The connection between the vagus nerve and the pelvic floor is an emerging area of research that is shedding light on the intricate links between the nervous system and the musculoskeletal system. Understanding this connection is crucial for diagnosing and treating various disorders that affect both the vagus nerve and the pelvic floor. In this article, we will delve into the role of the vagus nerve and the anatomy of the pelvic floor, examine the neurological connection between the two, explore the implications for health and wellness, discuss therapeutic approaches, and highlight future research directions.
Understanding the Vagus Nerve
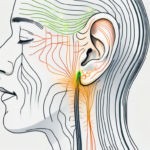
The vagus nerve, also known as the tenth cranial nerve, is a critically important component of the parasympathetic nervous system. It originates in the brainstem and travels throughout the body, innervating various organs and tissues, including the heart, lungs, stomach, and intestines. The vagus nerve plays a vital role in regulating many bodily functions, such as heart rate, digestion, and respiratory rhythm. It is often referred to as the “wandering nerve” due to its extensive reach throughout the body.
The vagus nerve is not only responsible for the regulation of basic bodily functions but also has a profound impact on overall health and well-being. Research has shown that the vagus nerve is involved in the modulation of inflammation and immune response. When activated, it can help reduce the production of pro-inflammatory cytokines, molecules that play a significant role in the development of chronic diseases such as cardiovascular disease, diabetes, and autoimmune disorders.
In addition to its role in physical health, the vagus nerve also influences mood and emotional well-being. It has been found that stimulating the vagus nerve can have antidepressant effects, leading to improvements in symptoms of depression and anxiety. This connection between the vagus nerve and mental health highlights the intricate relationship between the brain and the body, demonstrating how the health of one can impact the other.
The Role and Function of the Vagus Nerve
One of the primary functions of the vagus nerve is to promote a state of relaxation and rest by activating the parasympathetic response. It helps to reduce heart rate, lower blood pressure, and enhance digestion. The vagus nerve achieves this by releasing acetylcholine, a neurotransmitter that acts as a messenger between nerve cells. Acetylcholine binds to receptors on target cells, triggering a cascade of physiological responses that promote relaxation and restoration.
Furthermore, the vagus nerve is involved in the regulation of gastrointestinal motility and secretion. It stimulates the release of digestive enzymes and increases blood flow to the digestive organs, facilitating the breakdown and absorption of nutrients. Dysfunction of the vagus nerve can lead to digestive problems such as gastroparesis, a condition characterized by delayed stomach emptying.
The Vagus Nerve and the Autonomic Nervous System
The vagus nerve is intimately connected with the autonomic nervous system, which controls involuntary bodily functions. It works in conjunction with the sympathetic nervous system, which is responsible for the body’s response to stress and danger. The vagus nerve acts as a counterbalance, helping to restore equilibrium and promote relaxation after periods of heightened activity.
During times of stress or danger, the sympathetic nervous system triggers the “fight or flight” response, preparing the body for action. This response involves an increase in heart rate, blood pressure, and respiration, as well as a redirection of blood flow to the muscles. Once the threat has passed, the vagus nerve steps in to activate the parasympathetic response, which promotes rest and recovery. It helps to lower heart rate, blood pressure, and respiration, allowing the body to return to a state of balance.
This delicate balance between the sympathetic and parasympathetic responses is critical for maintaining overall health and well-being. Dysfunction of the vagus nerve can disrupt this balance, leading to a range of health issues. For example, an overactive vagus nerve can result in excessive relaxation and a decrease in heart rate, causing conditions such as bradycardia. On the other hand, an underactive vagus nerve can lead to increased sympathetic activity, contributing to conditions such as hypertension and anxiety disorders.
The Anatomy of the Pelvic Floor
The pelvic floor refers to a group of muscles and connective tissues that form a supportive hammock-like structure in the pelvic region. It plays a significant role in supporting the organs of the pelvis, including the bladder, uterus, and rectum. The pelvic floor also has a crucial function in maintaining urinary and bowel continence, as well as facilitating sexual function. It is important to note that both men and women have a pelvic floor, although it serves slightly different purposes for each gender.
The pelvic floor is a complex network of muscles that work together to provide support and stability to the pelvic organs. These muscles include the pubococcygeus muscle, the iliococcygeus muscle, and the coccygeus muscle. The pubococcygeus muscle, also known as the PC muscle, is responsible for controlling the flow of urine and contracting during orgasm. The iliococcygeus muscle helps to maintain continence and supports the pelvic organs. The coccygeus muscle provides additional support to the pelvic floor.
The Importance of a Healthy Pelvic Floor
A healthy pelvic floor is essential for overall well-being and quality of life. Weakness or dysfunction in the pelvic floor muscles can lead to urinary incontinence, fecal incontinence, and pelvic organ prolapse. Conditions such as pregnancy, childbirth, aging, obesity, and chronic constipation can contribute to pelvic floor disorders. It is important to maintain the strength and integrity of the pelvic floor to prevent and manage these issues.
Pregnancy and childbirth can put significant strain on the pelvic floor muscles. The weight of the growing fetus and the stretching of the pelvic muscles during delivery can weaken the pelvic floor. This can result in urinary incontinence, where the individual experiences involuntary leakage of urine. It can also lead to fecal incontinence, where the person is unable to control bowel movements. These conditions can be distressing and affect a person’s self-esteem and confidence.
Aging is another factor that can contribute to pelvic floor disorders. As we age, the muscles and tissues in the pelvic floor naturally weaken. This can lead to urinary incontinence and pelvic organ prolapse, where the bladder, uterus, or rectum descend into the vaginal canal. Pelvic organ prolapse can cause discomfort, pain, and a feeling of pressure in the pelvic region. It can also interfere with sexual function and quality of life.
Common Disorders of the Pelvic Floor
There are several common disorders that can affect the pelvic floor. Urinary incontinence, which is the involuntary leakage of urine, affects millions of people worldwide. Stress urinary incontinence occurs when there is pressure on the bladder, such as during coughing, sneezing, or physical activity. Urge incontinence, on the other hand, is characterized by a sudden and intense urge to urinate, followed by involuntary leakage.
Fecal incontinence, the inability to control bowel movements, is another prevalent condition. It can be caused by a variety of factors, including muscle or nerve damage, chronic constipation, or certain medical conditions. Fecal incontinence can have a significant impact on a person’s daily life, causing embarrassment, social isolation, and a decreased quality of life.
Pelvic organ prolapse, where the pelvic organs descend into the vaginal canal, is also a common disorder. This can occur when the muscles and tissues that support the pelvic organs become weakened or damaged. Pelvic organ prolapse can cause a variety of symptoms, including a feeling of pressure or fullness in the pelvic area, a bulge or protrusion from the vagina, and discomfort during sexual intercourse.
These conditions can significantly impact a person’s quality of life and should be addressed with medical professionals specializing in pelvic health. Treatment options for pelvic floor disorders may include pelvic floor exercises, lifestyle modifications, medications, or surgical interventions. It is important to seek help and support if you are experiencing any symptoms related to pelvic floor dysfunction.
The Neurological Connection
The connection between the vagus nerve and the pelvic floor lies in the intricate network of nerves that innervate the pelvic region. When the vagus nerve is activated, it can influence the muscles of the pelvic floor through these nerve connections. Research suggests that the vagus nerve may play a role in regulating the tone and function of the pelvic floor muscles, contributing to urinary and bowel control, as well as sexual function.
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It originates in the brainstem and extends down to various organs in the body, including the heart, lungs, and gastrointestinal tract. Along its pathway, the vagus nerve branches out and forms connections with different structures, including the pelvic floor.
Within the pelvic region, the pelvic floor muscles are responsible for supporting the pelvic organs, maintaining continence, and facilitating sexual function. These muscles work in coordination with other structures, such as the bladder, urethra, rectum, and reproductive organs. The vagus nerve’s influence on the pelvic floor muscles is crucial for their proper functioning.
How the Vagus Nerve Influences the Pelvic Floor
Studies have shown that stimulation of the vagus nerve can have effects on the pelvic floor, including increased sphincter tone and improved muscle strength. By activating the parasympathetic response, the vagus nerve can promote relaxation and enhance blood flow to the pelvic region, facilitating optimal muscle function. This connection offers potential therapeutic avenues for individuals with pelvic floor disorders.
Furthermore, the vagus nerve’s influence on the pelvic floor extends beyond muscle tone and strength. It also plays a role in modulating pain perception and inflammation in the pelvic region. Activation of the vagus nerve has been found to have analgesic effects, reducing pain sensations and inflammation in conditions such as chronic pelvic pain syndrome and interstitial cystitis.
Understanding the intricate relationship between the vagus nerve and the pelvic floor is essential for developing targeted therapies and interventions to improve pelvic floor function and alleviate symptoms associated with pelvic floor disorders.
The Impact of Stress on the Vagus Nerve and Pelvic Floor
It is well-known that stress can have a profound impact on both the vagus nerve and the pelvic floor. Heightened levels of stress can disrupt the balance between the sympathetic and parasympathetic responses, leading to increased tension in the pelvic floor and compromised muscle function. Chronic stress can contribute to the development or exacerbation of pelvic floor disorders. Therefore, stress management techniques, such as mindfulness, relaxation exercises, and therapy, can be beneficial in maintaining pelvic health.
When a person experiences stress, the sympathetic nervous system, also known as the “fight-or-flight” response, becomes activated. This response prepares the body for immediate action by increasing heart rate, constricting blood vessels, and diverting blood flow away from non-essential organs, including the pelvic region. As a result, the pelvic floor muscles may become tense and less responsive, leading to symptoms such as urinary urgency, frequency, or incontinence.
On the other hand, the parasympathetic nervous system, which is regulated by the vagus nerve, promotes relaxation and restoration. It counteracts the effects of stress by slowing heart rate, dilating blood vessels, and increasing blood flow to the pelvic region. By engaging in stress management techniques, individuals can activate the parasympathetic response and promote optimal pelvic floor function.
Overall, the relationship between the vagus nerve, stress, and the pelvic floor is complex and multifaceted. By understanding and addressing this connection, healthcare professionals can develop comprehensive treatment plans that target both the physical and emotional aspects of pelvic floor disorders.
The Implications for Health and Wellness
The connection between the vagus nerve and the pelvic floor has significant implications for health and wellness. By understanding this link, healthcare professionals can develop targeted interventions that aim to regulate both the vagus nerve and the pelvic floor. This integrative approach can have positive effects on various aspects of health, including digestive health and sexual function.
The Vagus Nerve, Pelvic Floor, and Digestive Health
The vagus nerve plays a crucial role in regulating digestion and nutrient absorption. It is responsible for sending signals to the digestive organs, promoting relaxation, and enhancing blood flow to optimize digestive function. Dysfunction in the pelvic floor can impact digestive health, leading to symptoms such as constipation or delayed transit time.
When the pelvic floor muscles are weak or tight, they can disrupt the normal movement of food through the digestive system. This can result in difficulties with bowel movements, causing discomfort and irregularity. By addressing the dysfunction in both the vagus nerve and the pelvic floor, healthcare professionals can help individuals manage their digestive issues more effectively.
Consulting with healthcare professionals experienced in both neurology and pelvic health can provide guidance on managing digestive issues related to the vagus nerve and pelvic floor. They can recommend specific exercises and techniques to strengthen and relax the pelvic floor muscles, as well as provide dietary recommendations to support optimal digestive function.
The Vagus Nerve, Pelvic Floor, and Sexual Health
Sexual function is influenced by a variety of factors, including the health of the pelvic floor and the functioning of the vagus nerve. Dysfunction in either of these areas can contribute to sexual difficulties, such as decreased libido, pain during intercourse, or difficulty achieving orgasm.
The pelvic floor muscles play a crucial role in sexual function by supporting the organs involved in sexual activity and controlling the flow of blood to the genital area. When these muscles are weak or tight, they can impair sexual function and lead to discomfort or pain. Additionally, the vagus nerve is responsible for regulating arousal and sexual response, making it essential for a healthy and satisfying sexual experience.
Addressing sexual health issues requires a comprehensive approach that considers both the muscular and neurological aspects. Collaborating with healthcare professionals specializing in both neurology and pelvic health can help individuals navigate these challenges. They can provide guidance on exercises to strengthen the pelvic floor muscles, as well as techniques to regulate the vagus nerve and enhance sexual function.
Furthermore, healthcare professionals can also explore other factors that may be contributing to sexual difficulties, such as hormonal imbalances or psychological factors. By taking a holistic approach to sexual health, individuals can work towards improving their overall well-being and quality of life.
Therapeutic Approaches and Interventions
Several therapeutic approaches and interventions can be utilized to address the connection between the vagus nerve and the pelvic floor. Vagus nerve stimulation techniques, such as deep breathing exercises, meditation, and vagal maneuvers, can help activate the parasympathetic response and promote relaxation throughout the body. Pelvic floor exercises, such as kegels, can be beneficial in strengthening the pelvic floor muscles and improving muscle tone. These interventions should be approached under the guidance of healthcare professionals experienced in neurology and pelvic health.
Vagus Nerve Stimulation Techniques
Vagus nerve stimulation techniques involve various methods of activating the vagus nerve to promote relaxation and improve overall well-being. Deep breathing exercises, where the focus is on slow, diaphragmatic breathing, can have a calming effect on the nervous system. By taking deep breaths, you allow your body to take in more oxygen, which can help reduce stress and anxiety. This type of breathing can also stimulate the vagus nerve, leading to a relaxation response throughout your body.
In addition to deep breathing exercises, meditation and mindfulness practices can help regulate stress responses and enhance vagal tone. When you engage in meditation, you focus your attention and eliminate the stream of thoughts that may be causing stress or anxiety. This practice can activate the parasympathetic nervous system, which is responsible for promoting relaxation and reducing stress. By incorporating meditation into your daily routine, you can strengthen the connection between the vagus nerve and the pelvic floor, leading to improved overall well-being.
Furthermore, certain physical maneuvers, such as cold-water face immersion or gag reflex stimulation, can stimulate the vagus nerve. Cold-water face immersion involves submerging your face in cold water for a short period. This sudden change in temperature can activate the vagus nerve, triggering a relaxation response. Gag reflex stimulation, on the other hand, involves gently stimulating the back of your throat to elicit a gag reflex. This stimulation can also activate the vagus nerve, promoting relaxation and reducing tension in the pelvic floor.
Pelvic Floor Exercises and Their Benefits
Pelvic floor exercises, commonly known as kegels, aim to strengthen the muscles of the pelvic floor. These exercises involve contracting and relaxing the muscles that support the bladder, uterus, and rectum. Regular practice of kegels can improve muscle tone, enhance pelvic organ support, and alleviate symptoms associated with pelvic floor disorders.
When performing kegels, it is important to learn proper technique and seek guidance from healthcare professionals specializing in pelvic health. They can provide personalized instructions and ensure that you are targeting the correct muscles. Additionally, they can help you establish an appropriate exercise routine and monitor your progress over time.
By incorporating kegels into your daily routine, you can strengthen the pelvic floor muscles, which play a crucial role in maintaining continence, supporting pelvic organs, and enhancing sexual function. These exercises can be particularly beneficial for individuals experiencing urinary incontinence, pelvic organ prolapse, or sexual dysfunction.
In conclusion, therapeutic approaches and interventions that target the connection between the vagus nerve and the pelvic floor can have significant benefits for overall well-being. Vagus nerve stimulation techniques, such as deep breathing exercises, meditation, and physical maneuvers, can activate the parasympathetic response and promote relaxation. Pelvic floor exercises, such as kegels, can strengthen the pelvic floor muscles and improve muscle tone. It is important to seek guidance from healthcare professionals experienced in neurology and pelvic health to ensure the effectiveness and safety of these interventions.
Future Research Directions
The connection between the vagus nerve and the pelvic floor is still an area of ongoing research. There are many unanswered questions and potential studies that could shed further light on this link and its implications for health and wellness. Researchers are exploring the potential benefits of vagus nerve stimulation techniques, such as non-invasive methods and the use of neuromodulation devices. Furthermore, more studies are needed to elucidate the specific effects of vagal interventions on the pelvic floor and identify optimal therapeutic approaches.
Unanswered Questions and Potential Studies
Despite the progress made in understanding the connection between the vagus nerve and the pelvic floor, there are still many unanswered questions. For example, the specific mechanisms through which the vagus nerve influences pelvic floor function are not yet fully understood. Further research is needed to explore the complex interplay between the nervous system and the musculoskeletal system in the pelvic region. Additionally, randomized controlled trials are necessary to determine the efficacy and safety of interventions targeting the vagus nerve and the pelvic floor.
The Future of Neurological and Pelvic Health
The expanding knowledge of the connection between the vagus nerve and the pelvic floor holds great promise for the future of neurological and pelvic health. By unraveling the intricate links between these systems, healthcare professionals can develop more targeted and effective interventions for individuals with pelvic floor disorders. It is crucial to continue supporting and investing in research that explores this connection to improve the lives of those affected by neurological and pelvic health conditions.
In conclusion, the connection between the vagus nerve and the pelvic floor is a complex and fascinating area of study. Understanding this link can unlock new approaches for diagnosing and treating various disorders that affect both the vagus nerve and the pelvic floor. By exploring the role of the vagus nerve, the anatomy of the pelvic floor, the neurological connection, the implications for health and wellness, therapeutic approaches, and future research directions, we can broaden our understanding and pave the way for advancements in neurological and pelvic health. If you are experiencing symptoms related to the vagus nerve or the pelvic floor, it is essential to consult with healthcare professionals who specialize in these areas to receive appropriate diagnosis and treatment.
If you’re fascinated by the profound impact the vagus nerve has on your health and are eager to delve deeper into its mysteries, “My Vagus Nerve & Me Book” is the perfect resource for you. Discover the secrets of one of the most sophisticated systems in the human body and learn how to harness its power for your well-being. From understanding its complex functions to exploring ways to stimulate it for better health, this book is an essential guide for anyone looking to improve their immune system, digestion, heart rate, mental health, and more. Don’t miss out on the opportunity to unlock the full potential of your vagus nerve. Get My Vagus Nerve & Me eBook today and take the first step towards a healthier you.