The vagus nerve and hiatal hernia are two fascinating aspects of the human body that have a profound impact on our overall health. In this article, we will explore the intricate connection between these two entities and discuss their role and significance.
Understanding the Vagus Nerve
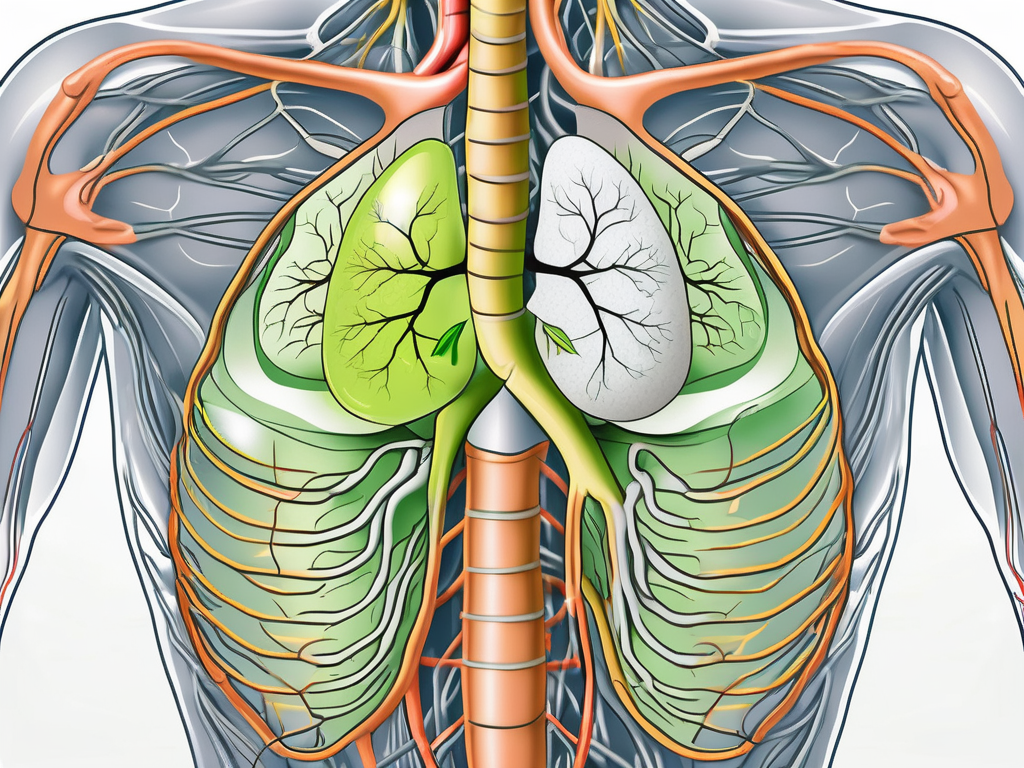
The vagus nerve, also known as the tenth cranial nerve, is one of the longest and most important nerves in our body. It originates in the brainstem and extends down to our abdomen, innervating various organs along the way. This vital nerve plays a crucial role in regulating many bodily functions, including digestion, heart rate, and lung function.
When it comes to digestion, the vagus nerve acts as a messenger between the brain and the gastrointestinal tract. It helps stimulate the release of digestive enzymes and promotes the movement of food through the digestive system. This intricate communication system ensures that our bodies efficiently break down and absorb nutrients from the food we consume.
Furthermore, the vagus nerve influences heart rate regulation. It sends signals to the heart, instructing it to slow down during periods of rest and relaxation. This mechanism helps conserve energy and maintain a healthy cardiovascular system. In addition to heart rate control, the vagus nerve also plays a role in regulating blood pressure by relaxing blood vessels, promoting optimal blood flow throughout the body.
The Role and Function of the Vagus Nerve
The vagus nerve serves as a vital communication channel between the brain and the rest of the body. It is responsible for transmitting signals that control the parasympathetic nervous system, which helps regulate the body’s resting state. This includes functions such as promoting digestion, reducing heart rate, and relaxing blood vessels. Additionally, the vagus nerve plays a role in maintaining a healthy balance within our body systems.
Moreover, the vagus nerve has a profound impact on our respiratory system. It sends signals to the muscles in our lungs, allowing us to breathe effortlessly and efficiently. This intricate connection ensures that oxygen is properly delivered to our cells and carbon dioxide is effectively eliminated from our bodies.
Furthermore, the vagus nerve influences various aspects of our gastrointestinal system. It helps regulate the production of stomach acid, ensuring optimal digestion and nutrient absorption. Additionally, it plays a role in controlling the contraction and relaxation of the muscles in the intestines, facilitating the movement of food through the digestive tract.
The Vagus Nerve’s Impact on the Body
Besides its primary functions, the vagus nerve also has a profound impact on various aspects of our health. Research suggests that it influences our mood, immune system response, and even plays a role in reducing inflammation. The vagus nerve is involved in the release of neurotransmitters such as serotonin and dopamine, which are crucial for regulating mood and emotions.
Furthermore, the vagus nerve has been implicated in the modulation of the immune system. It helps regulate the release of anti-inflammatory molecules, which play a crucial role in preventing excessive inflammation. This intricate connection between the vagus nerve and the immune system highlights the importance of maintaining a healthy vagal tone for overall well-being.
Excitingly, recent studies have also shown a potential link between the vagus nerve and certain chronic conditions, including hiatal hernia. Hiatal hernia occurs when a portion of the stomach protrudes into the chest cavity through the diaphragm. Research suggests that the vagus nerve may play a role in the regulation of the diaphragm’s function, potentially contributing to the development or progression of hiatal hernia.
In conclusion, the vagus nerve is a remarkable and intricate part of our nervous system. Its extensive reach and multifaceted functions make it a vital component in maintaining our overall health and well-being. Understanding the role and impact of the vagus nerve can provide valuable insights into various bodily processes and potentially open doors to new therapeutic approaches for a range of conditions.
What is a Hiatal Hernia?
A hiatal hernia occurs when a portion of the stomach pushes through the diaphragm and into the chest cavity. This protrusion can result in various uncomfortable symptoms, including acid reflux, chest pain, and difficulty swallowing. Hiatal hernias are relatively common, and they can occur in people of all ages, although they are more prevalent in older adults and those who are overweight.
When a hiatal hernia occurs, the natural barrier between the stomach and the chest cavity is disrupted. This can lead to the backflow of stomach acid into the esophagus, causing irritation and discomfort. The diaphragm, a muscle that separates the chest and abdominal cavities, normally helps to keep the stomach in place. However, certain factors can weaken the diaphragm and contribute to the development of a hiatal hernia.
Causes and Symptoms of Hiatal Hernia
The exact cause of hiatal hernias is not always known. However, factors such as age, obesity, and prolonged pressure on the abdominal area may contribute to their development. As we age, the muscles and tissues in our body naturally weaken, including the diaphragm. This weakening can make it easier for the stomach to push through the diaphragm and into the chest cavity.
Obesity is another risk factor for hiatal hernias. Excess weight puts added pressure on the abdominal area, which can increase the likelihood of a hernia forming. Additionally, certain lifestyle habits such as heavy lifting, persistent coughing, or straining during bowel movements can also contribute to the development of a hiatal hernia.
Symptoms of hiatal hernias can range from mild to severe, depending on the size and type of hernia. Common symptoms include heartburn, regurgitation, chest pain, and difficulty swallowing. Heartburn, also known as acid indigestion, is a burning sensation in the chest that occurs when stomach acid flows back into the esophagus. Regurgitation refers to the backflow of stomach contents into the mouth or throat. Chest pain caused by a hiatal hernia can mimic the symptoms of a heart attack, leading to anxiety and concern. Difficulty swallowing, known as dysphagia, can occur when the hernia compresses the esophagus, making it harder for food and liquids to pass through.
It is important to note that not all hiatal hernias cause symptoms. Some individuals may have a hiatal hernia without experiencing any discomfort or noticeable effects. However, if symptoms do occur and persist, it is essential to seek medical attention for proper diagnosis and treatment.
Treatment Options for Hiatal Hernia
The management of hiatal hernias typically involves a combination of lifestyle modifications and, in some cases, medical intervention. Lifestyle changes may include maintaining a healthy weight, avoiding foods that trigger symptoms, and elevating the head of the bed while sleeping. These measures can help reduce the occurrence and severity of symptoms associated with hiatal hernias.
In addition to lifestyle modifications, medications may be prescribed to alleviate symptoms. Antacids, which neutralize stomach acid, can provide temporary relief from heartburn and indigestion. Proton pump inhibitors (PPIs), on the other hand, reduce the production of stomach acid and can help heal the esophagus. These medications are typically taken on a regular basis to manage symptoms and prevent complications.
In severe cases where lifestyle modifications and medications do not provide sufficient relief, surgical intervention may be necessary to repair the hernia. The most common surgical procedure for hiatal hernias is called a Nissen fundoplication. During this procedure, the upper part of the stomach is wrapped around the lower esophagus to strengthen the natural barrier and prevent acid reflux. Surgery is usually considered when the hernia is large, causing severe symptoms, or if complications such as bleeding or obstruction occur.
It is important to consult with a healthcare professional to determine the most appropriate treatment plan for an individual with a hiatal hernia. The severity of symptoms, the size and type of hernia, and the overall health of the individual will all be taken into consideration when determining the best course of action.
The Vagus Nerve-Hiatal Hernia Connection
Recent research has shed light on the intriguing relationship between the vagus nerve and hiatal hernia. While the exact mechanisms are not fully understood, it is believed that alterations in vagal function and dysfunction may play a role in the development and progression of hiatal hernias.
How the Vagus Nerve Influences Hiatal Hernia
The vagus nerve, also known as the wandering nerve due to its extensive distribution throughout the body, controls the movement and contraction of various muscles. Among these are the muscles involved in maintaining the integrity of the diaphragm and supporting the esophagus.
When the vagus nerve functions optimally, it ensures that these muscles are strong and able to perform their roles effectively. However, dysfunction or impaired signaling of the vagus nerve can potentially weaken these muscles, leading to an increased risk of hiatal hernia development or exacerbation.
Studies have shown that conditions such as diabetes, obesity, and certain neurological disorders can negatively impact vagal function. These conditions may interfere with the nerve’s ability to transmit signals properly, compromising the muscles’ strength and leaving them susceptible to the forces that contribute to hiatal hernias.
The Effect of Hiatal Hernia on the Vagus Nerve
Conversely, hiatal hernias themselves can impact the vagus nerve. A hiatal hernia occurs when a portion of the stomach protrudes through the diaphragm into the chest cavity, disrupting the normal anatomical arrangement.
As the displaced stomach pushes against the diaphragm, it can put pressure on the vagus nerve, disturbing its normal function and signaling. This disruption can further contribute to digestive issues, including acid reflux and other gastrointestinal symptoms associated with hiatal hernias.
Moreover, the pressure exerted on the vagus nerve by the herniated stomach can lead to vagal nerve irritation. This irritation can result in a cascade of events, including increased acid production in the stomach, impaired motility of the esophagus, and dysfunction of the lower esophageal sphincter. These factors can exacerbate the symptoms of hiatal hernias and contribute to the development of complications such as gastroesophageal reflux disease (GERD).
It is worth noting that the relationship between the vagus nerve and hiatal hernia is complex and multifactorial. Other factors, such as genetic predisposition, lifestyle choices, and anatomical variations, also contribute to the development and progression of hiatal hernias.
Further research is needed to fully understand the intricate interplay between the vagus nerve and hiatal hernia. By unraveling the mechanisms underlying this connection, scientists and healthcare professionals can develop more targeted and effective treatments for individuals affected by hiatal hernias.
The Medical Implications of the Connection
Understanding the connection between the vagus nerve and hiatal hernia has important implications for medical treatment and management strategies. By targeting vagal function and considering its role in hiatal hernia development, healthcare professionals can tailor interventions to address these underlying mechanisms.
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in the regulation of various bodily functions. It is responsible for controlling the muscles of the digestive tract, including the esophagus and stomach. When the vagus nerve is not functioning properly, it can lead to a variety of gastrointestinal issues, including hiatal hernias.
A hiatal hernia occurs when the upper part of the stomach protrudes through the diaphragm into the chest cavity. This can result in symptoms such as heartburn, chest pain, and difficulty swallowing. While the exact cause of hiatal hernias is not fully understood, it is believed that a combination of factors, including weakened muscles and increased pressure on the abdomen, contribute to their development.
Potential Complications and Risks
While hiatal hernias, in themselves, may not pose severe threats to one’s health, they can lead to complications if left untreated. These include chronic heartburn, esophageal inflammation, and, in rare cases, the development of a paraesophageal hernia. Chronic heartburn, also known as gastroesophageal reflux disease (GERD), can cause damage to the lining of the esophagus over time, leading to a condition called Barrett’s esophagus, which increases the risk of esophageal cancer.
Esophageal inflammation, known as esophagitis, can result from the stomach acid flowing back into the esophagus due to the hiatal hernia. This can cause pain, difficulty swallowing, and even bleeding in severe cases. Paraesophageal hernias, although rare, occur when a portion of the stomach squeezes through the diaphragm alongside the esophagus. This can lead to a medical emergency if the hernia becomes trapped or twisted, cutting off blood supply to the stomach.
It is crucial for individuals with hiatal hernias to monitor their symptoms and seek medical attention if they experience any alarming or persistent signs. Early detection and appropriate management can help prevent complications and improve the overall quality of life for those affected.
Prevention and Management Strategies
Although hiatal hernias cannot always be prevented, certain lifestyle modifications can help reduce the risk and manage symptoms. Maintaining a healthy weight is important, as excess weight can put additional pressure on the abdomen and increase the likelihood of developing a hiatal hernia. Eating smaller and more frequent meals can also help prevent the stomach from becoming too full and pushing up through the diaphragm.
Avoiding trigger foods, such as spicy or fatty foods, caffeine, and citrus fruits, can help reduce the occurrence of acid reflux and heartburn. Excessive alcohol consumption should also be avoided, as it can relax the lower esophageal sphincter, allowing stomach acid to flow back into the esophagus.
Consulting with a healthcare professional for personalized advice is also recommended for effective management. They may recommend medications to reduce stomach acid production, such as proton pump inhibitors or H2 blockers. In some cases, surgery may be necessary to repair the hernia and prevent further complications.
Furthermore, stress management techniques, such as deep breathing exercises and meditation, can help regulate vagal function and reduce the risk of hiatal hernia development. Regular exercise, particularly activities that strengthen the abdominal muscles, can also provide support to the diaphragm and reduce the likelihood of herniation.
In conclusion, understanding the connection between the vagus nerve and hiatal hernia opens up new possibilities for medical treatment and management strategies. By addressing vagal function and considering its role in hiatal hernia development, healthcare professionals can provide more targeted interventions and improve outcomes for individuals with this condition.
Future Research Directions
While significant progress has been made in understanding the connection between the vagus nerve and hiatal hernia, several unanswered questions remain. Ongoing research aims to further explore the intricate mechanisms involved and uncover new avenues for diagnosis, prevention, and treatment.
One area of interest for future research is investigating how specific vagal dysfunctions may contribute to the development and progression of hiatal hernias. The vagus nerve, also known as the “wandering nerve,” plays a crucial role in regulating various bodily functions, including digestion and the movement of food through the gastrointestinal tract. Understanding how disruptions in vagal signaling may impact the structure and function of the hiatus, the opening in the diaphragm through which the esophagus passes, could provide valuable insights into the underlying causes of hiatal hernias.
Furthermore, researchers are eager to explore the complex interplay between genetic, environmental, and lifestyle factors in the development of hiatal hernias. While it is known that certain factors, such as obesity and smoking, can increase the risk of developing a hiatal hernia, the precise mechanisms by which these factors interact with genetic predispositions are not fully understood. Future studies may aim to unravel these intricate relationships, potentially leading to personalized approaches for intervention and prevention.
The Potential for New Treatment Approaches
As research progresses, the knowledge gained from studying the vagus nerve and hiatal hernia connection holds the potential for innovative treatment approaches. Targeting vagal signaling pathways and developing therapies that restore or enhance vagal function may offer novel avenues for managing hiatal hernias and related symptoms.
One potential treatment approach that researchers are exploring is the use of vagal nerve stimulation. This technique involves the implantation of a device that delivers electrical impulses to the vagus nerve, aiming to modulate its activity and potentially alleviate symptoms associated with hiatal hernias. Preliminary studies have shown promising results, with some patients experiencing a reduction in acid reflux and improvement in overall quality of life.
Additionally, researchers are investigating the role of lifestyle modifications in managing hiatal hernias. While surgery is often recommended for severe cases, lifestyle changes such as weight loss, dietary modifications, and avoiding trigger foods may help alleviate symptoms in milder cases. Understanding how these lifestyle factors interact with vagal function and the structural integrity of the hiatus could provide valuable insights into non-invasive treatment options.
In conclusion
The connection between the vagus nerve and hiatal hernia is a fascinating field of study that highlights the intricate interplay between our nervous system and overall health. While more research is needed to fully understand this connection, the existing knowledge provides valuable insights that can guide medical professionals in their approach to diagnosis, prevention, and management. If you suspect you have a hiatal hernia or are experiencing related symptoms, it is always advisable to consult with a healthcare professional for an accurate diagnosis and personalized guidance.
If you’re captivated by the critical role the vagus nerve plays in your health as discussed in this article, you’ll find the “My Vagus Nerve & Me Book” an invaluable resource. Dive deeper into the wonders of this complex system that orchestrates functions from heart rate to digestion, and discover practical ways to stimulate your vagus nerve for improved well-being. Whether you’re dealing with a hiatal hernia or simply seeking to enhance your overall health, this book is your guide to harnessing the power of one of the most essential nerves in your body. Don’t miss out on unlocking the secrets of your vagus nerve—Get My Vagus Nerve & Me eBook today and embark on a journey to better health.