may help stabilize mood and reduce the severity of bipolar symptoms.
Moreover, gabapentin has been studied as a potential treatment for insomnia, a common sleep disorder that affects millions of people worldwide. Insomnia can have a significant impact on an individual’s quality of life, leading to daytime sleepiness, impaired cognitive function, and reduced productivity. Gabapentin’s ability to modulate neurotransmitter release and promote relaxation may make it a valuable option for individuals struggling with sleep disturbances.
In conclusion, while gabapentin is primarily used as an anticonvulsant and for nerve pain, its pharmacology and medical applications go beyond these initial indications. Its unique mechanism of action, targeting voltage-gated calcium channels, allows it to modulate neurotransmitter release and reduce neuronal excitability. This versatility has led to its exploration in various medical conditions, including neuropathic pain, psychiatric disorders, and insomnia. As research continues, gabapentin may prove to be an even more valuable tool in the field of medicine.
The Vagus Nerve: An Overview
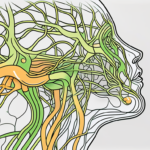
The vagus nerve, also known as the tenth cranial nerve, is a significant component of the autonomic nervous system. It extends from the brainstem to various organs in the body, including the heart, lungs, liver, and digestive tract. As a key player in the parasympathetic division of the autonomic nervous system, the vagus nerve is responsible for regulating numerous bodily functions.
The vagus nerve, with its extensive reach throughout the body, plays a crucial role in maintaining optimal health and well-being. Let’s delve deeper into the anatomy and functions of this remarkable nerve.
Anatomy and Functions of the Vagus Nerve
The vagus nerve consists of both motor and sensory fibers. Its motor fibers control the muscles involved in speech, swallowing, and the muscles of the digestive tract. These motor functions allow us to communicate, consume nourishment, and ensure the proper breakdown and absorption of nutrients.
On the other hand, the sensory fibers of the vagus nerve transmit information from various organs to the brain. This two-way communication enables the brain to receive vital feedback from the body and respond accordingly. The vagus nerve’s sensory functions are responsible for regulating heart rate, breathing, digestion, and other essential processes that keep our bodies functioning optimally.
Imagine a well-orchestrated symphony, where each instrument plays its part to create a harmonious melody. Similarly, the vagus nerve coordinates the various bodily functions, ensuring they work together seamlessly to maintain homeostasis.
Role of the Vagus Nerve in the Nervous System
As a critical part of the parasympathetic nervous system, the vagus nerve helps maintain homeostasis by counterbalancing the sympathetic division’s fight-or-flight response. While the sympathetic nervous system prepares the body for action and survival, the parasympathetic nervous system, led by the vagus nerve, promotes rest and relaxation.
One of the primary functions of the vagus nerve is to stimulate digestion. When we eat, the vagus nerve sends signals to the digestive organs, triggering the release of digestive enzymes and promoting the movement of food through the gastrointestinal tract. This intricate dance of signals ensures that our bodies efficiently extract nutrients from the food we consume.
Moreover, the vagus nerve plays a vital role in regulating heart rate. It acts as a natural pacemaker, sending electrical signals to the heart to maintain a steady rhythm. By modulating heart rate, the vagus nerve helps keep blood pressure in check and ensures adequate blood flow to all parts of the body.
Interestingly, the vagus nerve is also involved in the communication between the gut and the brain. This bidirectional pathway, known as the gut-brain axis, allows the gut to send signals to the brain, influencing mood, cognition, and overall well-being. The vagus nerve acts as a messenger, transmitting information about the gut’s state to the brain, which in turn influences our emotional and mental states.
In conclusion, the vagus nerve is a remarkable component of the autonomic nervous system, with far-reaching effects on our overall health and well-being. Its intricate network of motor and sensory fibers ensures the smooth functioning of various bodily processes, from digestion to heart rate regulation. Understanding the role of the vagus nerve can provide valuable insights into maintaining a healthy and balanced lifestyle.
The Interaction between Gabapentin and the Vagus Nerve
With a basic understanding of gabapentin and the vagus nerve established, let us explore how these two entities interact and what potential effects gabapentin may have on the vagus nerve.
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions, including heart rate, digestion, and inflammation. It is a complex network of fibers that extends from the brainstem to different organs in the body. Gabapentin, on the other hand, is a medication primarily used to treat seizures and neuropathic pain.
Mechanism of Gabapentin’s Impact on the Vagus Nerve
While the exact mechanisms through which gabapentin affects the vagus nerve are not yet fully understood, researchers have proposed several theories. One hypothesis suggests that gabapentin’s modulation of neurotransmitter release, particularly gamma-aminobutyric acid (GABA), may indirectly influence vagal activity. GABA is an inhibitory neurotransmitter that helps regulate neuronal excitability.
Another theory proposes that gabapentin may enhance the function of potassium channels in the vagus nerve. By increasing the flow of potassium ions, gabapentin could potentially promote vagal tone, leading to a state of relaxation and improved regulation of bodily functions.
Furthermore, studies have shown that gabapentin may have anti-inflammatory effects. Inflammation can negatively impact vagal function, and by reducing inflammation, gabapentin could potentially improve vagal activity.
Potential Therapeutic Implications
Given its possible impact on the vagus nerve, gabapentin’s therapeutic potential extends beyond its primary indications. Preliminary studies have shown promising results in utilizing gabapentin as an adjunctive treatment for conditions associated with impaired vagal function, such as epilepsy, depression, and anxiety disorders.
For individuals with epilepsy, gabapentin’s ability to modulate neuronal excitability and potentially increase vagal tone may help reduce the frequency and severity of seizures. Similarly, in individuals with depression or anxiety disorders, gabapentin’s potential to promote relaxation and regulate bodily functions through vagal stimulation could offer additional benefits.
However, it is important to note that further research is needed to establish the efficacy and safety of gabapentin in these off-label uses. Clinical trials and long-term studies are necessary to fully understand the potential therapeutic implications of gabapentin’s interaction with the vagus nerve.
In conclusion, while the exact mechanisms and therapeutic implications of gabapentin’s impact on the vagus nerve are still being explored, the current understanding suggests that gabapentin may have a positive influence on vagal activity. This opens up new possibilities for utilizing gabapentin in the treatment of various conditions associated with vagal dysfunction. Continued research in this field will help shed more light on the potential benefits and limitations of gabapentin in modulating vagal function.
Analyzing the Clinical Impact of Gabapentin on the Vagus Nerve
As we delve into the clinical impact of gabapentin on the vagus nerve, it is essential to review the relevant medical literature and interpret the findings cautiously.
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions, including heart rate, digestion, and inflammation. It is a complex network of fibers that connects the brain to different organs throughout the body. Understanding the potential impact of gabapentin on this important nerve has garnered significant attention in the medical community.
Reviewing Relevant Medical Literature
Several studies have explored the potential benefits of gabapentin on vagal activity and associated health conditions. One study conducted on animal models demonstrated that gabapentin administration increased vagal tone, leading to improved heart rate variability and reduced inflammation. These findings suggest that gabapentin may have a positive impact on vagal function.
In addition to animal studies, human trials have also been conducted to investigate the effects of gabapentin on the vagus nerve. A randomized controlled trial involving patients with epilepsy found that gabapentin treatment resulted in increased vagal activity, leading to a reduction in seizure frequency. This suggests that gabapentin may have therapeutic implications for certain neurological conditions.
However, it is important to note that not all studies have reported positive outcomes. Some research has shown conflicting results, highlighting the need for further investigation. The limitations and variances in methodologies across different studies also emphasize the importance of conducting more rigorous research to establish a clear understanding of the relationship between gabapentin and the vagus nerve.
Interpreting the Findings
While research has shown potential therapeutic implications of gabapentin on the vagus nerve, it is important to remember that findings are not conclusive. The effects of gabapentin may vary depending on the individual and the specific health condition being treated.
Consulting with a healthcare professional, such as a neurologist, is crucial to determine whether gabapentin may be an appropriate treatment option for specific conditions. These professionals can provide personalized guidance based on a thorough assessment of individual needs and medical history. They can weigh the potential benefits and risks of gabapentin and consider alternative treatment options, ensuring the best possible outcome for each patient.
Furthermore, it is worth noting that gabapentin is not without its side effects. Common side effects include dizziness, drowsiness, and fatigue. Rare but serious side effects may include allergic reactions and suicidal thoughts. Therefore, careful monitoring and regular follow-up with a healthcare professional are essential when using gabapentin as a treatment option.
In conclusion, while the clinical impact of gabapentin on the vagus nerve shows promise, further research is needed to fully understand its potential benefits and limitations. The relationship between gabapentin and the vagus nerve is complex, and individual responses may vary. Consulting with a healthcare professional is crucial to make informed decisions regarding the use of gabapentin as a treatment option for specific conditions.
Risks and Side Effects of Gabapentin on the Vagus Nerve
Like any medication, gabapentin carries potential risks and side effects that need to be considered before starting treatment.
Gabapentin is a commonly prescribed medication used to treat various conditions, including epilepsy, neuropathic pain, and restless leg syndrome. While it can be highly effective in managing these conditions, it is important to be aware of the potential risks and side effects associated with its use, particularly when it comes to its impact on the vagus nerve.
Common Side Effects and Risks
The most commonly reported side effects of gabapentin include drowsiness, dizziness, and fatigue. These effects are usually mild and tend to resolve as the body adjusts to the medication. However, it is important to note that some individuals may experience these side effects more intensely than others.
In addition to drowsiness and fatigue, individuals taking gabapentin may also experience gastrointestinal disturbances, such as nausea or constipation. These side effects can be bothersome but are generally manageable with lifestyle modifications and over-the-counter remedies.
While rare, it is important to be aware that gabapentin can lead to more severe side effects, including increased suicidal thoughts or behaviors. This risk is particularly relevant for individuals with a history of mental health conditions or those taking other medications that may interact with gabapentin. It is crucial to inform healthcare providers promptly if any concerning side effects occur.
Managing Potential Complications
To minimize risks and manage the potential complications associated with gabapentin use on the vagus nerve, healthcare professionals adhere to careful prescribing practices. Starting with lower doses and gradually increasing dosage based on individual responses can help mitigate side effects.
Regular monitoring and open communication with healthcare providers are essential to ensure the medication’s effectiveness and safety. Healthcare professionals will closely monitor patients for any signs of adverse effects and adjust the dosage or consider alternative treatment options if necessary.
It is also important for individuals taking gabapentin to be proactive in managing their health. This includes following a healthy lifestyle, such as getting regular exercise, eating a balanced diet, and practicing stress-reducing techniques. These lifestyle factors can contribute to overall well-being and potentially minimize the occurrence of side effects.
In conclusion, while gabapentin can be an effective medication for various conditions, it is important to be aware of the potential risks and side effects associated with its use on the vagus nerve. By working closely with healthcare providers and being proactive in managing one’s health, individuals can maximize the benefits of gabapentin while minimizing any potential complications.
Future Research Directions
As we conclude our comprehensive analysis, it is worth considering the future research directions that may shed further light on the impact of gabapentin on the vagus nerve.
One potential avenue for future research is to investigate the specific molecular mechanisms through which gabapentin interacts with the vagus nerve. Understanding these mechanisms could provide valuable insights into the drug’s effectiveness and help identify potential targets for therapeutic intervention.
Another area of interest for future studies is the optimal dosage and treatment duration of gabapentin for vagus nerve-related conditions. While current research has provided some guidance, further investigation is needed to determine the most effective and safe dosing regimens for different patient populations.
Furthermore, exploring the potential benefits of gabapentin in specific populations with vagal involvement could be a fruitful area of research. For example, investigating the drug’s efficacy in treating neurological and neuropsychiatric disorders that are known to involve vagal dysfunction, such as epilepsy or depression, could provide valuable insights into its therapeutic potential.
Unanswered Questions and Potential Studies
Despite the growing body of research, several unanswered questions remain regarding the specific mechanisms and potential long-term effects of gabapentin on the vagus nerve. Further studies are needed to investigate optimal dosages, treatment durations, and the potential benefits of gabapentin in specific populations.
One important question that remains unanswered is whether there are any potential side effects or adverse reactions associated with long-term gabapentin use for vagus nerve-related conditions. Understanding the safety profile of the drug is crucial for its widespread use and acceptance in clinical practice.
Additionally, more research is needed to explore the potential interactions between gabapentin and other medications commonly used in conjunction with vagus nerve treatment. Understanding these interactions could help optimize treatment strategies and minimize the risk of adverse drug reactions.
The Future of Gabapentin and Vagus Nerve Treatment
With the increasing recognition of the vagus nerve’s role in human health and disease, as well as the expanding knowledge surrounding the potential impact of gabapentin, there is great potential for future developments in this field.
One exciting prospect is the development of novel gabapentin formulations or delivery methods that could enhance its efficacy and improve patient compliance. For example, exploring the use of extended-release formulations or alternative routes of administration, such as transdermal patches or inhalation, could offer new treatment options for patients with vagus nerve-related conditions.
Furthermore, the future of gabapentin and vagus nerve treatment may involve the development of personalized medicine approaches. By identifying biomarkers or genetic factors that can predict an individual’s response to gabapentin, clinicians could tailor treatment strategies to maximize therapeutic benefits and minimize potential side effects.
However, it is important to approach these possibilities with cautious optimism, as ongoing research will determine the true therapeutic potential of gabapentin in vagus nerve treatment.
In conclusion, gabapentin’s impact on the vagus nerve holds significant promise for expanding its therapeutic applications beyond its primary indications. While preliminary evidence suggests potential benefits, further research is needed to fully understand the mechanisms and establish the efficacy and safety of gabapentin in targeting vagal dysfunction.
As with any medical treatment, it is crucial to consult with a healthcare professional to determine the appropriate course of action for individual circumstances. By staying informed and engaged with ongoing research, we can continue to unravel the complex relationship between gabapentin and the vagus nerve in pursuit of improved patient care and well-being.
If you’re fascinated by the intricate relationship between gabapentin and the vagus nerve, and wish to delve deeper into understanding this remarkable aspect of human physiology, “My Vagus Nerve & Me Book” is the perfect next step. This comprehensive guide will take you on a journey through the complexities of the vagus nerve, from its role in regulating essential bodily functions to innovative ways to stimulate it for improved health. Discover the secrets of one of the most sophisticated systems in your body and learn practical insights into enhancing your well-being. Ready to unlock the mysteries of your vagus nerve? Get My Vagus Nerve & Me eBook today and embark on a transformative exploration of your inner workings.