The COVID-19 pandemic has brought about numerous challenges and has impacted various aspects of our lives. One area that has gained attention in recent research is the potential impact of COVID-19 on the vagus nerve. In this comprehensive analysis, we will delve into the understanding of the vagus nerve, explore its connection to the immune system, and examine how COVID-19 affects this crucial neural pathway.
Understanding the Vagus Nerve
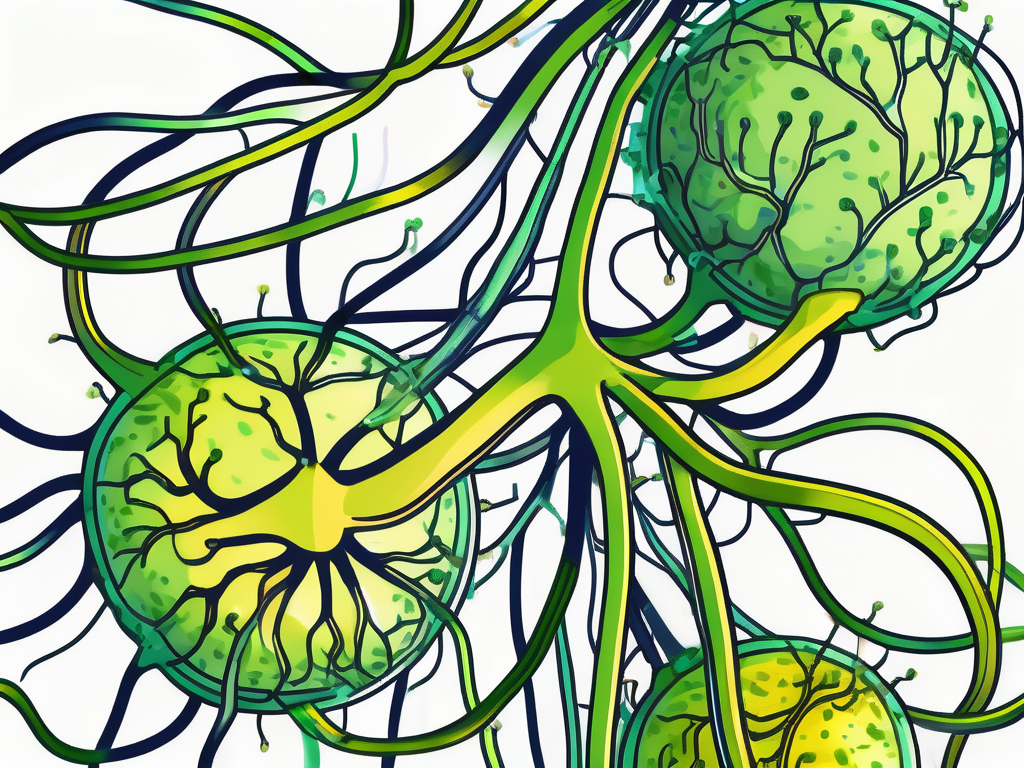
The vagus nerve, also known as the 10th cranial nerve, is a key player in our nervous system. It is the longest cranial nerve and plays a vital role in regulating several bodily functions. Responsible for the parasympathetic nervous system, the vagus nerve controls autonomous processes such as heart rate, digestion, and respiratory function.
The vagus nerve originates in the medulla oblongata of the brain and extends through the neck and chest to the abdomen. Dividing into multiple branches, it innervates various organs, including the heart, lungs, and digestive system.
One of the primary functions of the vagus nerve is to promote rest and relaxation by activating the parasympathetic nervous system. It helps to slow down heart rate, stimulate digestion, and enhance immune responses.
But let’s delve deeper into the fascinating anatomy and function of the vagus nerve.
Anatomy and Function of the Vagus Nerve
The vagus nerve, originating in the medulla oblongata, is a complex network of fibers that extends through the neck and chest, reaching all the way down to the abdomen. It is composed of both sensory and motor fibers, allowing it to transmit information from the body to the brain and vice versa.
As the vagus nerve travels through the body, it branches out into various pathways, each responsible for innervating specific organs. For instance, one branch connects to the heart, regulating its rhythm and ensuring its proper functioning. Another branch reaches the lungs, controlling respiratory processes such as breathing rate and depth.
Moreover, the vagus nerve plays a crucial role in the digestive system. It sends signals to the stomach, intestines, and other digestive organs, stimulating the release of digestive enzymes and promoting efficient nutrient absorption.
It is truly remarkable how this single nerve can have such a widespread influence on our bodily functions.
The Vagus Nerve and the Immune System
Research has suggested a fascinating connection between the vagus nerve and the immune system. Through its extensive reach, the vagus nerve can interact with immune cells and modulate their activity. This interaction is known as the “vagus nerve-immune axis.”
When the vagus nerve is activated, it can reduce the release of pro-inflammatory cytokines, which are associated with inflammation and autoimmune diseases. This anti-inflammatory effect helps to maintain a balanced immune response, preventing excessive inflammation that can harm the body.
Furthermore, the vagus nerve promotes the production of anti-inflammatory substances, such as acetylcholine, which have a protective effect on the body. These substances help to regulate the immune system, ensuring it functions optimally and efficiently.
The vagus nerve’s influence on the immune system highlights its importance in maintaining overall health and well-being.
In conclusion, the vagus nerve is a remarkable component of our nervous system. Its extensive reach and intricate connections allow it to regulate various bodily functions, promoting rest, relaxation, and a balanced immune response. Understanding the vagus nerve’s anatomy and function provides valuable insights into the complexity of our bodies and the interconnectedness of our physiological processes.
COVID-19: A Brief Overview
As we examine the influence of COVID-19 on the vagus nerve, it is essential to have a brief overview of this novel coronavirus.
The COVID-19 pandemic has had a profound impact on the world, affecting millions of lives and disrupting societies on a global scale. This highly contagious virus, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has presented numerous challenges to healthcare systems and scientists worldwide. To better understand the implications of COVID-19 on the vagus nerve, we must delve into the nature of the virus and its wide-ranging effects on the human body.
The Nature of the Virus
COVID-19 primarily affects the respiratory system, with symptoms ranging from mild to severe respiratory distress. The virus spreads through respiratory droplets when an infected person coughs, sneezes, or talks, making it highly contagious. However, research has shown that the virus can also affect other organ systems, including the cardiovascular and nervous systems.
Scientists have discovered that SARS-CoV-2 enters human cells by binding to a specific receptor called angiotensin-converting enzyme 2 (ACE2). This receptor is found in various tissues throughout the body, including the lungs, heart, blood vessels, and even the brain. The ability of the virus to invade multiple organ systems contributes to its diverse range of symptoms and complications.
Symptoms and Complications of COVID-19
The most commonly observed symptoms of COVID-19 include fever, cough, shortness of breath, and fatigue. However, the virus’s impact can extend beyond these typical respiratory symptoms.
As the virus spreads throughout the body, it can lead to complications such as blood clots, kidney damage, and neurological symptoms. Blood clots, also known as thrombosis, can form in blood vessels, obstructing the flow of blood and potentially causing severe complications such as strokes or heart attacks. Kidney damage can occur due to the virus’s direct attack on kidney cells or as a result of the body’s immune response to the infection. Neurological symptoms, including loss of taste and smell, headaches, dizziness, and even strokes, have been reported in COVID-19 patients.
Furthermore, recent studies have highlighted the potential impact of COVID-19 on the vagus nerve, a crucial component of the parasympathetic nervous system. The vagus nerve plays a vital role in regulating various bodily functions, including heart rate, digestion, and inflammation. Understanding the comprehensive impact of COVID-19 is essential to explore its potential effects on the vagus nerve and the subsequent implications for overall health and well-being.
The Intersection of COVID-19 and the Vagus Nerve
Now let’s delve into the intersection of COVID-19 and the vagus nerve, examining the potential pathways through which the virus affects this vital neural pathway.
The vagus nerve, also known as the tenth cranial nerve, is a crucial component of the parasympathetic nervous system. It is the longest cranial nerve in the body, extending from the brainstem to various organs, including the heart, lungs, and digestive system. The vagus nerve plays a vital role in regulating bodily functions such as heart rate, digestion, and immune response.
The Vagus Nerve as a Pathway for COVID-19
Research suggests that SARS-CoV-2 has the potential to directly infect neurons, including those that make up the vagus nerve. This raises the possibility of direct viral infiltration into the vagus nerve, impacting its function and communication with various organs.
Furthermore, the vagus nerve is not only a potential target for viral invasion but also a conduit for the transmission of signals between the brain and the immune system. By infiltrating the vagus nerve, the virus may disrupt this crucial line of communication, leading to dysregulation of immune responses and potentially exacerbating the severity of COVID-19 symptoms.
Moreover, the virus may indirectly affect the vagus nerve through the release of pro-inflammatory cytokines and other immune responses triggered by COVID-19. Inflammation in the vicinity of the vagus nerve can disrupt its normal functionality and subsequent communication with targeted organs.
The Impact of COVID-19 on Vagus Nerve Function
The vagus nerve’s potential involvement in COVID-19 raises intriguing questions about its impact on vagal tone and regulation. Vagal tone refers to the vagus nerve’s efficiency in modulating bodily processes, and its disruption can have significant implications for overall well-being.
Preliminary evidence suggests that COVID-19 may alter vagal tone and contribute to autonomic dysregulation. This dysregulation can manifest in various symptoms such as rapid heart rate, gastrointestinal disturbances, and sleep disturbances.
Furthermore, the vagus nerve is known to play a crucial role in the regulation of inflammation. By modulating the release of inflammatory molecules, the vagus nerve helps maintain a balanced immune response. However, in the context of COVID-19, the virus’s impact on the vagus nerve may disrupt this delicate balance, leading to excessive inflammation and potentially contributing to the development of severe complications.
Additionally, the vagus nerve is intricately connected to the brain’s emotional and stress response centers. It is involved in regulating mood, anxiety, and stress levels. Given the psychological impact of the COVID-19 pandemic, it is plausible that the virus’s effects on the vagus nerve may contribute to the development or exacerbation of mental health conditions.
In conclusion, the intersection of COVID-19 and the vagus nerve presents a complex and fascinating area of research. Understanding the mechanisms through which the virus affects this vital neural pathway can provide valuable insights into the pathophysiology of the disease and potentially guide the development of targeted therapeutic interventions.
Potential Long-Term Effects of COVID-19 on the Vagus Nerve
As we continue to unravel the mysteries surrounding COVID-19, it is crucial to consider the potential long-term effects on the vagus nerve.
The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body. It plays a vital role in regulating various bodily functions, including heart rate, digestion, and immune response. Given its extensive reach and influence, any disruption or damage to the vagus nerve can have profound consequences.
Chronic Symptoms and the Vagus Nerve
Some individuals recovering from COVID-19 experience persistent symptoms, often referred to as “long COVID” or post-acute sequelae of SARS-CoV-2 infection. These chronic symptoms can extend beyond respiratory issues and may involve the vagus nerve.
While the exact mechanisms linking COVID-19 to vagus nerve dysfunction are not yet fully understood, emerging evidence suggests a potential connection. The virus can directly invade the nervous system, causing inflammation and damage to nerve cells, including those of the vagus nerve.
Furthermore, the immune response triggered by COVID-19 can lead to a state of chronic inflammation, which can affect the vagus nerve’s function. Inflammation can alter the nerve’s signaling pathways, disrupting its ability to regulate various bodily processes.
Although research is ongoing, it is important to note that the vagus nerve’s involvement in chronic symptoms is likely complex and requires further investigation. Scientists are diligently working to unravel the intricate relationship between COVID-19 and the vagus nerve to develop effective treatment strategies.
The Role of the Vagus Nerve in Post-Acute Sequelae of SARS-CoV-2
Post-acute sequelae of SARS-CoV-2, also known as “long COVID,” is a multifaceted condition that can affect various organs and systems in the body. The vagus nerve’s potential involvement in long COVID raises intriguing possibilities.
It is hypothesized that the dysregulation of vagal tone may contribute to the symptoms experienced by individuals with long COVID, such as brain fog, fatigue, and autonomic dysfunction. The vagus nerve’s intricate network of connections allows it to communicate with different regions of the brain, influencing cognitive function, mood, and overall well-being.
Moreover, the vagus nerve plays a crucial role in the immune response. It helps regulate the body’s inflammatory processes, ensuring a balanced immune reaction. Dysregulation of vagal tone in long COVID patients could lead to an overactive immune response, perpetuating chronic inflammation and contributing to ongoing symptoms.
Understanding the intricate interplay between COVID-19, the vagus nerve, and long COVID is a complex task. Researchers are exploring various avenues, including neuroimaging studies, to gain insights into how the virus affects the vagus nerve and how this impacts long-term health outcomes.
By unraveling the mysteries surrounding the potential long-term effects of COVID-19 on the vagus nerve, scientists hope to develop targeted interventions that can alleviate symptoms and improve the quality of life for those affected by long COVID.
Therapeutic Approaches and the Vagus Nerve
While we await further research on the specific impact of COVID-19 on the vagus nerve, exploring potential therapeutic approaches holds promise for mitigating its effects.
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions, including heart rate, digestion, and immune response. It is a complex network of fibers that connects the brain to different organs throughout the body.
One potential therapeutic approach that has shown promise in various medical conditions is vagus nerve stimulation (VNS). This well-established therapy involves the application of low-level electrical pulses to stimulate the vagus nerve, promoting its normal functionality.
VNS has been used as a treatment option for conditions such as epilepsy and treatment-resistant depression. By stimulating the vagus nerve, VNS aims to restore balance and improve overall well-being.
Vagus Nerve Stimulation as a Potential Treatment
Although VNS has shown promise in various conditions, its specific role in COVID-19-related vagus nerve dysregulation requires further investigation. The novel coronavirus, SARS-CoV-2, has been found to affect multiple organ systems, including the respiratory system, cardiovascular system, and nervous system.
Research suggests that COVID-19 may have an impact on the vagus nerve, leading to dysregulation and potential health complications. However, the exact mechanisms through which the virus affects vagal function are still not fully understood.
Consultation with a healthcare professional is crucial before considering any therapeutic interventions. They can provide personalized advice based on your specific medical history and symptoms.
Future Research Directions in Vagus Nerve and COVID-19 Interaction
As the scientific community continues to explore the complex relationship between COVID-19 and the vagus nerve, future research holds the potential to expand our understanding of this interaction.
Researchers are actively investigating the mechanisms through which the virus affects vagal function. By unraveling these mechanisms, scientists hope to develop targeted therapies that can mitigate the impact of COVID-19 on the vagus nerve.
Additionally, exploring potential preventive measures is another important area of research. Understanding how to protect the vagus nerve from the detrimental effects of the virus could help reduce the severity of COVID-19-related complications.
It is important to acknowledge that this comprehensive analysis represents the current state of scientific knowledge and ongoing research. The field of COVID-19 research is rapidly evolving, and new findings may emerge that further enhance our understanding of the vagus nerve’s role in this disease.
If you have concerns or experience symptoms related to COVID-19 or the vagus nerve, it is advisable to consult with a healthcare professional for accurate diagnosis and appropriate guidance. They can provide the most up-to-date information and recommend the best course of action for your specific situation.
By staying informed and supporting ongoing research, we can collectively strive to understand the impact of COVID-19 on the vagus nerve and develop strategies to promote health and well-being.
If you’re fascinated by the critical role the vagus nerve plays in your health and are eager to delve deeper into its functions and the ways you can nurture it, “My Vagus Nerve & Me Book” is the perfect resource. Discover the secrets of this extraordinary system that orchestrates your heart rate, digestion, immune response, and so much more. Learn practical tips on how to stimulate your vagus nerve, both naturally and artificially, to enhance your overall well-being. Embrace the opportunity to empower yourself with knowledge about this vital nerve that influences everything from liver detoxification to blood pressure regulation. Get My Vagus Nerve & Me eBook today and embark on a journey to better health!