Hiatal hernia is a medical condition that affects the upper part of the stomach. It occurs when the stomach pushes through the diaphragm, the muscle that separates the chest from the abdomen. This condition can lead to various symptoms, such as heartburn, acid reflux, and chest pain.Understanding Hiatal Hernia
Understanding Hiatal Hernia
Hiatal hernias are classified into two types: sliding hiatal hernia and paraesophageal hiatal hernia. Sliding hiatal hernia is the most common type and occurs when the junction between the stomach and the esophagus slides up into the chest. Paraesophageal hiatal hernia is less common but can be more serious, as it involves the stomach squeezing through the diaphragm next to the esophagus.
When it comes to understanding hiatal hernia, it is important to delve deeper into its definition, causes, symptoms, and diagnosis. By exploring these aspects, we can gain a comprehensive understanding of this condition and its impact on the human body.
Definition and Causes of Hiatal Hernia
A hiatal hernia is defined as the protrusion of the stomach through the diaphragm. The diaphragm is a large muscle that separates the chest cavity from the abdominal cavity. It plays a crucial role in the process of breathing by contracting and relaxing. However, weakened muscles in the diaphragm can lead to the development of hiatal hernia.
There are various factors that can contribute to the weakening of the diaphragm muscles and the subsequent occurrence of hiatal hernia. Increased pressure in the abdomen, such as during pregnancy or obesity, can put strain on the diaphragm and cause it to weaken. Additionally, age-related changes in the diaphragm can also make it more susceptible to herniation. Certain lifestyle factors, such as smoking and unhealthy eating habits, may further exacerbate the risk of developing hiatal hernia.
Symptoms and Diagnosis of Hiatal Hernia
The symptoms of hiatal hernia can vary from person to person. While some individuals may experience no symptoms at all, others may have frequent heartburn, difficulty swallowing, regurgitation, or chest pain. These symptoms can be attributed to the abnormal positioning of the stomach and the resulting disruption in the functioning of the esophagus.
Diagnosing hiatal hernia typically involves a series of tests and examinations conducted by medical professionals. One common diagnostic procedure is the barium swallow, where the patient drinks a liquid containing barium, which helps in visualizing the esophagus and stomach on X-rays. Another method is an upper endoscopy, where a flexible tube with a camera is inserted through the mouth to examine the esophagus and stomach. Additionally, esophageal manometry may be performed to measure the pressure and movement of the esophagus.
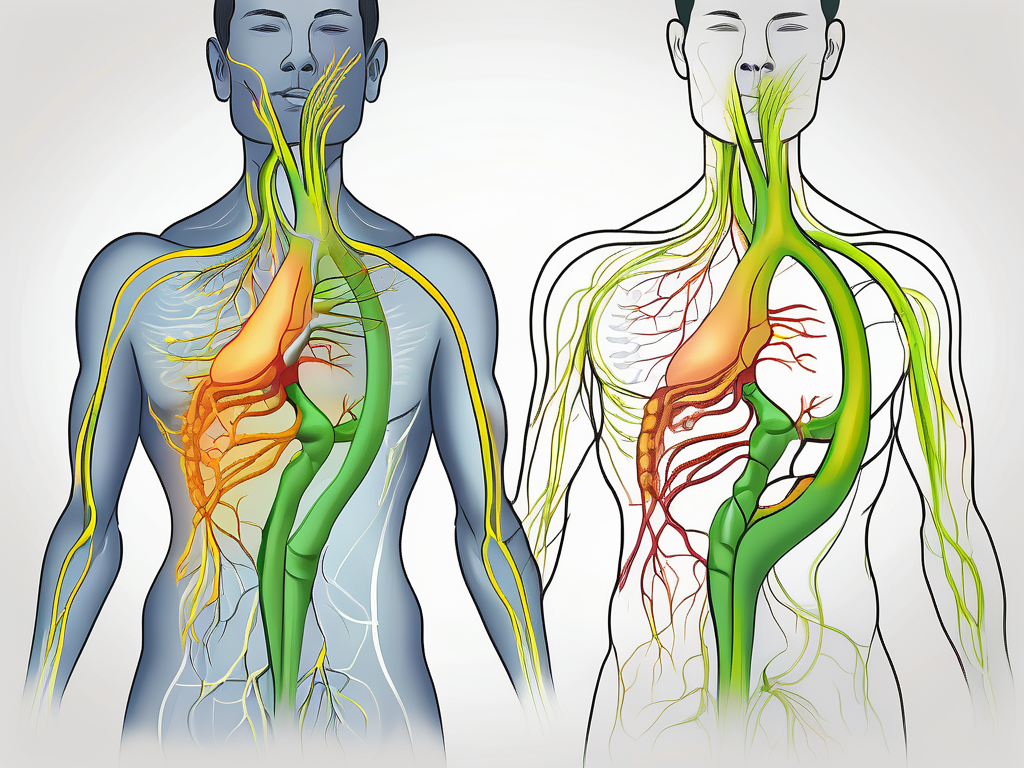
The Role of the Vagus Nerve in the Body
While understanding hiatal hernia, it is important to explore the role of the vagus nerve in the human body. The vagus nerve is one of the cranial nerves and is responsible for transmitting sensory and motor signals between the brain and various organs, including the stomach and esophagus.
When the vagus nerve functions properly, it helps regulate the movement and coordination of the digestive system. However, in cases of hiatal hernia, the abnormal positioning of the stomach can potentially affect the vagus nerve’s ability to transmit signals effectively. This disruption in communication between the brain and the digestive organs can contribute to the development of symptoms associated with hiatal hernia.
Understanding the intricate relationship between the vagus nerve and hiatal hernia can provide valuable insights into the underlying mechanisms of this condition. Further research and exploration in this area may lead to advancements in the diagnosis and treatment of hiatal hernia.
The Role of the Vagus Nerve in the Body
The vagus nerve, also known as the tenth cranial nerve, is a major component of the autonomic nervous system. It is responsible for regulating various bodily functions, including heart rate, respiration, and digestion.
But did you know that the vagus nerve does much more than just that? Let’s dive deeper into the anatomy and function of this fascinating nerve.
Anatomy and Function of the Vagus Nerve
The vagus nerve extends from the brainstem to various organs in the body, including the heart, lungs, stomach, and intestines. It is the longest cranial nerve and has multiple branches that innervate different areas.
One of the primary functions of the vagus nerve is to control the parasympathetic nervous system, which is responsible for rest and digest functions. It helps regulate heart rate, release digestive enzymes, and control the movement of food through the digestive tract.
But its influence doesn’t stop there. The vagus nerve also plays a role in other important bodily functions, such as regulating blood pressure, influencing mood and emotions, and even modulating inflammation.
The Vagus Nerve and the Digestive System
When it comes to the digestive system, the vagus nerve plays a crucial role in ensuring its proper functioning. It stimulates gastric acid secretion, promoting motility in the gastrointestinal tract, and coordinates the release of digestive enzymes.
Imagine a symphony orchestra, with each instrument playing its part to create a harmonious melody. Similarly, the vagus nerve orchestrates the digestive process, ensuring efficient digestion and absorption of nutrients.
Moreover, the vagus nerve also communicates with the gut microbiota, the vast community of microorganisms residing in our intestines. This bidirectional communication between the gut and the brain, known as the gut-brain axis, influences our mood, behavior, and overall well-being.
The Link Between Hiatal Hernia and the Vagus Nerve
Now, let’s explore an interesting connection between the vagus nerve and a common condition called hiatal hernia. A hiatal hernia occurs when a part of the stomach protrudes through the diaphragm into the chest cavity.
While the exact cause of hiatal hernia is not fully understood, it is believed that the vagus nerve may play a role in its development. The vagus nerve innervates the diaphragm and helps regulate its function. Dysfunction of the vagus nerve could potentially contribute to the weakening of the diaphragm, leading to the formation of a hiatal hernia.
Understanding the intricate relationship between the vagus nerve and hiatal hernia can provide valuable insights into potential treatment approaches and management strategies for this condition.
In conclusion, the vagus nerve is a remarkable part of our nervous system, with its reach extending far beyond its role in regulating heart rate, respiration, and digestion. Its influence on various bodily functions highlights its importance in maintaining overall health and well-being. Exploring the intricacies of the vagus nerve opens up new avenues for understanding and treating a wide range of conditions.
The Link Between Hiatal Hernia and the Vagus Nerve
Research suggests that there might be a connection between hiatal hernia and vagus nerve dysfunction. Hiatal hernia’s impact on the vagus nerve can contribute to the development or worsening of symptoms experienced by individuals with hiatal hernia.
Understanding the relationship between hiatal hernia and the vagus nerve can provide valuable insights into the management and treatment of these conditions.
How Hiatal Hernia Affects the Vagus Nerve
When the stomach pushes through the diaphragm, it can put pressure on the vagus nerve, affecting its function. This pressure can disrupt the transmission of nerve signals between the brain and the digestive system, leading to various digestive issues, such as acid reflux, bloating, and delayed gastric emptying.
The vagus nerve plays a crucial role in regulating the digestive system. It controls the movement of food through the esophagus, stomach, and intestines. When the vagus nerve is compressed or irritated by a hiatal hernia, its ability to coordinate these movements may be compromised.
Additionally, the vagus nerve is responsible for controlling the release of gastric acid and enzymes that aid in digestion. When the nerve’s function is disrupted, it can lead to an imbalance in the production of these substances, resulting in symptoms such as heartburn, indigestion, and difficulty swallowing.
The Impact of Vagus Nerve on Hiatal Hernia Symptoms
On the other hand, dysfunction of the vagus nerve can also contribute to the development of hiatal hernia symptoms. If the vagus nerve fails to regulate the movement of food through the digestive tract or control the release of gastric acid and enzymes, it can result in symptoms such as heartburn, indigestion, and difficulty swallowing.
Furthermore, the vagus nerve plays a vital role in maintaining the tone of the lower esophageal sphincter (LES), a muscular valve that prevents stomach acid from flowing back into the esophagus. If the vagus nerve is not functioning properly, the LES may weaken, leading to an increased risk of acid reflux and the development of hiatal hernia symptoms.
It is important to note that while there is a clear relationship between hiatal hernia and vagus nerve dysfunction, the exact mechanisms underlying this connection are still being studied. Further research is needed to fully understand the complex interplay between these two conditions.
Treatment Options for Hiatal Hernia and Vagus Nerve Issues
Managing hiatal hernia and vagus nerve dysfunction often involves a combination of lifestyle changes, medication, and, in some cases, surgical intervention.
Lifestyle modifications may include dietary changes, such as avoiding trigger foods that can exacerbate symptoms, maintaining a healthy weight, and practicing good posture to reduce pressure on the stomach and diaphragm.
Medications, such as proton pump inhibitors (PPIs) or H2 blockers, may be prescribed to reduce stomach acid production and alleviate symptoms of acid reflux. Additionally, prokinetic agents can be used to improve gastric motility and aid in the movement of food through the digestive system.
In severe cases or when conservative treatments fail to provide relief, surgical intervention may be necessary. Surgical options for hiatal hernia include laparoscopic repair, where the hernia is repositioned and the diaphragm is reinforced, or fundoplication, a procedure that strengthens the LES to prevent acid reflux.
It is essential to consult with a healthcare professional to determine the most appropriate treatment approach based on individual circumstances and the severity of symptoms.
In conclusion, the relationship between hiatal hernia and vagus nerve dysfunction is complex and multifaceted. Understanding how these conditions interact can guide healthcare professionals in providing effective management strategies for individuals experiencing symptoms related to hiatal hernia and vagus nerve dysfunction.
Hiatal hernia and vagus nerve-related issues have been the subject of ongoing research in the medical field. Scientists and healthcare professionals are continuously working to improve treatment options and gain a better understanding of the underlying mechanisms of these conditions.One area of research focuses on the development of new medications specifically designed to target the symptoms associated with hiatal hernia and vagus nerve dysfunction. These medications aim to provide more effective relief from acid reflux, heartburn, and other related symptoms. Researchers are exploring novel drug delivery systems and innovative approaches to enhance the efficacy of these medications.In addition to pharmaceutical advancements, researchers are also investigating the potential of non-invasive therapies for the management of hiatal hernia and vagus nerve-related issues. Techniques such as acupuncture, chiropractic adjustments, and nerve stimulation are being studied to determine their effectiveness in alleviating symptoms and improving overall quality of life for patients.Furthermore, there is growing interest in the role of diet and nutrition in the management of hiatal hernia and vagus nerve-related issues. Studies are being conducted to identify specific dietary modifications that may help reduce symptoms and prevent complications. For example, some research suggests that a low-acid diet, rich in alkaline foods, may be beneficial in reducing acid reflux and inflammation associated with hiatal hernia.The future of research in this field also includes exploring the potential of regenerative medicine and tissue engineering. Scientists are investigating the use of stem cells and biomaterials to repair and regenerate damaged tissues in the esophagus and diaphragm, which are commonly affected in hiatal hernia cases. This innovative approach holds promise for providing long-term solutions and reducing the need for invasive surgeries.In conclusion, the treatment options for hiatal hernia and vagus nerve-related issues are continually evolving as research progresses. Medical interventions, lifestyle changes, and natural remedies all play a role in managing these conditions. With ongoing research and advancements in the field, the future looks promising for improved treatment outcomes and enhanced quality of life for individuals affected by hiatal hernia and vagus nerve-related issues.
The Future of Research on Hiatal Hernia and the Vagus Nerve
As our understanding of the connection between hiatal hernia and the vagus nerve continues to evolve, ongoing research aims to explore potential breakthroughs and innovations that could improve treatment options for individuals with these conditions.
Hiatal hernia is a condition where a portion of the stomach protrudes through the diaphragm into the chest cavity. The vagus nerve, a major nerve that runs from the brain to the abdomen, plays a crucial role in regulating various bodily functions, including digestion. Understanding the relationship between hiatal hernia and vagus nerve dysfunction is essential for developing effective treatment strategies.
Current Research Trends
Current research focuses on further investigating the relationship between hiatal hernia and vagus nerve dysfunction. Studies aim to understand the mechanisms involved in the interaction between the hernia and the nerve and explore potential therapeutic targets.
Researchers are using advanced imaging techniques, such as magnetic resonance imaging (MRI) and computed tomography (CT), to visualize the structural changes in the diaphragm and the vagus nerve. By studying these changes, scientists hope to gain insights into the underlying causes of hiatal hernia and its impact on vagus nerve function.
In addition to structural changes, researchers are also investigating the role of inflammation in hiatal hernia and vagus nerve dysfunction. Inflammation is known to play a significant role in various diseases, and understanding its involvement in this condition may open up new avenues for treatment.
Advancements in medical technology continue to refine surgical techniques and interventions. Minimally invasive procedures, such as laparoscopic surgery, have become more common in the treatment of hiatal hernia. These procedures offer shorter recovery times and reduced post-operative complications.
Potential Breakthroughs and Innovations
It is anticipated that future breakthroughs in the field of hiatal hernia and vagus nerve research could lead to improved diagnostic methods, personalized treatment approaches, and novel interventions targeting the nerve dysfunction.
One potential breakthrough is the development of biomarkers that can identify individuals at a higher risk of developing hiatal hernia or experiencing vagus nerve dysfunction. These biomarkers could help healthcare professionals intervene earlier, potentially preventing the progression of the condition or reducing its impact on the patient’s quality of life.
Another area of innovation lies in the development of targeted therapies that specifically address the underlying causes of vagus nerve dysfunction in hiatal hernia. By targeting the mechanisms responsible for nerve dysfunction, researchers hope to develop treatments that can restore normal nerve function and alleviate symptoms.
Furthermore, advancements in genetic research may uncover genetic factors that predispose individuals to hiatal hernia and vagus nerve dysfunction. Identifying these genetic markers could help identify individuals at risk and allow for personalized treatment plans tailored to their specific needs.
By better understanding the intricate relationship between hiatal hernia and the vagus nerve, healthcare professionals may be able to provide more effective and tailored management strategies for individuals affected by hiatal hernia and vagus nerve-related symptoms.
Individuals experiencing symptoms related to hiatal hernia or vagus nerve dysfunction should consult with a healthcare professional for a proper diagnosis and appropriate management plan. Early intervention and personalized treatment can significantly improve outcomes and quality of life for those affected by these conditions.
If you’re fascinated by the role of the vagus nerve in conditions like hiatal hernia and want to delve deeper into the wonders of this crucial nerve, “My Vagus Nerve & Me Book” is your essential guide. Discover the secrets of one of the most sophisticated systems in the human body and learn how it influences everything from your digestion to your mental health. Uncover natural and artificial ways to stimulate your vagus nerve for improved well-being. Take the first step towards harnessing the power of your vagus nerve by getting your copy of the eBook today. Get My Vagus Nerve & Me eBook and embark on a journey to better health.