Gastroesophageal reflux disease (GERD) is a common condition that affects millions of people worldwide. It is a chronic digestive disorder characterized by the frequent flow of stomach acid into the esophagus, causing discomfort and potential damage to the lining of the esophagus. While GERD is primarily attributed to dysfunction of the lower esophageal sphincter (LES), recent research has shed light on another potential player in this condition: the vagus nerve.
Understanding GERD: Causes and Symptoms
GERD, or gastroesophageal reflux disease, is a condition that affects the digestive system. It is often caused by a weakened or malfunctioning lower esophageal sphincter (LES), the muscular ring that separates the esophagus from the stomach. When the LES fails to close properly, it allows stomach acid to flow back into the esophagus, resulting in the characteristic symptoms of GERD.
GERD is a common condition that affects millions of people worldwide. It can cause discomfort and disrupt daily life. Understanding the causes and symptoms of GERD is crucial for proper diagnosis and management.
The Role of the Lower Esophageal Sphincter in GERD
The lower esophageal sphincter (LES) plays a crucial role in preventing the backflow of stomach contents into the esophagus. It acts as a gateway, opening to allow food and liquid to pass into the stomach and closing to prevent the upward movement of stomach acid.
In individuals with GERD, the LES may be abnormally relaxed or weak, allowing stomach acid to escape upwards and irritate the esophageal lining. This dysfunction of the LES is a key factor in the development of GERD.
Various factors can contribute to the weakening of the LES. These include obesity, pregnancy, smoking, certain medications, and certain medical conditions such as hiatal hernia. Understanding these risk factors can help individuals take preventive measures to reduce the likelihood of developing GERD.
Common Symptoms of GERD
Symptoms of GERD can vary from person to person, but certain signs are commonly experienced by those affected. Heartburn, a burning sensation in the chest or throat, is one of the hallmark symptoms of GERD. It can be triggered by certain foods, lying down after a meal, or bending over.
Regurgitation is another common symptom of GERD. It occurs when acid or food comes back up into the mouth, leaving a sour or bitter taste. This can be uncomfortable and may lead to bad breath.
Other symptoms of GERD may include difficulty swallowing, chronic cough, hoarseness, and chest pain. These symptoms can vary in severity and frequency, depending on the individual. It is important to note that not everyone with GERD experiences all of these symptoms.
If you suspect that you may have GERD, it is important to consult with a healthcare professional for an accurate diagnosis. They can provide guidance on lifestyle modifications, medications, and other treatment options to help manage your symptoms and improve your quality of life.
The Vagus Nerve: An Overview
The vagus nerve, also known as the tenth cranial nerve, is one of the longest and most complex nerves in the body. It plays a vital role in the autonomic nervous system, which regulates various automatic bodily functions, including digestion, heart rate, and breathing.
But what exactly is the vagus nerve and how does it function? Let’s delve deeper into its anatomy and functions to gain a better understanding.
Anatomy and Functions of the Vagus Nerve
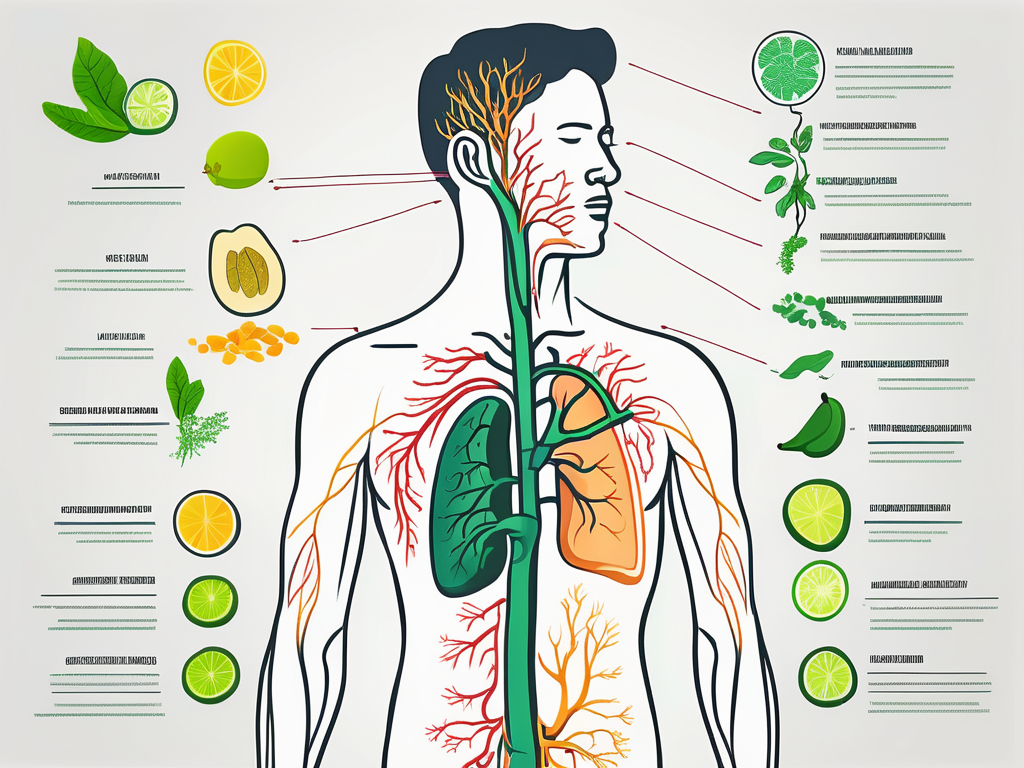
The vagus nerve originates in the brainstem, specifically the medulla oblongata, and extends down through the neck, chest, and abdomen. It is composed of both sensory and motor fibers, allowing it to transmit signals to and from various organs in the body.
Branching out like a complex network, the vagus nerve innervates multiple organs, including the heart, lungs, stomach, and intestines. These connections enable the nerve to carry signals from these organs back to the brain, allowing the body to maintain homeostasis and respond to internal and external stimuli.
One of the primary functions of the vagus nerve is to regulate the parasympathetic nervous system, which is responsible for the body’s “rest and digest” response. This means that the vagus nerve helps to promote relaxation, conserve energy, and facilitate the body’s recovery and repair processes.
The Vagus Nerve’s Role in Digestion
In the context of digestion, the vagus nerve plays a crucial role in coordinating the movements of the digestive tract and the release of digestive juices. It stimulates the production of stomach acid, aids in food propulsion through the stomach and intestines, and triggers the release of enzymes necessary for digestion and nutrient absorption.
When we eat, the vagus nerve sends signals to the brain to initiate the release of digestive enzymes and increase blood flow to the stomach and intestines. This helps to break down food into smaller particles, absorb nutrients, and eliminate waste products effectively.
Furthermore, the vagus nerve communicates with the enteric nervous system, a complex network of neurons embedded in the walls of the digestive tract. This communication allows for the coordination of peristalsis, the rhythmic contractions that propel food through the digestive system.
Interestingly, the vagus nerve also plays a role in the gut-brain axis, a bidirectional communication system between the gut and the brain. It helps to regulate mood, emotions, and even cognitive functions, highlighting the intricate connection between the gut and the brain.
In conclusion, the vagus nerve is a remarkable component of the autonomic nervous system, with its extensive reach and multifaceted functions. From regulating digestion to influencing our emotional well-being, this nerve serves as a vital link between our bodily functions and our brain. Understanding its anatomy and functions allows us to appreciate the intricate mechanisms that enable our bodies to function harmoniously.
The Link Between the Vagus Nerve and GERD
Recent studies have suggested a potential link between vagus nerve dysfunction and GERD. The vagus nerve, also known as the tenth cranial nerve, is a crucial component of the parasympathetic nervous system. It plays a vital role in regulating various bodily functions, including digestion. The vagus nerve controls the relaxation and contraction of the lower esophageal sphincter (LES), influencing its ability to properly perform its barrier function.
The LES, located at the junction between the esophagus and the stomach, acts as a valve that opens to allow food to enter the stomach and closes to prevent stomach contents from flowing back into the esophagus. Dysfunction or impairment of the vagus nerve’s signaling to the LES may contribute to LES malfunction, leading to GERD symptoms.
How the Vagus Nerve Influences GERD
When the vagus nerve is functioning normally, it sends signals to the LES, prompting it to relax during swallowing to allow food to pass from the esophagus into the stomach. This relaxation of the LES is essential for smooth food transit and proper digestion. After food has entered the stomach, the LES should tighten to prevent stomach contents, including acid, from flowing back into the esophagus.
However, in individuals with vagus nerve dysfunction, this process may be disrupted. If the vagus nerve fails to send appropriate signals or if the LES fails to respond, acid reflux and GERD symptoms may occur. The malfunctioning LES allows stomach acid to regurgitate into the esophagus, leading to heartburn, chest pain, and other discomforting symptoms associated with GERD.
Vagus Nerve Dysfunction and GERD
While the exact relationship between vagus nerve dysfunction and GERD is still being explored, several factors have been proposed to contribute to this connection. One possible factor is impaired communication between the vagus nerve and the LES. This breakdown in communication may result from nerve damage, inflammation, or other underlying conditions.
Additionally, reduced vagal tone, which refers to a decrease in the activity of the vagus nerve, has been suggested as a potential mechanism. A decrease in vagal tone may affect the LES’s ability to relax and contract appropriately, leading to GERD symptoms.
Furthermore, alterations in neural pathways that regulate LES function could also play a role in vagus nerve dysfunction and GERD. The complex network of nerves involved in controlling the LES may be disrupted, causing abnormal LES behavior and contributing to the development of GERD.
It is important to note that further research is needed to fully understand the mechanisms behind vagus nerve dysfunction in GERD. Scientists and medical professionals continue to investigate this intriguing link to develop more effective treatments and interventions for individuals with GERD.
Potential Treatments Targeting the Vagus Nerve
As the understanding of the role of the vagus nerve in GERD grows, potential treatments targeting this nerve are being explored. One such treatment is vagus nerve stimulation therapy.
The vagus nerve, also known as the “wandering nerve,” is a crucial part of the autonomic nervous system. It plays a vital role in regulating various bodily functions, including digestion, heart rate, and respiratory function. In the context of GERD, the vagus nerve is responsible for controlling the movement of food through the digestive tract and the production of stomach acid.
Vagus nerve stimulation involves delivering electrical impulses to the vagus nerve using a small device implanted under the skin. This therapy aims to modulate the activity of the vagus nerve and improve its function, potentially reducing GERD symptoms. The electrical impulses can be adjusted to target specific areas of the nerve, allowing for personalized treatment.
While still in its early stages, vagus nerve stimulation therapy shows promise as a potential treatment option for individuals with severe or refractory GERD. Clinical trials are underway to evaluate its effectiveness and safety in a larger population. If successful, this therapy could provide a non-invasive alternative to traditional GERD treatments, such as medication or surgery.
Lifestyle Changes to Improve Vagus Nerve Function
In addition to medical treatments, lifestyle modifications can also play a role in improving vagus nerve function and managing GERD. These lifestyle changes may include maintaining a healthy weight, avoiding trigger foods that can exacerbate GERD symptoms, eating smaller meals, avoiding lying down immediately after meals, and elevating the head of the bed while sleeping.
Obesity has been linked to increased GERD symptoms, as excess weight can put pressure on the stomach and weaken the lower esophageal sphincter, allowing stomach acid to flow back into the esophagus. By maintaining a healthy weight through regular exercise and a balanced diet, individuals can reduce the strain on their digestive system and potentially alleviate GERD symptoms.
Trigger foods, such as spicy or acidic foods, caffeine, alcohol, and fatty foods, can irritate the stomach and trigger excessive production of stomach acid. Avoiding these trigger foods can help minimize GERD symptoms and reduce the frequency of acid reflux episodes.
Eating smaller meals throughout the day, rather than consuming large meals, can also aid in digestion and prevent excessive pressure on the stomach. This can help reduce the likelihood of acid reflux and alleviate GERD symptoms.
Furthermore, avoiding lying down immediately after meals allows gravity to assist in keeping stomach acid in the stomach. It is recommended to wait at least two to three hours after eating before lying down or going to bed.
Elevating the head of the bed by placing blocks or using a wedge pillow can help prevent stomach acid from flowing back into the esophagus during sleep. This slight elevation helps maintain the proper alignment of the esophagus and stomach, reducing the risk of acid reflux and nighttime GERD symptoms.
However, it is important to consult with a healthcare provider before making any significant dietary or lifestyle changes. They can provide personalized recommendations based on individual health conditions and needs.
Future Research Directions in GERD and Vagus Nerve Connection
While there is growing evidence of a connection between the vagus nerve and GERD, more research is needed to fully unravel the complexity of this relationship. Ongoing studies aim to further elucidate the mechanisms by which the vagus nerve influences LES function and explore potential therapeutic interventions that leverage this connection.
One area of future research in the field of GERD and the vagus nerve is focused on understanding the role of inflammation. Inflammation has been implicated in the development and progression of GERD, and researchers are investigating how the vagus nerve may modulate the inflammatory response in the esophagus. By gaining a better understanding of this process, scientists hope to identify new targets for intervention and develop more effective treatments for GERD.
Another avenue of exploration is the impact of lifestyle factors on the vagus nerve and GERD. It is well-known that certain lifestyle choices, such as diet and stress levels, can contribute to the development and exacerbation of GERD symptoms. Researchers are interested in understanding how these factors may influence the vagus nerve and its role in regulating LES function. This knowledge could potentially lead to personalized treatment approaches that take into account an individual’s lifestyle habits.
Potential for New GERD Treatments
Increased understanding of the vagus nerve’s involvement in GERD may pave the way for the development of innovative treatments targeting this neural pathway. By targeting vagus nerve dysfunction, researchers hope to improve LES function, reduce acid reflux, and alleviate the symptoms and complications associated with GERD. One potential treatment approach being explored is vagus nerve stimulation, which involves the use of electrical impulses to modulate nerve activity. Preliminary studies have shown promising results, but further research is needed to determine its safety and efficacy.
In addition to vagus nerve stimulation, other potential treatment options being investigated include pharmacological interventions that specifically target the vagus nerve or its downstream signaling pathways. By selectively modulating the activity of the vagus nerve, researchers aim to restore the balance between LES relaxation and contraction, thus reducing the occurrence of acid reflux episodes.
The Need for Further Understanding of the Vagus Nerve’s Role in GERD
While the vagus nerve’s involvement in GERD is an active area of investigation, it should be noted that the understanding of this connection is still evolving. Researchers are constantly uncovering new insights and challenging existing theories, highlighting the need for continued exploration.
One aspect that requires further investigation is the potential bidirectional relationship between GERD and the vagus nerve. While it is clear that vagus nerve dysfunction can contribute to the development of GERD, it is not yet fully understood how GERD may in turn affect vagus nerve function. By unraveling this complex interplay, researchers hope to gain a more comprehensive understanding of the pathophysiology of GERD and identify novel therapeutic targets.
Furthermore, the impact of individual variability in vagus nerve function on GERD remains an important area of research. It is well-known that individuals differ in their susceptibility to GERD and response to treatment. By studying the factors that influence vagus nerve function, such as genetic variations or environmental factors, researchers aim to identify biomarkers that can help predict an individual’s risk of developing GERD and guide personalized treatment approaches.
In conclusion, the connection between the vagus nerve and GERD is a complex and multifaceted topic that requires further investigation. Ongoing research aims to uncover the underlying mechanisms, explore new treatment options, and improve our understanding of the interplay between the vagus nerve and GERD. Individuals experiencing GERD symptoms should consult with a healthcare provider for a proper diagnosis and appropriate management strategies.
If you’re fascinated by the critical role the vagus nerve plays in conditions like GERD and want to delve deeper into its functions and impact on overall health, “My Vagus Nerve & Me Book” is an essential resource. Discover the wonders of this intricate system that orchestrates vital bodily functions, from digestion to heart rate regulation. Learn practical ways to stimulate your vagus nerve for improved well-being. Ready to embark on a journey of understanding and harnessing the power of your vagus nerve? Get My Vagus Nerve & Me eBook today and take the first step towards optimal health.