Vagus Nerve Stimulation (VNS) has emerged as a promising treatment option for individuals with seizures. This non-invasive therapy works by delivering electrical impulses to the vagus nerve, which is responsible for regulating various bodily functions. While VNS is not a cure for epilepsy or other seizure disorders, it can significantly reduce seizure frequency and intensity, leading to an improved quality of life for patients. In this article, we will explore the underlying science of VNS, its benefits, risks, and potential future applications.
Understanding the Vagus Nerve and Its Functions
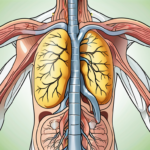
The vagus nerve is one of the cranial nerves and is the longest nerve in the body. It connects the brain to various organs, including the heart, lungs, and digestive system. The vagus nerve plays a crucial role in regulating many bodily functions, such as heart rate, breathing, digestion, and even mood. It acts as a communication highway between the brain and the rest of the body, allowing for the exchange of vital information.
The vagus nerve, also known as the tenth cranial nerve or the wandering nerve, is a fascinating and complex part of the human body. With its extensive reach and numerous functions, it is often referred to as the “commander-in-chief” of the parasympathetic nervous system. This nerve, originating from the medulla oblongata in the brainstem, extends down through the neck and into the chest and abdomen, branching out to innervate various organs and tissues.
The Role of the Vagus Nerve in the Body
The vagus nerve is responsible for transmitting signals between the brain and different organs. It helps regulate heart rate, blood pressure, and respiratory rate. This nerve plays a vital role in maintaining homeostasis, ensuring that the body’s internal environment remains stable and balanced. It achieves this by continuously monitoring and adjusting various physiological processes.
When it comes to heart rate, the vagus nerve acts as a natural pacemaker, slowing down the heart’s rhythm and reducing the force of contractions. This parasympathetic control helps to maintain a steady heart rate, preventing it from becoming too fast or irregular. Similarly, the vagus nerve influences blood pressure by dilating blood vessels and reducing vascular resistance, ultimately promoting a healthy blood flow throughout the body.
In terms of respiration, the vagus nerve plays a crucial role in regulating the rate and depth of breathing. It sends signals to the diaphragm and other respiratory muscles, ensuring their coordinated contraction and relaxation. By modulating the activity of these muscles, the vagus nerve helps maintain a balanced exchange of oxygen and carbon dioxide, essential for the body’s overall functioning.
Furthermore, the vagus nerve is involved in controlling digestion and gastrointestinal motility. It stimulates the production of digestive enzymes, enhances nutrient absorption, and promotes the rhythmic contractions of the digestive tract. This intricate network of signals ensures that food is properly broken down and nutrients are efficiently absorbed, supporting overall digestive health.
Interestingly, the vagus nerve’s influence extends beyond the physical aspects of the body. It also plays a role in emotional regulation and mental well-being. Studies have shown that stimulating the vagus nerve can have a positive impact on mood, reducing symptoms of anxiety and depression. This connection between the vagus nerve and emotional health highlights the intricate interplay between the mind and the body.
The Connection Between the Vagus Nerve and Seizures
Researchers have discovered a strong link between the vagus nerve and seizures. Abnormal electrical activity in the brain can trigger seizures, and the vagus nerve acts as a pathway for these electrical signals. By stimulating the vagus nerve, it is possible to modulate these abnormal electrical patterns and reduce the likelihood of seizures occurring.
This discovery has led to the development of a medical treatment known as vagus nerve stimulation (VNS). In this procedure, a small device is implanted in the body, typically in the chest area, and connected to the vagus nerve. The device delivers mild electrical impulses to the nerve, helping to regulate its activity and prevent the occurrence of seizures.
VNS has shown promising results in reducing seizure frequency and severity in individuals with epilepsy. It is particularly beneficial for those who do not respond well to traditional anti-seizure medications. By directly targeting the vagus nerve, this treatment offers a new avenue for managing epilepsy and improving the quality of life for those affected by this neurological disorder.
As our understanding of the vagus nerve continues to grow, so does the potential for harnessing its power in medical treatments. Researchers are exploring various applications of vagus nerve stimulation, not only for epilepsy but also for other conditions such as depression, chronic pain, and inflammatory disorders. The vagus nerve’s intricate functions and its connection to various bodily systems make it a fascinating area of study, offering hope for innovative therapies in the future.
The Science Behind Vagus Nerve Stimulation
Vagus Nerve Stimulation (VNS) is a well-established procedure that has been used for many years to help manage seizures in individuals with epilepsy. It involves the implantation of a small device, known as a vagus nerve stimulator, under the skin. This device is connected to the vagus nerve in the neck and delivers regular electrical impulses to the nerve. These electrical signals help regulate the brain’s electrical activity, reducing the chance of seizures.
The vagus nerve is one of the longest nerves in the body, extending from the brainstem down to the abdomen. It plays a crucial role in the regulation of various bodily functions, including heart rate, digestion, and even mood. By stimulating the vagus nerve, VNS can have a profound impact on the brain’s functioning and overall well-being.
The Process of Vagus Nerve Stimulation
The implantation of a vagus nerve stimulator typically requires a minor surgical procedure that can be performed on an outpatient basis. The procedure is conducted under local anesthesia, ensuring minimal discomfort for the patient. A small incision is made in the neck, and the device is carefully placed near the vagus nerve.
Once the stimulator is in position, it is connected to the nerve and programmed to deliver electrical impulses at regular intervals. The stimulation parameters can be adjusted by a healthcare professional to optimize seizure control for each individual. This personalized approach ensures that the therapy is tailored to the specific needs of the patient, maximizing its effectiveness.
After the procedure, patients are usually able to resume their normal activities within a short period. The device is designed to be discreet and comfortable, allowing individuals to go about their daily lives without any significant disruptions.
How Vagus Nerve Stimulation Affects the Brain
While the exact mechanisms of VNS are not fully understood, researchers have made significant progress in unraveling the complex relationship between the vagus nerve and the brain. It is believed that the electrical stimulation of the vagus nerve has a modulatory effect on the brain’s electrical activity.
The electrical impulses generated by the vagus nerve stimulator travel up the vagus nerve to the brain, where they stimulate specific areas involved in seizure control. These areas include the thalamus, hippocampus, and prefrontal cortex, which play critical roles in regulating the brain’s electrical patterns.
By modulating these abnormal electrical patterns, VNS helps restore balance and stability to the brain, reducing the frequency and intensity of seizures. This can have a profound impact on the quality of life for individuals living with epilepsy, allowing them to better manage their condition and engage in daily activities with greater confidence.
Furthermore, recent research suggests that VNS may have additional benefits beyond seizure control. Studies have shown that VNS can improve mood and cognitive function in some individuals, offering a potential avenue for treating conditions such as depression and memory disorders.
The field of Vagus Nerve Stimulation continues to evolve, with ongoing research and technological advancements aimed at improving outcomes and expanding its applications. As our understanding of the brain and the vagus nerve deepens, we can expect further advancements in this exciting field, bringing hope and relief to individuals affected by epilepsy and other neurological conditions.
The Benefits of Vagus Nerve Stimulation for Seizure Control
Reduction in Seizure Frequency
One of the most significant benefits of Vagus Nerve Stimulation (VNS) is its ability to reduce the frequency of seizures. Clinical studies have shown that VNS can lead to a substantial decrease in seizure frequency in individuals with epilepsy. This groundbreaking therapy works by delivering electrical impulses to the vagus nerve, which is responsible for regulating various bodily functions, including seizure activity. By stimulating the vagus nerve, VNS helps to restore the balance of electrical signals in the brain, thereby reducing the occurrence of seizures.
While the results may vary from person to person, many patients experience a significant improvement in seizure control after undergoing VNS therapy. The reduction in seizure frequency can greatly enhance the patient’s quality of life, allowing them to engage in daily activities with greater confidence and independence. With fewer seizures to contend with, individuals with epilepsy can experience a sense of freedom and relief, knowing that their condition is being effectively managed.
Improvement in Seizure Severity
Aside from reducing seizure frequency, VNS has also been shown to improve the intensity and duration of seizures. For individuals who experience severe or prolonged seizures, this can make a considerable difference in their overall well-being. By modulating the brain’s electrical activity, VNS can help reduce the severity and duration of seizures, minimizing their impact on the individual’s daily life.
When a seizure occurs, it can be a frightening and disruptive experience for both the individual and those around them. The physical and emotional toll of a severe seizure can be overwhelming, often leading to feelings of anxiety and fear. However, with VNS therapy, the intensity and duration of seizures can be significantly reduced, providing individuals with a greater sense of control and stability. This improvement in seizure severity can have a profound impact on the individual’s overall quality of life, allowing them to engage in activities and pursue their goals with greater confidence and peace of mind.
Furthermore, the reduction in seizure severity can also lead to a decrease in the need for emergency medical interventions. Severe seizures often require immediate medical attention, which can be both physically and emotionally draining for the individual and their loved ones. By minimizing the severity of seizures, VNS therapy can help reduce the frequency of emergency situations, allowing individuals to feel more secure and less reliant on external assistance.
In conclusion, Vagus Nerve Stimulation offers numerous benefits for individuals with epilepsy, including a reduction in seizure frequency and an improvement in seizure severity. By harnessing the power of electrical impulses to modulate the brain’s activity, VNS provides a promising avenue for managing seizures and enhancing the overall well-being of individuals with epilepsy. With ongoing research and advancements in technology, VNS continues to evolve as a valuable therapeutic option, offering hope and improved quality of life for those living with epilepsy.
Risks and Considerations of Vagus Nerve Stimulation
Vagus Nerve Stimulation (VNS) is a medical procedure that carries potential risks and side effects that should be carefully considered. While it is a generally safe procedure, it is important to be aware of the possible complications that may arise.
Potential Side Effects of Vagus Nerve Stimulation
Common side effects of VNS may include voice changes, cough, throat pain, or hoarseness. These side effects are usually temporary and tend to improve over time as the body adjusts to the stimulation. It is important to note that these side effects vary in severity and may not occur in every individual who undergoes VNS.
In addition to the common side effects, some individuals may experience temporary discomfort or pain at the implantation site. This discomfort is typically managed with pain medication and subsides as the body heals. It is crucial to follow the post-operative instructions provided by the healthcare provider to ensure proper healing and minimize any potential complications.
It is important to note that severe complications associated with VNS are rare. However, as with any medical procedure, there is a small risk of infection, bleeding, or damage to surrounding structures. These risks are minimized through careful surgical technique and proper post-operative care.
Furthermore, it is essential to consider the potential impact of VNS on daily activities. The device, which is implanted under the skin in the chest area, may cause slight discomfort or irritation during physical activities such as exercising or sleeping. However, most individuals adapt to these sensations and find ways to manage them effectively.
Despite the potential side effects and risks, it is crucial to remember that VNS has been proven to be an effective treatment option for individuals who have not responded well to other seizure control methods. The benefits of VNS often outweigh the risks, especially for those who have been living with uncontrolled seizures and are seeking alternative solutions.
Who Should Consider Vagus Nerve Stimulation?
Vagus Nerve Stimulation is typically considered an option for individuals who have not achieved adequate seizure control with medication and other conventional treatments. It is important for individuals to consult with their healthcare provider, particularly a neurologist specializing in epilepsy, to determine if VNS is a suitable treatment option for them.
The decision to undergo VNS should involve a thorough evaluation of the potential benefits, risks, and individual needs. The healthcare provider will consider various factors, such as the frequency and severity of seizures, the impact of seizures on daily life, and the individual’s overall health. Additionally, they will review the individual’s medical history and any previous treatments attempted.
It is important to have realistic expectations when considering VNS. While it can significantly reduce seizure frequency and severity in many individuals, it may not eliminate seizures entirely. The goal of VNS is to improve quality of life by reducing the impact of seizures and enabling individuals to engage in daily activities more confidently.
In conclusion, Vagus Nerve Stimulation is a potential treatment option for individuals with epilepsy who have not responded well to other seizure control methods. While it carries potential risks and side effects, the benefits of VNS often outweigh these concerns. It is crucial to consult with a healthcare provider to determine if VNS is a suitable treatment option and to have a thorough understanding of the potential risks and benefits before making a decision.
The Future of Vagus Nerve Stimulation in Seizure Treatment
Ongoing Research and Developments
Vagus Nerve Stimulation (VNS) continues to be an active area of research, with ongoing studies aiming to further understand its mechanisms and improve its effectiveness. Researchers are exploring new techniques and technologies to enhance VNS therapy, such as closed-loop systems that can adapt the stimulation parameters based on individual needs. By developing more personalized approaches, researchers hope to optimize seizure control and minimize side effects.
One area of research focuses on identifying the optimal stimulation parameters for VNS therapy. Studies are investigating the effects of different stimulation frequencies, pulse widths, and amplitudes on seizure control. Researchers are also exploring the potential benefits of varying the timing and duration of VNS therapy sessions.
Another avenue of research involves understanding the underlying mechanisms of VNS therapy. Scientists are investigating how VNS affects neural circuits and neurotransmitter systems involved in seizure generation and propagation. By gaining a deeper understanding of these mechanisms, researchers hope to develop more targeted and effective therapies.
Furthermore, researchers are exploring the use of VNS in combination with other treatment modalities. Studies are investigating the potential synergistic effects of VNS with antiepileptic drugs, ketogenic diet, and neurofeedback. By combining different therapies, researchers aim to enhance seizure control and improve overall quality of life for individuals with epilepsy.
The Potential of Vagus Nerve Stimulation Beyond Seizure Control
While VNS is primarily used for seizure control, studies have suggested potential benefits beyond epilepsy management. Research has shown that VNS may have a positive impact on other neurological conditions, including depression and chronic pain. For individuals with treatment-resistant depression, VNS therapy has been shown to improve mood and reduce depressive symptoms. Additionally, VNS has demonstrated promising results in alleviating chronic pain, offering a potential alternative for individuals who have not responded well to conventional pain management strategies.
These findings pave the way for exploring the wider applications of VNS therapy and its potential to improve the lives of individuals with various medical conditions. Ongoing research is investigating the mechanisms underlying the effects of VNS on mood regulation and pain perception. By unraveling these mechanisms, researchers hope to develop targeted therapies for depression and chronic pain that can provide long-lasting relief.
In conclusion, Vagus Nerve Stimulation offers a significant step forward in seizure control and management. While it may not be suitable for everyone, this non-invasive therapy has shown promising results in reducing seizure frequency and improving seizure severity. It is an important treatment option to consider for individuals who have not achieved satisfactory seizure control with other methods. If you or a loved one is living with seizures, consulting with a healthcare professional, such as a neurologist, is crucial to explore the potential benefits and risks of Vagus Nerve Stimulation.
If you’re fascinated by the role of the vagus nerve in seizure control and curious about its broader impact on your health, “My Vagus Nerve & Me Book” is the perfect resource to deepen your understanding. Discover the secrets of this remarkable nerve that orchestrates your body’s most vital functions, from heart rate and digestion to your immune system and mental health. Learn how to harness its power through natural and artificial stimulation to enhance your well-being. Ready to embark on a journey of discovery about one of the most sophisticated systems in your body? Get My Vagus Nerve & Me eBook today and unlock the full potential of your vagus nerve!